Abstract
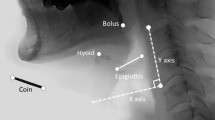
As a bolus enters the pharynx during the swallow, the airway is protected by laryngeal closure, a process characterized by approximation of the vocal folds plus approximation of the arytenoid cartilages to the base of the epiglottis. The purpose of this study was to measure initiation of laryngeal closure (ILC) and laryngeal closure duration (LCD) in three groups of subjects: (1) ten stroke patients who aspirated before and during the swallow (aspirators), (2) ten stroke patients who did not aspirate (nonaspirators), and (3) ten normal control subjects. Means and standard deviations of ILC and LCD were analyzed for both 5-ml and 10-ml thin-liquid boluses using a 100-ms timer during subsequent analysis of videofluoroscopic swallowing examinations. There were significant differences between aspirators and control subjects for both ILC and LCD, and significant differences between aspirators and nonaspirators for ILC. There were no significant differences between aspirators and nonaspirators for LCD. Both delayed ILC and reduced LCD were associated with post-stroke aspiration. Delayed ILC is a significant indicator of overall risk of aspiration. Clinical implications for these findings are discussed.


Similar content being viewed by others
References
Logemann JA, Kahrilas PJ, Cheng J, Pauloski BR, Gibbons PJ, Rademaker AW, et al. Closure mechanisms of laryngeal vestibule during swallowing. Am J Physiol Gastrointest Liver Physiol. 1992;262(2 Pt 1):G338–44.
Gordon C, Hewer RL, Wade DT. Dysphagia in acute stroke. Br Med J (Clin Res Ed). 1987;295(6595):411–4.
Tracy JF, Logemann JA, Kahrilas PJ, Jacob P, Kobara M, Krugler C. Preliminary observations on the effects of age on oropharyngeal deglutition. Dysphagia. 1969;4:90–4. doi:10.1007/BF02407151.
Robbins JA, Hamilton JW, Lof GL, Kempster GB. Oropharyngeal swallowing in normal adults of different ages. Gastroenterology. 1992;103:823–9.
Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA, Kahrilas PJ, Smith CH. Temporal and biomechanical characteristics of oropharyngeal swallow in younger and older men. J Speech Lang Hear Res. 2000;43(5):1264–74.
Logemann JA, Pauloski BR, Rademaker AW, Kahrilas PJ. Oropharyngeal swallow in younger and older women: videofluoroscopic analysis. J Speech Lang Hear Res. 2002;45(3):434–45. doi:10.1044/1092-4388(2002/034).
Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999;10:744–8.
Robbins J, Levine RL. Swallowing after unilateral stroke of the cerebral cortex: preliminary experience. Dysphagia. 1988;3:11–7. doi:10.1007/BF02406275.
Robbins J, Levine RL, Maser A, Rosenbek JC, Kempster GB. Swallowing after unilateral stroke of the cerebral cortex. Arch Phys Med Rehabil. 1993;74:1295–300. doi:10.1016/0003-9993(93)90082-L.
Kendall KA, Leonard RJ. Bolus transit and airway protection coordination in older dysphagic patients. Laryngoscope. 2001;111:2017–21. doi:10.1097/00005537-200111000-00028.
Kahrilas PJ, Lin S, Rademaker AW, Logemann JA. Impaired deglutitive airway protection: a videofluoroscopic analysis of severity and mechanism. Gastroenterology. 1997;113(5):1457–64. doi:10.1053/gast.1997.v113.pm9352847.
Kim Y, McCullough GH, Asp CW. Stage transition duration in patients post-stroke. Dysphagia. 2007;22(4):299–305. doi:10.1007/s00455-007-9085-4.
Rademaker AW, Pauloski BR, Logemann JA, Shanahan TK. Oropharyngeal swallow efficiency as a representative measure of swallowing function. J Speech Hear Res. 1994;37:314–25.
Perlman AL, Booth BM, Grayhack JP. Videofluoroscopic predictors of aspiration in patients with oropharyngeal dysphagia. Dysphagia. 1994;9:90–5. doi:10.1007/BF00714593.
Kendall KA, Leonard RJ, McKenzie S. Airway protection: evaluation with videofluoroscopy. Dysphagia. 2004;19:65–70.
Power ML, Hamdy S, Singh S, Tyrrell PJ, Turnbull I, Thompson DG. Deglutitive laryngeal closure in stroke patients. J Neurosurg Psychiatry. 2007;78:141–6. doi:10.1136/jnnp.2006.101857.
Bisch EM, Logemann JA, Rademaker AW, Kahrilas PJ, Lazarus CL. Pharyngeal effects of bolus volume, viscosity, and temperature in patients with dysphagia resulting from neurologic impairment and in normal subjects. J Hear Speech Lang Sci. 1994;37(5):1041–59.
McCullough GH, Wertz RT, Rosenbek JC. Sensitivity and specificity of clinical/bedside examination signs for detecting aspiration in adults subsequent to stroke. J Commun Disord. 2001;34:55–72. doi:10.1016/S0021-9924(00)00041-1.
McCullough GH, Wertz RT, Rosenbek JC. Age, gender, size, consistency effects on swallowing function in adults between 21 and 99 years of age. Albuquerque, NM: the 10th Annual Dysphagia Research Society; 2001.
Sellars C, Campbell AM, Stott DJ, Stewart M, Wilson JA. Swallowing abnormalities after acute stroke: a case control study. Dysphagia. 1999;14(4):212–8. doi:10.1007/PL00009608.
Curtis DJ, Sepulveda GU. Epiglottic motion: video recording of muscular dysfunction. Radiology. 1983;148:473–7.
Daniels SK, Schroeder MF, McClain M, Corey DM, Rosenbek JC, Foundas AL. Dysphagia in stroke: development of a standard method to examine swallowing recovery. J Rehabil Res Dev. 2006;43(3):347–56. doi:10.1682/JRRD.2005.01.0024.
Robbins J, Kays SA, Gangnon RE, Hind JA, Hewitt AL, Gentry LR, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007;88(2):150–8. doi:10.1016/j.apmr.2006.11.002.
Logemann JA, Pauloski BR, Rademaker AW, Colangelo L. Super-supraglottic swallow in irradiated head and neck cancer patients. Head Neck. 1997;19(6):535–40. doi:10.1002/(SICI)1097-0347(199709)19:6<535::AID-HED11>3.0.CO;2-4.
Acknowledgment
This work was performed at the School of Hearing, Speech and Language Sciences, Ohio University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, T., Kim, Y., Ko, DH. et al. Initiation and Duration of Laryngeal Closure During the Pharyngeal Swallow in Post-Stroke Patients. Dysphagia 25, 177–182 (2010). https://doi.org/10.1007/s00455-009-9237-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-009-9237-9