Abstract
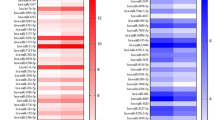
The peri-tooth root alveolar loss often does not have sufficient space for repair material transplantation and plasticity. Mesenchymal stem cell (MSC) sheets have an advantage in providing more extracellular matrix (ECM) and may prove to be a new therapeutic consideration for this bone defect repair. The identification of key regulators that stimulate MSCs’ osteogenic potential and sheet-derived ECM deposition is the key to promoting its application. In this study, we found that inhibition or overexpression of miR-196a-5p led to a decline or enhancement, respectively, in the alkaline phosphatase (ALP) activity, mineralization, and the levels of osteogenic markers, Osteocalcin (OCN), Dentin Matrix Protein 1 (DMP1), Bone Sialoprotein (BSP), and Dentin Sialophosphoprotein (DSPP) of Wharton’s jelly of umbilical cord stem cells (WJCMSCs) in vitro. Moreover, the 5,6-Carboxyfluorescein Diacetate Succinimidyl Ester (CFSE) analysis revealed inhibition of the WJCMSCs’ proliferative ability upon miR-196a-5p overexpression. Characterization of the sheet formation by picrosirius red and Masson staining indicated that miR-196a-5p overexpression significantly promoted the collagen content in whole WJCMSC sheet–derived ECM. Furthermore, micro-CT and histopathology results indicated that the miR-196a-5p-overexpressed WJCMSC sheets significantly promoted new bone regeneration and rat calvarial bone defect closure 12 weeks following transplantation. The mRNA microarray analysis of miR-196a-5p-overexpressed WJCMSCs revealed 959 differentially expressed genes (DEGs) (34 upregulated and 925 downregulated). Moreover, 241 genes targeted by miR-196a-5p were predicted by using miRNA function websites of which only 19 predicted genes were consistent with the microarray revealed DEGs. Hence, one unrevealed downregulated DEG Serpin Family B Member 2 (SERPINB2) was investigated. And the deletion of SERPINB2 enhanced the ALP activity and mineralization of WJCMSCs in vitro. In conclusion, our study found that miR-196a-5p, as a key regulator, could repress the proliferation tendency, while stimulating osteogenic ability and WJCMSC sheet–derived ECM deposition, thus promoting new bone formation and rat calvarial bone defect closure. Furthermore, SERPINB2 is a key downstream gene involved in the miR-196a-5p-promoted WJCMSC osteogenesis.







Similar content being viewed by others
Abbreviations
- ADSCs:
-
Adipose-derived stem cells
- ALP:
-
Alkaline phosphatase
- BMSCs:
-
Bone marrow mesenchymal stem cells
- BSP:
-
Bone Sialoprotein
- CFSE:
-
5,6-Carboxyfluorescein Diacetate Succinimidyl Ester
- CLDN11:
-
Claudin
- DAPI:
-
4′,6‐Diamidino‐2‐phenylindole dihydrochloride
- DEGs:
-
Differentially expressed genes
- DPSCs:
-
Dental pulp stem cells
- DSPP:
-
Dentin Sialophosphoprotein
- DMP1:
-
Dentin Matrix Protein 1
- ECM:
-
Extracellular matrix
- ENPP1:
-
Ectonucleotide pyrophosphatase phosphodiesterase 1
- EVs:
-
Extracellular vesicles
- GNAS:
-
GNAS Complex Locus
- H&E:
-
Hematoxylin-eosin
- HOXC8 :
-
homeobox C8
- IL6 :
-
interleukin 6
- micro-CT:
-
micro-computed tomography
- MiRNA:
-
microRNA
- miR‐196a-5p:
-
microRNA-196a-5p
- MSCs:
-
mesenchymal stem cells
- OCN:
-
Osteocalcin
- RT-PCR:
-
Reverse transcriptase polymerase chain reaction
- SD:
-
Sprague Dawley
- SERPINB2 :
-
Serpin Family B Member 2
- VCAM1 :
-
Vascular cell adhesion molecule 1
- WJCMSCs:
-
Wharton’s jelly of umbilical cord stem cells
References
Aghebati-Maleki L, Dolati S, Zandi R et al (2019) Prospect of mesenchymal stem cells in therapy of osteoporosis: a review. J Cell Physiol 234(6):8570–8578
Andrés-Sastre E, Nossin Y, Jansen I et al (2021) A new semi-orthotopic bone defect model for cell and biomaterial testing in regenerative medicine. Biomaterials 279:121187
Bakhshandeh B, Zarrintaj P, Oftadeh MO et al (2017) Tissue engineering; strategies, tissues, and biomaterials. Biotechnol Genet Eng Rev 33(2):144–172
Cabrera-Pérez R, Monguió-Tortajada M, Gámez-Valero A et al (2019) Osteogenic commitment of Wharton’s jelly mesenchymal stromal cells: mechanisms and implications for bioprocess development and clinical application. Stem Cell Res Ther 10(1):356
Cao Y, Shi R, Yang H et al (2020) Epiregulin promotes osteogenic differentiation and inhibits neurogenic trans-differentiation of adipose-derived mesenchymal stem cells via MAPKs pathway. Cell Biol Int 44(4):1046–1058
