Abstract
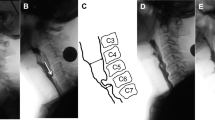
Dysphagia has previously been reported in the inflammatory myopathies (IMs): inclusion body myositis (IBM), dermatomyositis (DM), and polymyositis (PM). Patients report coughing, choking, and bolus sticking in the pharynx. Myotomy has been the treatment of choice, with variable success reported. We sought to determine underlying causes of dysphagia in IM patients using instrumental evaluation. Eighteen subjects participated in the study: four with DM, six with PM, and eight with IBM. They underwent simultaneous videofluoroscopy and manometry, yielding 214 swallows for analysis regarding function of the upper esophageal sphincter (UES), swallow initiation, hyolaryngeal excursion, and pharyngeal residue. Penetration and aspiration were also recorded. UES failed to relax in two participants. High incidence of pharyngeal dysphagia was noted; 72% of participants demonstrated abnormalities, including delayed swallow initiation (24%), decreased hyolaryngeal excursion (22%), pyriform residue (17%), and penetration (22%). Dysphagia in IM patients appears to be more due to impaired muscle contraction and reduced hyolaryngeal excursion than the often held belief of failed UES relaxation. The distinction between mechanisms causing patients’ dysphagia should be examined, particularly if CP myotomy is being considered as it may be contraindicated for patients with normal UES relaxation. More studies investigating IM patients pre- and post-myotomy are needed.






Similar content being viewed by others
References
Dalakas MC. Sporadic inclusion body myositis: diagnosis pathogenesis and therapeutic strategies. Nat Clin Pract Neurol. 2005;2:437–47.
Oh TH, Brumfield KA, Hoskin TL, Stolp KA, Murray JA, Basford JR. Dysphagia in inflammatory myopathy: clinical characteristics, treatment strategies, and outcome in 62 patients. Mayo Clin Proc. 2007;82:4.
Mastaglia FL. Inflammatory muscle diseases. Neurol India. 2008;56:263–70.
Mastaglia FL, Phillips BA. Idiopathic inflammatory myopathies: epidemiology, classification and diagnostic criteria. Rheum Dis Clin N Am. 2002;28:723–41.
Flachenecker P. Epidemiology of neuroimmunological diseases. J Neurol. 2006;253:2–8.
Houser SM, Calabrease LH, Strome M. Dysphagia in patients with inclusion body myositis. Laryngoscope. 1998;108:1001–5.
Liu LWC, Tarnopolsky M, Armstrong D. Injection of botulinum toxin A to the upper esophageal sphincter for oropharyngeal dysphagia in two patients with inclusion body myositis. Can J Gastroenterol. 2004;18:397–9.
Needham M, Mastaglia FL. Inclusion body myositis: current pathogenetic concepts and diagnostic and therapeutic approaches. Lancet Neurol. 2007;6:620–31.
Needham M, James I, Corbett A, Day T, Christiansen F, Phillips B, Mastaglia FL. Sporadic inclusion body myositis: phenotypic variability and influence of HLA-DR3 in a cohort of 57 Australian cases. J Neurol Neurosurg Psychiatry. 2008;79:1056–60.
Cox FM, Verschuuren JJ, Verbist BM, Niks EH, Wintzen AR, Badrising UA. Detecting dysphagia in inclusion body myositis. J Neurol. 2009;256:2009–13.
Nagano H, Yoshifuku K, Kurono Y. Polymyositis with dysphagia treated with endoscopic balloon dilatation. Auris Nasas Larynx. 2009;36:705–8.
Parodi A, Caproni M, Marzano AV, De Simone C, La Placa M, Quaglini P, Veller Formasa C, Zane C, Vaccaro M, Papini M, Fabbri P, Rebora A. Dermatomyositis in 132 patients with different clinical subtypes: cutaneous signs, constitutional symptoms and circulating antibodies. Acta Derm Venereol. 2002;82:48–51.
Na SJ, Kim SM, Sunwoo IN, Choi YC. Clinical characteristics and outcomes of juvenile and adult dermatomyositis. J Korean Med Sci. 2009;24:715–21.
Sivarao DV, Goyal RK. Functional anatomy and physiology of the upper esophageal sphincter. Am J Med. 2000;108:27S–37S.
Ertekin C, Secil Y, Yuceyar N, Aydogdu I. Oropharyngeal dysphagia in polymyositis/dermatomyositis. Clin Neurol Neurosurg. 2004;107:32–7.
Oddis CV. Idiopathic inflammatory myopathy: management and prognosis. Rheum Dis Clin North Am. 2002;28:979–1001.
