Abstract
Minimally invasive (MI) esophageal resection (ER) has the theoretical advantage of reduced postoperative complications compared with standard ER. However, the impact of MIER on rates and severity of pulmonary complications is unclear. Four patients underwent laparoscopic gastroesophageal mobilization and resection followed by gastric pull-up and cervical esophageal anastomosis (MIER). Videofluoroscopic swallowing studies (VFSS) assessed pharyngolaryngeal function postoperatively. All postoperative complications were documented. Each MIER was completed successfully without intraoperative complications. Mean operative time was 4.3 ± 2 h. Postoperatively, VFSS detected laryngeal penetration, vocal cord paralysis, and/or aspiration in three patients, two of whom experienced severe respiratory complications. MIER patients are susceptible to aspiration, likely due to transient denervation of the pharynx and laryngeal structures. Following MIER, aggressive pulmonary toilet and aspiration precautions are emphasized to reduce pulmonary complications. Furthermore, serial evaluation of deglutition is encouraged to guide the safe and appropriate resumption of oral feeding.
Similar content being viewed by others
Esophageal resection (ER) remains the treatment standard for resectable esophageal cancer and for some benign esophageal conditions [1]. Despite surgical and anesthetic advances, morbidity and mortality rates of ER are consistently higher than those associated with other commonly performed general and thoracic surgical procedures [2]. Importantly, pulmonary complications occur in as many as 25% of patients after ER, and aspiration pneumonia represents the major cause of early death in ER patients [3–5]. In fact, it has been estimated that approximately two-thirds of deaths after ER are associated with respiratory complications [3].
Various minimally invasive (MI) approaches to ER have been introduced with the goals of decreased surgical morbidity and faster postoperative recovery [1,6–12]. Select centers have shown reduced intensive care unit and hospital stays and decreased blood loss following MIER compared with standard ER [1,6,8,10], but conclusive evidence for decreased postoperative complications after MIER is lacking, particularly since most reports on MIER suffer from patient selection biases and none involve head-to-head comparison with open resection techniques [1,7,8]. Furthermore, few studies have specifically addressed the effect of MIER on pulmonary complications. Osugi et al. [7] recently compared open ER with thoracoscopic ER and stated that thoracoscopic ER preserves pulmonary function. However, MIER did not differ from open ER in rates of pneumonia (20%) and recurrent laryngeal nerve injury (18%). Similar observations have been noted elsewhere [6,10].
The purpose of this study was to review our recent experience with laparoscopic transhiatal ER to determine the degree to which these patients remain at risk for respiratory complications. We found that although this particular procedure can be performed safely, patients remained at extremely high risk for pulmonary morbidity, which is likely due to transient denervation of pharyngeal or laryngeal structures. These findings reiterate the need for careful evaluation of swallowing abnormalities by videofluoroscopic or fiberoptic techniques after ER in order to reduce the rates and consequences of aspiration and respiratory complications.
Methods
Four patients presented for treatment of various esophageal disorders over a one-year period (September 2002 to August 2003) to a single tertiary care center for gastroesophageal disorders. Indications for surgery are listed in Table 1. Laparoscopic transhiatal esophageal resection (MIER) was performed in each patient. The perioperative course of each patient was retrospectively reviewed. Particular attention was given to intraoperative details, postoperative course, and the results of swallow function testing.
Surgical Technique
The arrangement for MIER is shown in Figure 1. Details of the procedure have been previously described [9,10]. Briefly, three 11-mm laparoscopic trocars were inserted in the upper abdomen, with one trocar positioned to the left of midline in a supraumbilical location and the other two in the bilateral midclavicular lines subcostally. Bilateral 5-mm laparoscopic trocars were also placed in the anterior axillary lines (Fig. 1). Gastric mobilization and esophageal dissection well into the posterior mediastinum were performed using a flexible laparoscope (Olympus LTF-V3, Olympus America Inc., Melville, NY) and ultrasonic shears (Ethicon Endo-Surgery Inc., Cincinnati, OH) for tissue division. The vagus nerves were transected at the level of the gastroesophageal junction early in the dissection to minimize inferiorly oriented traction upon the left vagus nerve and the left recurrent laryngeal nerve (RLN). Heinecke-Mikulicz pyloroplasty was performed in each patient. After mobilizing the stomach and thoracic esophagus, the cervical esophagus was encircled through an incision paralleling the medial border of the left sternocleidomastoid muscle. Anastomosis of the stomach to the cervical esophagus was performed using a modified Collard technique [13]. All patients were initially admitted to the surgical intensive care unit, and postoperative management was guided by a care pathway.
