Abstract
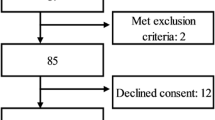
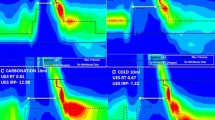
Recent studies have shown an association between alterations in laryngopharyngeal mechanosensitivity (LPMS) and dysphagia, obstructive sleep apnea, and chronic cough hypersensitivity syndrome. A previous reliability study of a new laryngopharyngeal endoscopic esthesiometer and rangefinder (LPEER) showed high intra- and inter-rater reliability; however, its accuracy has not been tested. We performed an accuracy study of the LPEER in a prospectively and consecutively recruited cohort of 118 patients at two tertiary care university hospitals. Most of the patients were suffering from dysphagia, and all of them underwent a standard clinical evaluation and fiberoptic endoscopic evaluation of swallowing with sensory testing (FEESST) using a new sensory testing protocol. The sensory test included determinations of the laryngeal adductor reflex threshold (LART), the cough reflex threshold (CRT) and the gag reflex threshold (GRT). Abnormalities on these reflex thresholds were evaluated for associations with major alterations in swallowing safety (pharyngeal residues, penetration, and aspiration). We evaluated the discriminative capacity of the LPMS test using ROC curves and the area under the curve (AUC–ROC) and its relationship with the eight-point penetration–aspiration scale (PAS) using the Spearman’s ρ correlation coefficient (SCC). We found a positive correlation between the PAS and LART (SCC 0.47; P < 0.001), CRT (SCC 0.46; P < 0.001) and GRT (SCC 0.34; P = 0.002). The AUC–ROC values for detecting a PAS ≥7 were as follows: LART, 0.83 (P < 0.0001); CRT, 0.79 (P < 0.0001); GRT, 0.72 (P < 0.0001). In this study, the LPEER showed good accuracy for evaluating LPMS. These results justify further validation studies in independent populations.


Similar content being viewed by others
References
Aviv JE, Kim T, Sacco RL, Kaplan S, Goodhart K, Diamond B, Close LG. FEESST: a new bedside endoscopic test of the motor and sensory components of swallowing. Ann Otol Rhinol Laryngol. 1998;107(5 Pt 1):378–87.
Setzen M, Cohen MA, Mattucci KF, Perlman PW, Ditkoff MK. Laryngopharyngeal sensory deficits as a predictor of aspiration. Otolaryngol Head Neck Surg. 2001;124(6):622–4.
Aviv JE, Sacco RL, Mohr JP, Thompson JL, Levin B, Sunshine S, Thomson J, Close LG. Laryngopharyngeal sensory testing with modified barium swallow as predictors of aspiration pneumonia after stroke. Laryngoscope. 1997;107(9):1254–60.
Clayton NA, Carnaby-Mann GD, Peters MJ, Ing AJ. The effect of chronic obstructive pulmonary disease on laryngopharyngeal sensitivity. Ear Nose Throat J. 2012;91(9):370, 372, 374 passim.
Aviv JE, Spitzer J, Cohen M, Ma G, Belafsky P, Close LG. Laryngeal adductor reflex and pharyngeal squeeze as predictors of laryngeal penetration and aspiration. Laryngoscope. 2002;112(2):338–41.
Dedhia RC, Rosen CA, Soose RJ. What is the role of the larynx in adult obstructive sleep apnea? Laryngoscope. 2014;124(4):1029–34.
Ludlow CL. Central nervous system control of interactions between vocalization and respiration in mammals. Head Neck. 2011;33(Suppl 1):S21–5.
Morice AH, Millqvist E, Belvisi MG, Bieksiene K, Birring SS, Chung KF, Dal Negro RW, Dicpinigaitis P, Kantar A, McGarvey LP, Pacheco A, Sakalauskas R, Smith JA. Expert opinion on the cough hypersensitivity syndrome in respiratory medicine. Eur Respir J. 2014;44(5):1132–48.
Bucca CB, Bugiani M, Culla B, Guida G, Heffler E, Mietta S, Moretto A, Rolla G, Brussino L. Chronic cough and irritable larynx. J Allergy Clin Immunol. 2011;127(2):412–9.
Qiu Z, Yu L, Xu S, Liu B, Zhao T, Lu H. Cough reflex sensitivity and airway inflammation in patients with chronic cough due to non-acid gastro-oesophageal reflux. Respirology. 2011;16(4):645–52.
Murry T, Branski RC, Yu K, Cukier-Blaj S, Duflo S, Aviv JE. Laryngeal sensory deficits in patients with chronic cough and paradoxical vocal fold movement disorder. Laryngoscope. 2010;120(8):1576–81.