Postma GN, Butler SG, Belafsky PC, Halum SL. Normal pharyngeal and upper esophageal sphincter manometry. Ear Nose Throat J. 2004;83(12):809.
Atherton M, Bellis-Smith N, Cichero JAY, Suter M, Dietitians Association of Australia and Speech Pathology Australia. The Australian standardized terminology and definitions for texture modified foods and fluids [editorial]. Nutr Diet. 2007;64:S53–76.
Nicosia MA, Robbins J. The usefulness of the line spread test as a measure of liquid consistency. Dysphagia. 2007;22:306–11.
Williams RB, Wallace KL, Ali GN, Cook IJ. Biomechanics of failed deglutitive upper esophageal sphincter relaxation in neurogenic dysphagia. Am J Physiol Gastrointest Liver Physiol. 2002;283:G16–26.
Castell DO, Diederich LL, Castell JA. Esophageal motility and pH testing. Highlands Ranch: Sandhill Scientific; 2000.
Williams RB, Grehan MJ, Hersch M, Andre J, Cook IJ. Biomechanics, diagnosis and treatment outcome in inflammatory myopathy presenting as oropharyngeal dysphagia. Gut. 2003;42:471–8.
Belafsky PC. The pharyngoesophageal segment (PES). 2006. Available at www.vitalstim.com/health_professionals/certified_provider_resources/index.aspx?fid=358. Accessed 9 June 2010
Butler SG, Stuart A, Castell D, Russell GB, Koch K, Kemp S. Effects of age, gender, bolus condition, viscosity, and volume of pharyngeal and upper esophageal sphincter pressure and temporal measurements during swallowing. J Speech Lang Hear Res. 2009;52:240–53.
Langmore SE. Endoscopic evaluation and treatment of swallowing disorders. New York: Thieme; 2001.
Butler SG, Stuart A, Kemp S. Flexible endoscopic evaluation of swallowing in healthy young and older adults. Ann Otol Rhinol Laryngol. 2009;118:99–106.
Butler SG, Stuart A, Markley L, Rees C. Penetration and aspiration in healthy older adults as assessed during endoscopic evaluation of swallowing. Ann Otol Rhinol Laryngol. 2009;118:190–8.
Allen JE, White CJ, Leonard RJ, Belafsky PC. Prevalence of penetration and aspiration on videofluoroscopy in normal individuals without dysphagia. Otolaryngol Head Neck Surg. 2010;142:208–13.
Daggett A, Logemann J, Rademaker A, Pauloski B. Laryngeal penetration during deglutition in normal subjects of various ages. Dysphagia. 2006;21:270–4.
Kelly AM, Drinnan MJ, Leslie P. Assessing penetration and aspiration: how do videofluoroscopy and fiberoptic endoscopic evaluation of swallowing compare? Laryngoscope. 2007;117:1723–7.
Paik NJ, Kim SJ, Lee HJ, Jeon JY, Lim JY, Han TR. Movement of the hyoid bone and the epiglottis during swallowing in patients with dysphagia from different etiologies. J Electromyogr Kinesiol. 2008;18:329–35.
Kelly JH. Management of upper esophageal sphincter disorders: indications and complications of myotomy. Am J Med. 2000;108:43S–7S.
Singh S, Hamdy S. The upper esophageal sphincter. Neurogastroenterol Motil. 2005;17:3–12.
Dua K, Surapaneni SN, Kuribayashi S, Hafeezullah M, Shaker R. Protective role of aerodigestive reflexes against aspiration: study on subjects with impaired and preserved reflexes. Gastroenterology. 2011;140:1927–33.
Shaker R, Ren J, Bardan E, Easterling C, Dua K, Xie P, Kern M. Pharyngoglottal closure reflex: characterization in healthy young, elderly and dysphagic patients with predeglutitive aspiration. Gerontology. 2003;49:12–20.
Dua K, Surapaneni SN, Kuribayashi S, Hafeezullah M, Shaker R. Pharyngeal airway protective reflexes are triggered before the maximum volume of fluid that the hypopharynx can safely hold is exceeded. Am J Physiol Gastrointest Liver Physiol. 2011;301(2):G197–202.
Acknowledgment
This work was supported by a grant from the Sir Charles Gairdner Hospital Research Fund.
Conflict of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Claire Langdon, P., Mulcahy, K., Shepherd, K.L. et al. Pharyngeal Dysphagia in Inflammatory Muscle Diseases Resulting from Impaired Suprahyoid Musculature. Dysphagia 27, 408–417 (2012). https://doi.org/10.1007/s00455-011-9384-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-011-9384-7