The arrangement for laparoscopic transhiatal esophagectomy is demonstrated. Three 10-mm and two 5-mm ports are placed as shown in the abdomen. All gastroesophageal mobilization is completed transabdominally and into the posterior mediastinum. The cervical esophagus is approached through a standard left neck incision.
Results
All MIER procedures were completed successfully without conversion to an open procedure. The average length of operation was 4.3 ± 2 h. The mean estimated blood loss was 160 ± 70 ml. The right pleural cavity was entered in two patients, both of whom required postoperative pleural cavity drainage. No other intraoperative complications were noted. Specifically, the left RLN was considered to be intact and undisturbed in each case.
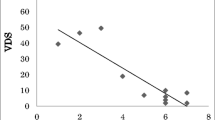
Postoperatively, swallowing function was prospectively assessed in each patient. Individual results after MIER are shown in Table 1. Patient No. 1 was reintubated shortly after surgery for progressive hypoxemia. Because of a prolonged hospital course, videofluoroscopic swallowing study (VFSS) was delayed until one month after ER. This study revealed severe deficits of the oral preparatory phase, reduced laryngeal elevation, and laryngeal penetration and aspiration (Fig. 2A). Subsequently, fiberoptic examination demonstrated left vocal cord paralysis, decreased supraglottic sensation, and aspiration suggesting a combined injury of the left RLN and the superior laryngeal nerve (Fig. 2B). The patient ultimately expired due to the severity of illness. Patient No. 2 required reintubation on postoperative day 2 for respiratory distress and ultimately developed pneumonia. VFSS revealed penetration/aspiration in the context of severe pharyngeal-phase dysphagia, characterized by incomplete laryngeal elevation and pharyngeal residue. These findings prohibited oral nutrition even when the patient was discharged on postoperative day 16. Enteral feeding was maintained through a feeding catheter jejunostomy until the patient eventually demonstrated resolution of swallowing dysfunction upon reexamination approximately one month after surgery. Patient No. 3 reported subjective hoarseness on postoperative day 1 and was found to have left vocal cord immobility by indirect laryngoscopy. However, VFSS performed on postoperative day 4 failed to demonstrate any swallowing abnormalities, and the patient was discharged to home on postoperative day 5 tolerating a regular diet. Patient No. 4 resumed oral intake after VFSS on post operative day 5 and did not demonstrate any swallowing abnormalities. The patient was discharged to home on postoperative day 8.
Other complications of MIER were infrequently encountered and are listed in Table 1. Patient No. 3 developed a chylothorax which resolved with conservative measures and did not require thoracic exploration. Patient No. 4 developed postoperative atrial fibrillation, which resolved spontaneously and was not hemodynamically significant.
Discussion
Respiratory insufficiency is widely recognized as a dominant feature affecting the postoperative course of patients undergoing ER. In fact, aspiration pneumonia is the most common and most lethal complication of ER [3–5]. Because it is often presumed that the origin for most ER-associated pulmonary morbidity is related to standard chest or abdominal incisions with secondary inspiratory splinting [6,11], minimally invasive (MI) ER has been promoted as a means to decrease the morbidity of ER. However, according to Law and Wong [6,14], most iterations of MIER have failed to demonstrate conclusively that complications of ER are lessened by minimized incisions. Therefore, the advantages of MIER compared with those of open ER are still debated. Certainly, excellent results have been reported in select centers using minimally invasive resection techniques. For instance, Luketich et al. [1] have demonstrated an incredibly low operative mortality rate of 1.4% for over 200 patients treated with MIER, which is strikingly low compared with other reports of open resection [4,5]. In addition, they also report surprisingly few cases of pneumonia (7.6%) and respiratory distress syndrome (5%). Finally, their data analysis suggests that MIER may be associated with improved quality of life among those patients surviving beyond two years after surgery when compared with historical controls of open ER. While these data are impressive, they have been criticized on the basis of patient selection bias, and data were not compared with a concurrent set of patients undergoing open esophagectomy [1].