Aviv JE, Martin JH, Kim T, Sacco RL, Thomson JE, Diamond B, Close LG. Laryngopharyngeal sensory discrimination testing and the laryngeal adductor reflex. Ann Otol Rhinol Laryngol. 1999;108(8):725–30.
Cunningham JJ, Halum SL, Butler SG, Postma GN. Intraobserver and interobserver reliability in laryngopharyngeal sensory discrimination thresholds: a pilot study. Ann Otol Rhinol Laryngol. 2007;116(8):582–8.
Hammer MJ. Design of a new somatosensory stimulus delivery device for measuring laryngeal mechanosensory detection thresholds in humans. IEEE Trans Biomed Eng. 2009;56(4):1154–9.
Haynes RB, You JJ. The architecture of diagnostic research. In: Knottnerus JA, Buntinx F, editors. The evidence base of clinical diagnosis: theory and methods of diagnostic research. 2nd ed. Oxford: Wiley-Blackwell-BMJ Books; 2009. p. 20–41.
Giraldo-Cadavid LF, Agudelo-Otalora LM, Burguete J, Arbulu M, Moscoso WD, Martínez F, Ortiz AF, Diaz J, Pantoja JA, Rueda-Arango AF, Fernández S. Design, development and validation of a new laryngo-pharyngeal endoscopic esthesiometer and range-finder based on the assessment of air-pulse variability determinants. Biomed Eng Online. 2016;15(1):1–23.
Giraldo-Cadavid LF, Burguete J, Rueda F, Galvis AM, Castaneda N, Agudelo-Otalora LM, Moscoso WD, Paez N, Fernandez S. Reliability of a laryngo-pharyngeal esthesiometer and a method for measuring laryngo-pharyngeal mechano-sensitivity in a prospectively recruited cohort of patients. Eur Arch Otorhinolaryngol. 2017;274(7):2861–70.
Aviv JE, Sacco RL, Thomson J, Tandon R, Diamond B, Martin JH, Close LG. Silent laryngopharyngeal sensory deficits after stroke. Ann Otol Rhinol Laryngol. 1997;106(2):87–93.
World Health Organization. Global Health Observatory Data Repository. 2012 Mortality and global health estimates. WHO; 2012. http://apps.who.int/gho/data/node.resources. Accessed 11 July 2015.
Nguyen AT, Jobin V, Payne R, Beauregard J, Naor N, Kimoff RJ. Laryngeal and velopharyngeal sensory impairment in obstructive sleep apnea. Sleep. 2005;28(5):585–93.
Wang X, Ouyang Y, Wang Z, Zhao G, Liu L, Bi Y. Obstructive sleep apnea and risk of cardiovascular disease and all-cause mortality: a meta-analysis of prospective cohort studies. Int J Cardiol. 2013;169(3):207–14.
Morice AH. The cough hypersensitivity syndrome: a novel paradigm for understanding cough. Lung. 2010;188(Suppl 1):S87–90.
Johansson A, Millqvist E, Nordin S, Bende M. Relationship between self-reported odor intolerance and sensitivity to inhaled capsaicin: proposed definition of airway sensory hyperreactivity and estimation of its prevalence. Chest. 2006;129(6):1623–8.
Vertigan AE, Bone SL, Gibson PG. Development and validation of the Newcastle laryngeal hypersensitivity questionnaire. Cough. 2014;10(1):1.
Rofes L, Arreola V, Lopez I, Martin A, Sebastian M, Ciurana A, Clave P. Effect of surface sensory and motor electrical stimulation on chronic poststroke oropharyngeal dysfunction. Neurogastroenterol Motil. 2013;25(11):888-e701.
Pauloski BR, Logemann JA, Rademaker AW, Lundy D, Sullivan PA, Newman LA, Lazarus C, Bacon M. Effects of enhanced bolus flavors on oropharyngeal swallow in patients treated for head and neck cancer. Head Neck. 2013;35(8):1124–31.
Sackett DL, Haynes RB. The architecture of diagnostic research. BMJ. 2002;324(7336):539–41.
Nierenberg AA, Feinstein AR. How to evaluate a diagnostic marker test. Lessons from the rise and fall of dexamethasone suppression test. JAMA. 1988;259(11):1699–702.
Knottnerus JA, van Weel C, Muris JW. Evaluation of diagnostic procedures. BMJ. 2002;324(7335):477–80.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36.
Bossuyt P, Davenport C, Deeks J, Hyde C, Leeflang M, Scholten R. Chapter 11: interpreting results and drawing conclusions. In: Deeks J, Bossuyt P, Gatsonis C, editors. Cochrane handbook for systematic reviews of diagnostic test accuracy version 0.9. London: The Cochrane Collaboration; 2013.
