Abstract
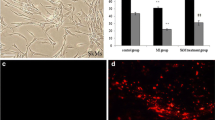
Interleukin (IL)-6 is a proinflammatory cytokine released in injured and contracting skeletal muscles. In this study, we examined cellular expression of proteins associated with cytoskeleton organization and cell migration, chosen on the basis of microRNA profiling, in rat primary skeletal muscle cells (RSkMC) treated with IL-6 (1 ng/ml) for 11 days. MiRNA microarray analysis and qRT-PCR revealed increased expression of miR-154-3p and miR-338-3p in muscle cells treated with IL-6. Pacsin3 was downregulated post-transcriptionally by IL-6, but not by IGF-I. Ephrin4A protein was increased both in IL-6- and IGF-I-treated myocytes. IL-6, but not IGF-I, stimulated migratory ability of RSkMC, examined in wound healing assay. Alpha-actinin protein was slightly augmented in RSKMC treated with IL-6, similarly to IGF-I. IL-6, but not IGF-I, upregulated desmin in differentiating RSkMC. IL-6 supplementation caused accumulation of alpha-actinin and desmin in near-nuclear area of muscle cells, which was manifested by increased ratio: mean near-nuclear fluorescence/mean peripheral cytoplasm fluorescence of these proteins. We concluded that IL-6, a known proinflammatory cytokine and a physical activity-associated myokine, acting during differentiation of primary skeletal muscle cells, alters expression of nonmuscle-specific miRNAs. This cytokine causes differential effects on pacsin-3 and ephrinA4, through post-transcriptional inhibition and stimulation, respectively. IL-6-exerted modifications of cytoskeletal proteins in muscle cells include both transcriptional (desmin and dynein heavy chain 5) and post-transcriptional activation (alpha-actinin). Moreover, IL-6 augments near-nuclear distribution of cytoskeletal proteins, alpha-actinin and desmin and promotes migration of myocytes. Such effects suggest that IL-6 plays a role during skeletal muscle regeneration, acting through mechanisms independent of regulation of myogenic program.









Similar content being viewed by others
References
Bartel D (2004) MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116:281–297
Benjamini Y, Hochberg Y, (1995) Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society: Series B (Methodological) 57 (1):289–300
Błaszczyk M, Gajewska M, Milewska M, Grzelkowska-Kowalczyk K (2017) Insulin-dependent cytoplasmic distribution of Rab4a in mouse adipocytes is inhibited by interleukin-6, -8, and -15. Cell Biol Int 41:457–463
Brosig M, Ferralli J, Gelman L, Chiquet M, Chiquet-Ehrismann R (2010) Interfering with the connection between the nucleus and the cytoskeleton affects nuclear rotation, mechanotransduction and myogenesis. Int J Biochem Cell Biol 42:1717–1728
Chapman MA, Zhang J, Banerjee I, Guo LT, Zhang Z, Shelton GD, Ouyang K, Lieber RL, Chen J (2014) Disruption of both nesprin 1 and desmin results in nuclear anchorage defects and fibrosis in skeletal muscle. Hum Mol Genet 23:5879–5892
Chen JF, Tao Y, Li J, Zhongliang D, Zhen Y, