Abstract
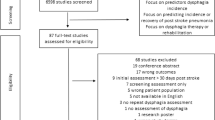
Oropharyngeal dysphagia is a common condition after stroke, Parkinson’s disease (PD), and Alzheimer’s disease (AD), and can cause serious complications including malnutrition, aspiration pneumonia, and premature mortality. Despite its high prevalence among the elderly and associated serious complications, dysphagia is often overlooked and under-diagnosed in vulnerable patient populations. This systematic review aimed to improve understanding and awareness of the prevalence of dysphagia in susceptible patient populations. MEDLINE, EMBASE, the Cochrane library, PROSPERO, and disease-specific websites were systematically searched for studies reporting oropharyngeal dysphagia prevalence or incidence in people with stroke, PD, AD, traumatic brain injury, and community-acquired pneumonia, from the USA, Canada, France, Germany, Italy, Spain, UK, Japan, China, and regional studies. The quality of study descriptions were assessed based on STROBE guidelines. A total of 1207 publications were identified and 33 met inclusion criteria: 24 in stroke, six in PD, two in traumatic brain injury, and one in patients with traumatic brain injury. Dysphagia was reported in 8.1–80 % of stroke patients, 11–81 % of PD, 27–30 % of traumatic brain injury patients, and 91.7 % of patients with community-acquired pneumonia. No relevant studies of dysphagia in AD were identified. This review demonstrates that dysphagia is highly prevalent in these populations, and highlights discrepancies between studies, gaps in dysphagia research, and the need for better dysphagia management starting with a reliable, standardized, and validated method for oropharyngeal dysphagia identification.

Similar content being viewed by others
References
Rofes L, Arreola V, Almirall J, Cabré M, Campins L, García-Peris P, et al. Diagnosis and management of oropharyngeal dysphagia and its nutritional and respiratory complications in the elderly. Gastroenterol Res Pract. 2011. doi:10.1155/2011/818979.
Stechmiller JK. Early nutritional screening of older adults: review of nutritional support. J Infus Nurs. 2003;26:170–7.
Marik PE, American College of Chest Physicians. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003;124:328–36.
Johnston BT, Li Q, Castell JA, Castell DO. Swallowing and esophageal function in Parkinson’s disease. Am J Gastroenterol. 1995;90:1741–6.
Kalia M. Dysphagia and aspiration pneumonia in patients with Alzheimer’s disease. Metabolism. 2003;52:36–8.
Singh S, Hamdy S. Dysphagia in stroke patients. Postgrad Med J. 2006;82:383–91.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–8.
Crary MA, Carnaby GD, Sia I, Khanna A, Waters MF. Spontaneous swallowing frequency has potential to identify dysphagia in acute stroke. Stroke. 2013;44:3452–7.
Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, et al. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009;18:329–35.
Gonzalez-Fernandez M, Kuhlemeier KV, Palmer JB. Racial disparities in the development of dysphagia after stroke: analysis of the California (MIRCal) and New York (SPARCS) inpatient databases. Arch Phys Med Rehabil. 2008;89:1358–65.
Kopey SA, Chae J, Vargo MM. Does a 3-sip test detect dysphagia in acute stroke rehabilitation patients? PM R. 2010;2:822–8.
Martino R, Silver F, Teasell R, Bayley M, Nicholson G, Streiner DL, et al. The Toronto Bedside Swallowing Screening Test (TOR-BSST): development and validation of a dysphagia screening tool for patients with stroke. Stroke. 2009;40:555–61.
Auyeung M, Tsoi TH, Mok V, Cheung CM, Lee CN, Li R, et al. Ten year survival and outcomes in a prospective cohort of new onset Chinese Parkinson’s disease patients. J Neurol Neurosurg Psychiatry. 2012;83:607–11.
Barichella M, Cereda E, Madio C, Iorio L, Pusani C, Cancello R, et al. Nutritional risk and gastrointestinal dysautonomia symptoms in Parkinson’s disease outpatients hospitalised on a scheduled basis. Br J Nutr. 2013;110:347–53.
Almirall J, Rofes L, Serra-Prat M, Icart R, Palomera E, Arreola V, et al. Oropharyngeal dysphagia is a risk factor for community-acquired pneumonia in the elderly. Eur Respir J. 2013;41:923–8.
Barer DH. The natural history and functional consequences of dysphagia after hemispheric stroke. J Neurol Neurosurg Psychiatry. 1989;52:236–41.
Bravata DM, Daggett VS, Woodward-Hagg H, Damush T, Plue L, Russell S, et al. Comparison of two approaches to screen for dysphagia among acute ischemic stroke patients: nursing admission screening tool versus National Institutes of Health stroke scale. J Rehabil Res Dev. 2009;46:1127–34.
Brody RA, Touger-Decker R, VonHagen S, Maillet JO. Role of registered dietitians in dysphagia screening. J Am Diet Assoc. 2000;100:1029–37.
Cecconi E, Palumbo M, Suardelli M, Di Clemente L, Toscano M, Bertora P, et al. Post-stroke dysphagia: clinical, cognitive and neuroanatomical correlates. Cerebrovasc Dis. 2010;29:294.
Cecconi E, Campiglio L, Toscano M, Petolicchio B, Capiluppi E, Bertora PL, et al. Leukoaraiosis and stroke severity as independent predictors of post-stroke dysphagia. Eur J Neurol. 2011;18:38.
Chumbler N. Demographic and clinical risk factors for dysphagia in acute stroke patients. Stroke. 2009;40:e276.
Cola MG, Daniels SK, Corey DM, Lemen LC, Romero M, Foundas AL. Relevance of subcortical stroke in dysphagia. Stroke. 2010;41:482–6.
Crary MA, Humphrey JL, Carnaby-Mann G, Sambandam R, Miller L, Silliman S. Dysphagia, nutrition, and hydration in ischemic stroke patients at admission and discharge from acute care. Dysphagia. 2012;28:69–76.
Daniels SK, Brailey K, Priestly DH, Herrington LR, Weisberg LA, Foundas AL. Aspiration in patients with acute stroke. Arch Phys Med Rehabil. 1998;79:14–9.
Daniels SK, Schroeder MF, McClain M, Corey DM, Rosenbek JC, Foundas AL. Dysphagia in stroke: development of a standard method to examine swallowing recovery. J Rehabil Res Dev. 2006;43:347–56.
Daniels SK, Schroeder MF, DeGeorge PC, Corey DM, Foundas AL, Rosenbek JC. Defining and measuring dysphagia following stroke. Am J Speech Lang Pathol. 2009;18:74–81.
Finestone HM, Greene-Finestone LS, Wilson ES, Teasell RW. Malnutrition in stroke patients on the rehabilitation service and at follow-up: prevalence and predictors. Arch Phys Med Rehabil. 1995;76:310–6.
Gordon C, Hewer RL, Wade DT. Dysphagia in acute stroke. BMJ. 1987;295:411–4.
Guyomard V, Fulcher RA, Redmayne O, Metcalf AK, Potter JF, Myint PK. Effect of dysphasia and dysphagia on inpatient mortality and hospital length of stay: a database study. J Am Geriatr Soc. 2009;57:2101–6.
Heckert KD, Komaroff E, Adler U, Barrett AM. Postacute reevaluation may prevent dysphagia-associated morbidity. Stroke. 2009;40:1381–5.
Stolzenburg J, Herrmann O, Hacke W, Gaugel D, Ringleb PA. Prevalence and outcome of dysphagia in patients with Wallenberg’s syndrome. Stroke. 2009;40:e105–276.
Teasell R, Foley N, Fisher J, Finestone H. The incidence, management, and complications of dysphagia in patients with medullary strokes admitted to a rehabilitation unit. Dysphagia. 2002;17:115–20.
Turner-Lawrence DE, Peebles M, Price MF, Singh SJ, Asimos AW. A feasibility study of the sensitivity of emergency physician dysphagia screening in acute stroke patients. Ann Emerg Med. 2009;54:344–8.
Young EC, Durant-Jones L. Developing a dysphagia program in an acute care hospital: a needs assessment. Dysphagia. 1990;5:159–65.
Bine JE, Frank EM, McDade HL. Dysphagia and dementia in subjects with Parkinson’s disease. Dysphagia. 1995;10:160–4.
Clarke CE, Gullaksen E, Macdonald S, Lowe F. Referral criteria for speech and language therapy assessment of dysphagia caused by idiopathic Parkinson’s disease. Acta Neurol Scand. 1998;97:27–35.
Coates C, Bakheit AM. Dysphagia in Parkinson’s disease. Eur Neurol. 1997;38:49–52.
Lam K, Lam FKY, Lau KK, Chan YK, Kan EYL, Woo J, et al. Simple clinical tests may predict severe oropharyngeal dysphagia in Parkinson’s disease. Mov Disord. 2007;22:640–4.
Field LH, Weiss CJ. Dysphagia with head injury. Brain Inj. 1989;3:19–26.
Winstein CJ. Neurogenic dysphagia. Frequency, progression, and outcome in adults following head injury. Phys Ther. 1983;63:1992–7.
Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJPM. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24(Suppl 1):57–65.
Clavé P, Arreola V, Romea M, Medina L, Palomera E, Serra-Prat M. Accuracy of the volume-viscosity swallow test for clinical screening of oropharyngeal dysphagia and aspiration. Clin Nutr. 2008;27:806–15.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63.
Kennedy G, Pring T, Fawcus R. No place for motor speech acts in the assessment of dysphagia Intelligibility and swallowing difficulties in stroke and Parkinson’s disease patients. Eur J Disord Commun. 1993;28:213–26.
Acknowledgments
CT determined the study concept and design. JK contributed to the searches, selected the references, and carried out the data extraction and quality assessment. JK and EG carried out the analysis and interpretation of the data, with input from CT and RS. EG drafted the manuscript with critical revision for important intellectual content from CT and RS. We would also like to acknowledge Sheila Ubamadu who carried out the systematic searches.
Funding
This work was funded by Nestlé Health Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Claire Takizawa is an employee of Nestlé Health Science. Elizabeth Gemmell and at the time of submission James Kenworthy, are employed by PHMR Ltd. and Nestle Health Science funded the research that is reported in this paper. Renée Speyer has received funding from industry Nestlé Health Science, Fresenius-Kabi, Nutricia, Speech Pathology Australia, the European Society for Swallowing Disorders, and the Korean Dysphagia Society.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Takizawa, C., Gemmell, E., Kenworthy, J. et al. A Systematic Review of the Prevalence of Oropharyngeal Dysphagia in Stroke, Parkinson’s Disease, Alzheimer’s Disease, Head Injury, and Pneumonia. Dysphagia 31, 434–441 (2016). https://doi.org/10.1007/s00455-016-9695-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-016-9695-9