Aviv JE. Prospective, randomized outcome study of endoscopy versus modified barium swallow in patients with dysphagia. Laryngoscope. 2000;110(4):563–74.
Aviv JE, Martin JH, Keen MS, Debell M, Blitzer A. Air pulse quantification of supraglottic and pharyngeal sensation: a new technique. Ann Otol Rhinol Laryngol. 1993;102(10):777–80.
Doggett DL, Turkelson CM, Coates V. Recent developments in diagnosis and intervention for aspiration and dysphagia in stroke and other neuromuscular disorders. Curr Atheroscler Rep. 2002;4(4):311–8.
Giraldo-Cadavid LF, Leal-Leaño LR, Leon-Basantes GA, Bastidas AR, Garcia R, Ovalle S, Abondano-Garavito JE. Accuracy of endoscopic and videofluoroscopic evaluations of swallowing for oropharyngeal dysphagia. Laryngoscope. 2016;. doi:10.1002/lary.26419.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11(2):93–8.
Gates J, Hartnell GG, Gramigna GD. Videofluoroscopy and swallowing studies for neurologic disease: a primer. Radiographics. 2006;26(1):e22.
Machin D, Campbell MJ, Tan SB, Tan SH. Reference intervals and receiver operating curves. In: Machin D, Campbell MJ, Tan SB, Tan SH, editors. Sample size tables for clinical studies. 3rd ed. West Sussex: Wiley-Blackwell; 2009. p. 158–78.
Hosmer DW, Lemeshow S. Applied logistic regression. 2nd ed. New York: Wiley; 2000.
Bours GJ, Speyer R, Lemmens J, Limburg M, de Wit R. Bedside screening tests vs. videofluoroscopy or fibreoptic endoscopic evaluation of swallowing to detect dysphagia in patients with neurological disorders: systematic review. J Adv Nurs. 2009;65(3):477–93.
Kiernan MC, Vucic S, Cheah BC, Turner MR, Eisen A, Hardiman O, Burrell JR, Zoing MC. Amyotrophic lateral sclerosis. Lancet. 2011;377(9769):942–55.
Lee SP, Lee KN, Lee OY, Lee HL, Jun DW, Yoon BC, Choi HS, Kim SH. Risk factors for complications of percutaneous endoscopic gastrostomy. Dig Dis Sci. 2014;59(1):117–25.
Oujamaa L, Relave I, Froger J, Mottet D, Pelissier JY. Rehabilitation of arm function after stroke. Literature review. Ann Phys Rehabil Med. 2009;52(3):269–93.
Eccles R, Lee PCL. Cough induced by airway vibration as a model of airway hyperreactivity in patients with acute upper respiratory tract infection. Pulm Pharmacol Ther. 2004;17(6):337–42.
Vertigan AE, Bone SL, Gibson PG. Laryngeal sensory dysfunction in laryngeal hypersensitivity syndrome. Respirology. 2013;18(6):948–56.
Morrison M, Rammage L. The irritable larynx syndrome as a central sensitivity syndrome [Le syndrome du larynx irritable: un syndrome de sensibilité centrale]. Can J Speech Lang Pathol Audiol. 2010;34(4):282–9.
Grushka M, Sessle BJ, Howley TP. Psychophysical assessment of tactile, pain and thermal sensory functions in burning mouth syndrome. Pain. 1987;28(2):169–84.
Funding
This study was funded by Colciencias, Colombia (Grant 768-2013) and by the University of La Sabana Chia, Colombia (Grant MED-164-2013). It also received support from the University of Navarra, Pamplona, Spain.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Luis F. Giraldo-Cadavid, Javier Burguete, Mario Arbulu, and Secundino Fernandez have a Patent granted by the Colombian’s Superintendencia de Industria y Comercio to the Laryngo-pharyngeal Endoscopic Esthesiometer and Range Finder (LPEER) (No. 13-121843-00003-0000), a PCT (International Application No. PCT/IB2014/061063) and a US Patent in process. University of La Sabana (Colombia) is the owner of the financial rights for this patent and the authors own the intellectual property over this patent.
Additional information
Institutions where the work was performed: Pulmonary Medicine Service and the Rehabilitation Department of the Clinica University of La Sabana, Chia, Cundinamarca, Colombia. Interventional Pulmonology Division, Fundacion Neumologica Colombiana, Bogota, DC, Colombia.
Rights and permissions
About this article
Cite this article
Giraldo-Cadavid, L.F., Burguete, J., Rueda, F. et al. Accuracy of a Laryngopharyngeal Endoscopic Esthesiometer (LPEER) for Evaluating Laryngopharyngeal Mechanosensitivity: A Validation Study in a Prospectively Recruited Cohort of Patients. Dysphagia 33, 15–25 (2018). https://doi.org/10.1007/s00455-017-9826-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-017-9826-y