Abstract
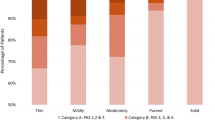
A high incidence of oropharyngeal dysphagia (OD) in acute-care settings has been reported; however, no data on its management are found in the literature. Here we report the experience with rehabilitative management of OD in a large Italian hospital. The characteristics of inpatients with OD during 2004 have been studied prospectively. For each patient, demographic data, the department referring the patient, the disease causing OD, and the presence of a communication disorder were registered. The swallowing level at the beginning and at the end of rehabilitation were recorded. Of the 35,590 inpatients admitted to San Giovanni Battista Hospital of Turin during 2004, 222 of them were referred for the assessment and rehabilitation of OD. The inpatients with OD came from different departments and mainly had a neurologic disease. In 110 patients a communication disorder was present. The swallowing impairment was moderate to severe at the moment of referral, while on average patients were able to eat by mouth after swallowing therapy. Dysphagia rehabilitation in an acute care setting is requested from different departments because of its prevalence and severity; skilled specialists are needed for early assessment and the best management.


Similar content being viewed by others
References
Cook IJ. AGA technical review on management of oropharyngeal dysphagia. Gastroenterology 1999;116:455–478.
Logemann JA. Therapy for oropharyngeal swallowing disorders. In: Perlman AL, Schulze-Delrieu K, Editors. Deglutition and its disorders. San Diego, CA: Singular, 1997, pp. 449–461.
Schindler A, Grosso E, Tiddia C, Cavalot AL, Ricca G, Ottaviani F, Schindler O. Swallowing disorders: management data. Acta Otorhinolaryngol Ital 2003;23:180–184.
Reilly S. The evidence base for the management of dysphagia. In: Reilly S, Douglas J, Oates J, Editors. Evidence based practice in speech pathology. London: Whurr, 2004.
Logemann JA. Dysphagia: evaluation and treatment. Folia Phoniatr Logop 1995;47:140–164.
Odderson IR, Keaton JC, McKenna BS. Swallow management in patients on an acute stroke pathway: quality is cost effective. Arch Phys Med Rehabil 1995;76:1130–1133.
Logemann JA. Evaluation and treatment of swallowing disorders, 2nd ed. Austin, TX: Pro-Ed, 1998.
Schindler A, Spadola Bisetti M, Favero E, Musto R, Ottaviani F, Schindler O. Role of videoendoscopy in phoniatrics: data from three years of daily practice. Acta Otorhinolaryngol Ital 2005;25:43–49.
Rubin JS, Wendler J, Woisard V, Dejonckere PH, Wellens W, Kotby N. Phoniatric provision and training: current European perspectives. J Laryngol Otol 2007;121:427–430.
ASHA (American Speech-Language-Hearing Association), Skills needed by speech-language pathologists providing services to dysphagic patients/clients. Am Speech Lang Hear Assoc 1990;32(Suppl 2):7–12.
ASHA (American Speech-Language-Hearing Association), Omnibus survey results: 1995 edition. Rockville, MD: ASHA, 1995.
Groher ME, Bukatman R. The prevalence of swallowing disorders in two teaching hospitals. Dysphagia 1986;1:3–6.
ASHA (American Speech-Language-Hearing Association), Omnibus survey results: 2001 edition. Rockville, MD: ASHA, 2001.
Smithard DG, O’Neill PA, Park C, Morris J, Wyatt R, England R, Martin DF. Complications and outcome after acute stroke. Does dysphagia matter? Stroke 1996;27:1200–1204.
Bath PM, Bath FJ, Smithard DG. Interventions for dysphagia in acute stroke. Cochrane Dabase Syst Rev 2000;2:CD000323.
Perry L, Love CP. Screening for dysphagia and aspiration in acute stroke: a systematic review. Dysphagia 2001;16:7–18.
Ramsey DJC, Smithard DG, Kalra L. Early assessment of dysphagia and aspiration risk in acute stroke patients. Stroke 2003;34:1252–1257.
Bastian RW. Videoendoscopic evaluation of patients with dysphagia: an adjunct to the modified barium swallow. Otolaryngol Head Neck Surg 1991;104:339–350.
Logemann JA. Manual for the videofluorographic study of swallowing. London: Taylor & Francis, 1986.
American Speech-Language-Hearing Association National Outcome Measurement System (NOMS), Adult Speech-Language Pathology training manual. Rockville, MD: ASHA, 1998.
Cope N, Hall K. Head injury rehabilitation: benefit of early intervention. Arch Phys Med Rehabil 1982;63:433–437.
Logemann JA. Evaluation and treatment of swallowing problems after TBI. In: Zasler ND, Katz DI, Zafonte RD, Editors. Brain injury medicine. New York: Demos, 2007, pp. 887–894.
Mackay LE, Morgan AS, Bernstein BA. Swallowing disorders in severe brain injury: risk factors affecting return to oral intake. Arch Phys Med Rehabil 1999;80:365–371.
Wesling M, Brady S, Jensen M, Nickell M, Statkus D, Escobar N. Dysphagia outcomes in patients with brain tumors undergoing inpatient rehabilitation. Dysphagia 2003;18:203–210.
Schindler JS, Kelly JH. Swallowing disorders in the elderly. Laryngoscope 2002;112:589–602.
Leslie P, Drinnan MJ, Ford GA, Wilson JA. Swallow respiratory patterns and aging: presbyphagia or dysphagia? J Gerontol A Biol Sci Med Sci 2005;60:391–395.
Tracy JF, Logemann JA, Kahrilas PJ, Jacob P, Kobara M, Krugler C. Preliminary observations on the effects of age on oropharyngeal deglutition. Dysphagia 1989;4:90–94.
Gleeson DCL. Oropharyngeal swallowing and aging: a review. J Commun Disord 1999;32:373–396.
Agency for Health Care Policy and Research (AHCPR), Diagnosis and treatment of swallowing disorders (dysphagia) in acute care stroke patients. Evidence Report Technology Assessment 8, 1999.
Scottish Intercollegiate Guidelines Network (SIGN), Management of patients with stroke: Identification and management of dysphagia, 2004.
Stroke Prevention and Educational Awareness Diffusion (SPREAD), Ictus Cerebrale: linee guida italiane di prevenzione e trattamento, 2003.
Doggett DL, Tappe KA, Mitchell MD, Chapell R, Coates V, Turkelson CM. Prevention of pneumonia in elderly stroke patients by systematic diagnosis and treatment of dysphagia: an evidence-based comprehensive analysis of the literature. Dysphagia 2001;16:279–295.
Langmore SE. Dysphagia in neurologic patients in the intensive care unit. Sem Neurol 1996;16:329–340.
Mackay LE, Chapman PE, Morgan AS. The contribution of speech/language pathology in critical care. In: Mackay LE, Chapman PE, Morgan AS, Editors. Maximizing brain injury recovery: integrating critical care and early rehabilitation. Gaithersburg, MD: Aspen Publishers, 1997, pp. 444–482.
Acknowledgments
The authors thank Prof. O. Ekberg and Dr. V. Woisard for careful reading and reviewing of earlier drafts of the manuscript. The contribution of an anonymous reviewer that significantly improved the article is also acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schindler, A., Vincon, E., Grosso, E. et al. Rehabilitative Management of Oropharyngeal Dysphagia in Acute Care Settings: Data from a Large Italian Teaching Hospital. Dysphagia 23, 230–236 (2008). https://doi.org/10.1007/s00455-007-9121-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-007-9121-4