In this study, we evaluated patients after MIER to ascertain whether residual risk for aspiration and respiratory complications is present after such procedures. In this admittedly small series of patients, two of four patients had documented aspiration or laryngeal penetration on videofluoroscopic swallowing evaluation postoperatively, both of whom developed severe respiratory complications. Furthermore, these two patients and a third additional patient had vocal cord paralysis (VCP). Therefore, in the present study, both patients who had abnormal swallowing studies also had pulmonary complications after MIER. These findings as well as support from existing literature argue against a predominant mechanism whereby incisional pain leads to inadequate pulmonary toilet and atelectasis followed by respiratory insufficiency. Rather, it appears that postesophagectomy pulmonary complications are often related to reduced airway protection and aspiration as a result of transient denervation of the vocal cords or the motor or sensory function of the pharyngeal region [4,5,15,16]. Importantly, it is emphasized that such deficits are typically transient, as was seen in two of the three patients in the present study and has been noted previously [15,16].
To reiterate, the present study suggests that the risk for aspiration after esophagectomy is not decreased by the minimally invasive approach used in the present series. This is most likely related to the actual process of mobilizing the cervical or thoracic esophagus regardless of the incision through which access to the esophagus is gained. During ER, manipulation of the esophagus renders the recurrent laryngeal nerve (RLN) susceptible to traction or stretch injury at the level of the aortic arch or in the cervical region [16]. As a result, new swallowing abnormalities have been noted in 67% of patients following open transhiatal ER, and laryngeal penetration with tracheal aspiration occurred in almost half of those with newly discovered swallowing disorders [15]. Recently, Tangoku [12] showed a 36% rate of VCP after MIER.
To reduce pulmonary complications following ER, several suggestions for preventing RLN injury have been proposed. These include early division of the vagus nerves to avoid inferiorly oriented RLN traction, clean and careful cervical esophageal dissection, and avoiding placement of retractors in the tracheoesophageal groove during the cervical phase of ER [1,17]. Furthermore, novel approaches to esophageal mobilization have been introduced that may reduce the likelihood for RLN-related complications [9,12,18], although this remains speculative. Upon identification of postesophagectomy swallowing abnormalities, various rehabilitation techniques may also be instituted to help prevent aspiration and subsequent respiratory complications, including the chin tuck maneuver and swallowing exercises [19,20]. However, none of the patients comprising the present study required these therapies.
Multiple physiologic defects have been associated with RLN injury, including vocal fold motion abnormalities, pharyngeal dysfunction, and cricopharyngeal denervation, all predisposing to aspiration of pharyngeal contents and/or diminished airway protection. Sensory deficits generally compound the effects of motor deficits associated with RLN injury. Indeed, the most severe forms of swallowing impairment are classically associated with combined injuries to both the RLN and the superior laryngeal nerve (SLN), because of additional loss of laryngeal sensory input with SLN damage [17,21,22]. This appears to have been the case with Patient No. 2 in our study. To further illustrate the prevalence of postesophagectomy swallowing disorders, one study found that over 70% of patients had reduced or absent laryngeal sensation, which was directly associated with silent aspiration [21].
Following ER, early videofluoroscopic or fiberoptic swallowing evaluation is promoted to define the individual’s risk for aspiration and to assist in recommendations for the safe resumption of oral intake. Both videofluoroscopy swallow study (VFSS) and fiberoptic endoscopic evaluation of swallowing (FEES) provide better assessment of swallowing abnormalities than bedside clinical evaluation and they allow more informed clinical decision-making with regard to appropriate dietary recommendations [17,23]. Leder [24] has reported that serial FEES exams allow safe and early resumption of an oral diet at the appropriate consistency. When FEES results guided postoperative management, complications of aspiration were completely prevented.
Certainly, other factors may contribute to the development of pulmonary complications after ER. For instance, Law et al. [25] recently reported that advanced patient age, proximal tumor location, and prolonged operating times were each independently associated with pulmonary complications following esophagectomy. In the present series, however, the patients were at the younger end of the age spectrum and operative times were relatively low. However, a relatively proximal tumor location may have been an issue in Patient No. 2. It is felt that proximal tumor location most likely places the RLN at higher risk relative to pathology located near the gastroesophageal junction [25]. Finally, Makay et al. [26] postulated that certain issues related to anesthetic management during esophagectomy, particularly MIER, may contribute to pulmonary complications postoperatively. For example, in their study comparing MIER with open ER, they found a higher rate of pleural entry and intraoperative pneumothoraces in the MIER group. This led to increased end-tidal carbon dioxide and significantly increased airway pressures in the MIER group compared with the open ER group. However, Makay et al. found no difference in postoperative pulmonary complications between the two groups. In the present series, two patients required closed thoracic drainage of pneumothoraces incurred at surgery. However, based on the Makay study, it is unlikely this led to the observed pulmonary complications, particularly in light of the observed abnormal swallowing studies.
Conclusions
The present study is unique in that it documents swallowing abnormalities and aspiration risk after MIER. Because pulmonary complications are the most common source of morbidity and mortality after ER, a protocol instituting proactive identification of swallowing dysfunction by videofluoroscopic or fiberoptic techniques should be considered.
References
Luketich JD, Alvelo-Rivera M, Buenaventura PO, Christie NA, McCaughan JS, Litle VR, Schauer PR, Close JM, Fernando HC: Minimally invasive esophagectomy: outcomes in 222 patients. Ann Surg 238:486–495, 2003
Birkmeyer JD, Siewers AE, Finlayson EVA, Stukel TA, Lucas FL, Batista I, Welch G, Wennberg DE: Hospital volume and surgical mortality in the United States. N Eng J Med 346:1128–1137, 2002
Dumont P, Wihlm JM, Hentz JG, Roeslin N, Lion R, Morand G: Respiratory complications after surgical treatment of esophageal cancer: a study of 309 patients according to the type of resection. Eur J Cardiothorac Surg 9:539–543, 1995
Bailey SH, Bull DA, Harpole DH, Rentz JJ, Neumayer LA, Pappas TN, Daley J, Henderson WG, Krasnicka B, Khuri SF: Outcomes after esophagectomy: a ten-year prospective cohort. Ann Thorac Surg 75:217–222, 2003
Atkins BZ, Shah AS, Hutcheson KA, Mangum JH, Pappas TN, Harpole DH Jr, D’Amico TA: Reducing hospital morbidity and mortality following esophagectomy. Ann Thorac Surg 78:1170–1176, 2004
Law S, Fok M, Chu KM, Wong J: Thoracoscopic esophagectomy for esophageal cancer. Surgery 122:8–14, 1997