Chen M, Xu Y, Zhang T et al (2019) Mesenchymal stem cell sheets: a new cell-based strategy for bone repair and regeneration. Biotechnol Lett 41(3):305–318
Daley GQ, Scadden DT (2008) Prospects for stem cell-based therapy. Cell 132(4):544–548
Davies JE, Walker JT, Keating A (2017) Concise review: Wharton’s jelly: the rich, but enigmatic, source of mesenchymal stromal cells. Stem Cells Transl Med 6(7):1620–1630
Ding DC, Chang YH, Shyu WC et al (2015) Human umbilical cord mesenchymal stem cells: a new era for stem cell therapy. Cell Transplant 24(3):339–347
El-Badawy A, El-Badri N (2016) Clinical efficacy of stem cell therapy for diabetes mellitus: a meta-analysis. PLoS ONE 11(4):e0151938
Elsafadi M, Manikandan M, Atteya M et al (2017) SERPINB2 is a novel TGFβ-responsive lineage fate determinant of human bone marrow stromal cells. Sci Rep 7(1):10797
Fan Z, Yamaza T, Lee J et al (2009) BCOR regulates mesenchymal stem cell function by epigenetic mechanisms. Nat Cell Biol 11(8):1002–1009
Fujii Y, Kawase-Koga Y, Hojo H et al (2018) Bone regeneration by human dental pulp stem cells using a helioxanthin derivative and cell-sheets technology. Stem Cell Res Ther 9(1):24
Gaihre B, Uswatta S, Jayasuriya AC (2017) Reconstruction of craniomaxillofacial bone defects using tissue-engineering strategies with injectable and non-injectable scaffolds. J Funct Biomater 8(4):49
Han X, Yang H, Liu H et al (2021) miR-196b-5p inhibits proliferation of Wharton’s jelly umbilical cord stem cells. FEBS Open Bio 11(1):278–288
Harris NLE, Vennin C, Conway JRW et al (2017) SerpinB2 regulates stromal remodelling and local invasion in pancreatic cancer. Oncogene 36(30):4288–4298
Hu L, Zhao B, Gao Z et al (2020) Regeneration characteristics of different dental derived stem cell sheets. J Oral Rehabil 47(1):66–72
Jamalpoor Z, Soleimani M, Taromi N et al (2019) Comparative evaluation of morphology and osteogenic behavior of human Wharton’s jelly mesenchymal stem cells on 2D culture plate and 3D biomimetic scaffold. J Cell Physiol 234(12):23123–23134
Kim YJ, Bae SW, Yu SS et al (2009) miR-196a regulates proliferation and osteogenic differentiation in mesenchymal stem cells derived from human adipose tissue. J Bone Miner Res 24(5):816–825
La Rocca G, Lo Iacono M, Corsello T et al (2013) Human Wharton’s jelly mesenchymal stem cells maintain the expression of key immunomodulatory molecules when subjected to osteogenic, adipogenic and chondrogenic differentiation in vitro: new perspectives for cellular therapy. Curr Stem Cell Res Ther 8:100–113
Lee JA, Yerbury JJ, Farrawell N et al (2015) SerpinB2 (PAI-2) modulates proteostasis via binding misfolded proteins and promotion of cytoprotective inclusion formation. PLoS ONE 10(6):e0130136
Lee YC, Chan YH, Hsieh SC et al (2019) Comparing the osteogenic potentials and bone regeneration capacities of bone marrow and dental pulp mesenchymal stem cells in a rabbit calvarial bone defect model. Int J Mol Sci 20(20):5015
Lin X, Patil S, Gao YG et al (2020) The bone extracellular matrix in bone formation and regeneration. Front Pharmacol 11:757
Liu H, Han X, Yang H et al (2020) GREM1 inhibits osteogenic differentiation, senescence and BMP transcription of adipose-derived stem cells. Connect Tissue Res 1–12
Liu Y, Fang J, Zhang Q et al (2020) Wnt10b-overexpressing umbilical cord mesenchymal stem cells promote critical size rat calvarial defect healing by enhanced osteogenesis and VEGF-mediated angiogenesis. J Orthop Translat 23:29–37
Monguió-Tortajada M, Roura S, Gálvez-Montón C et al (2017) Mesenchymal stem cells induce expression of CD73 in human monocytes in vitro and in a swine model of myocardial infarction in vivo. Front Immunol 8:1577
Nanci A, Bosshardt DD (2000) Structure of periodontal tissues in health and disease. Periodontol 2006(40):11–28
Nawa K, Ikeno H, Matsuhashi N et al (2013) Discovering small molecules that inhibit adipogenesis and promote osteoblastogenesis: unique screening and Oncostatin M-like activity. Differentiation 86(1–2):65–74
Rasmussen HH, van Damme J, Puype M et al (1992) Microsequences of 145 proteins recorded in the two-dimensional gel protein database of normal human epidermal keratinocytes. Electrophoresis 13(12):960–969
Schindeler A, Mills RJ, Bobyn JD et al (2018) Preclinical models for orthopedic research and bone tissue engineering. J Orthop Res 36(3):832–840
Smith BT, Shum J, Wong M et al (2015) Bone tissue engineering challenges in oral & maxillofacial surgery. Adv Exp Med Biol 881:57–78
Socorro M, Shinde A, Yamazaki H et al (2020) Trps1 transcription factor represses phosphate-induced expression of SerpinB2 in osteogenic cells. Bone 141:115673
Styrkarsdottir U, Stefansson OA, Gunnarsdottir K et al (2019) GWAS of bone size yields twelve loci that also affect height, BMD, osteoarthritis or fractures. Nat Commun 10(1):2054
Sybil D, Jain V, Mohanty S et al (2020) Oral stem cells in intraoral bone formation. J Oral Biosci 62(1):36–43
Takafuji Y, Tatsumi K, Kawao N et al (2021) MicroRNA-196a-5p in extracellular vesicles secreted from myoblasts suppresses osteoclast-like cell formation in mouse cells. Calcif Tissue Int 108(3):364–376
Ustriyana P, Schulte F, Gombedza F et al (2021) Spatial survey of non-collagenous proteins in mineralizing and non-mineralizing vertebrate tissues ex vivo. Bone Rep 14:100754
Walmsley GG, Ransom RC, Zielins ER et al (2016) Stem cells in bone regeneration. Stem Cell Rev Rep 12(5):524–529
Wang J, Liu S, Li J et al (2019a) Roles for miRNAs in osteogenic differentiation of bone marrow mesenchymal stem cells. Stem Cell Res Ther 10(1):197
Wang L, Xu W, Chen Y et al (2019b) Alveolar bone repair of rhesus monkeys by using BMP-2 gene and mesenchymal stem cells loaded three-dimensional printed bioglass scaffold. Sci Rep 9(1):18175
Wang Y, Jia Z, Diao S et al (2016) IGFBP5 enhances osteogenic differentiation potential of periodontal ligament stem cells and Wharton’s jelly umbilical cord stem cells, via the JNK and MEK/Erk signalling pathways. Cell Prolif 49(5):618–627
Wang Z, Han L, Sun T et al (2021) Osteogenic and angiogenic lineage differentiated adipose-derived stem cells for bone regeneration of calvarial defects in rabbits. J Biomed Mater Res A 109(4):538–550
Wei F, Qu C, Song T et al (2012) Vitamin C treatment promotes mesenchymal stem cell sheets formation and tissue regeneration by elevating telomerase activity. J Cell Physiol 227(9):3216–3224
Wei F, Song T, Ding G et al (2013) Functional tooth restoration by allogeneic mesenchymal stem cell-based bio-root regeneration in swine. Stem Cells Dev 22(12):1752–1762
Zajdel A, Kałucka M, Kokoszka-Mikołaj E et al (2017) Osteogenic differentiation of human mesenchymal stem cells from adipose tissue and Wharton’s jelly of the umbilical cord. Acta Biochim Pol 64(2):365–369
Zhang J, Lv S, Liu X et al (2018) Umbilical cord mesenchymal stem cell treatment for Crohn’s disease: a randomized controlled clinical trial. Gut Liver 12(1):73–78
Zhang L, Xie H, Li S (2020) LncRNA LOXL1-AS1 controls osteogenic and adipocytic differentiation of bone marrow mesenchymal stem cells in postmenopausal osteoporosis through regulating the miR-196a-5p/Hmga2 axis. J Bone Miner Metab 38(6):794–805
Zhong LN, Zhang YZ, Li H et al (2019) Overexpressed miR-196a accelerates osteogenic differentiation in osteoporotic mice via GNAS-dependent Hedgehog signaling pathway. J Cell Biochem 120(12):19422–19431
Funding
This work was supported by grants from the General Program (Key Program, Major Research Plan) of the National Natural Science Foundation of China (81670948 to Y. C.).
Author information
Authors and Affiliations
Contributions
WY and ZS performed the experiments. WY analyzed the data. YH, YD, and ZY were responsible for collection of data and technical expertise. CY supplied experimental materials and resources. YH, CYY, and CY conceived the study. WY and CYY drafted the manuscript. CYY reviewed this work. All the authors approved the final manuscript. WY and ZS are senior authors, contributed equally, and are co-correspondents of CY to this work.
Corresponding author
Ethics declarations
Ethics approval
The animal study was approved by the animal care and use committee of Beijing Stomatological Hospital Animal laboratory (reference number: 81,670,948). The animal care and experimental procedure were performed following the guidelines of the Beijing Experimental Animal Management Ordinance. Human stem cell study complied with the ISSCR “guidelines for the Conduct of Human Embryonic Stem Cell Research.” Human WJCMSCs were obtained from ScienCell Research Laboratories (Carlsbad, CA, USA).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Y., Zhang, S., Yang, H. et al. MicroRNA-196a-5p overexpression in Wharton’s jelly umbilical cord stem cells promotes their osteogenic differentiation and new bone formation in bone defects in the rat calvarium. Cell Tissue Res 390, 245–260 (2022). https://doi.org/10.1007/s00441-022-03673-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-022-03673-2