Osugi H, Takemura M, Higashino M, Takada N, Lee S, Kinoshita H: A comparison of video-assisted thoracoscopic oesophagectomy and radical lymph node dissection for squamous cell cancer of the oesophagus with open operation. Br J Surg 90:108–113, 2003
Nguyen NT, Follette DM, Wolfe BM, Schneider PD, Roberts P, Goodnight JE Jr: Comparison of minimally invasive esophagectomy with transthoracic and transhiatal esophagectomy. Arch Surg 135:920–925, 2000
Bonavina L, Bona D, Binyom PR, Peracchia A: A laparoscopy-assisted surgical approach to esophageal carcinoma: J Surg Res 117:52–57, 2004
van den Broek WT, Makay O, Berends FJ, Yuan JZ, Houdijk APJ, Meijer S, Cuesta MA: Laparoscopically assisted transhiatal resection for malignancies of the distal esophagus. Surg Endosc 18:812–817, 2004
Cuesta MA, van den Broek WT, van der Peet DL, Meijer S: Minimally invasive esophageal resection. Surg Endosc 18:629–632, 2004
Tangoku A, Yoshino S, Abe T, Hayashi H, Satou T, Ueno T, Oka M: Mediastinoscope-assisted transhiatal esophagectomy for esophageal cancer. Surg Endosc 18:338–389, 2004
Ercan S, Rice TW, Murthy SC, Rybicki LA, Blackstone EH: Does esophagogastric anastomotic technique influence the outcome of patients with esophageal cancer? J Thorac Cardiovasc Surg 129:623–631, 2005
Law S, Wong J: Use of minimally invasive oesophagectomy for cancer of the oesophagus. Lancet Oncol 3:215–222, 2002
Heitmiller RF, Jones B: Transient diminished airway protection after transhiatal esophagectomy. Am J Surg 162:442–446, 1991
Johnson PR, Kanegoanker GS, Bates T: Indirect laryngoscopic evaluation of vocal cord function in patients undergoing transhiatal esophagectomy. J Am Coll Surg 178:605–608, 1994
Périé S, Laccourreye O, Bou-Malhab F, Brasnu D: Aspiration in unilateral recurrent laryngeal nerve paralysis after surgery. Am J Otolaryngol 19:18–23, 1998
Costi R, Himpens J, Bruyns J, Cadiere GB: Totally laparoscopic transhiatal esophago-gastrectomy without thoracic or cervical access. Surg Endosc 18:629–632, 2004
Lewin JS, Hebert TM, Putnam JB Jr, DuBrow RA: Experience with the chin tuck maneuver in postesophagectomy aspirators. Dysphagia 16:216–219, 2001
Shaker R, Easterling C, Kern M, Nitschke T, Massey B, Daniels S, Grande B, Kazandjian M, Dikeman K: Rehabilitation of swallowing by exercise in tube-fed patients with pharyngeal dysphagia secondary to abnormal UES opening. Gastroenterology 122:1314–1321, 2002
Heitmiller RF, Tseng E, Jones B: Prevalence of aspiration and laryngeal penetration in patients with unilateral vocal fold motion impairment. Dysphagia 15:184–187, 2000
Setzen M, Cohen MA, Perlman PW, Belafsky PC, Guss J, Mattucci KF, Ditkoff M: The association between laryngopharyngeal sensory deficits, pharyngeal motor function, and the prevalence of aspiration with thin liquids. Otolaryngol Head Neck Surg 128:99–102, 2003
Aviv JE, Kim T, Sacco RL, Kaplan S, Goodhart K, Diamond B, Close LG: FEESST: a new bedside endoscopic test of the motor and sensory components of swallowing. Ann Otol Rhinol Laryngol 107:378–387, 1998
Leder SB: Serial fiberoptic endoscopic swallowing evaluations in the management of patients with dysphagia. Arch Phys Med Rehabil 79:1264–1269, 1998
Law S, Wong K-H, Kwok K-F, Chu K-M, Wong J: Predictive factors for postoperative pulmonary complications and mortality after esophagectomy for cancer. Ann Surg 240:791–800, 2004
Makay O, van den Broek WT, Yuan JZ, Veerman DP, Helfferich DWH, Cuesta MA: Anesthesiological hazards during laparoscopic transhiatal esophageal resection: a case control study of the laparoscopic-assisted vs. the conventional approach. Surg Endosc 18:1263–1267, 2004
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Atkins, B.Z., Fortes, D.L. & Watkins, K.T. Analysis of Respiratory Complications After Minimally Invasive Esophagectomy: Preliminary Observation of Persistent Aspiration Risk. Dysphagia 22, 49–54 (2007). https://doi.org/10.1007/s00455-006-9042-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-006-9042-7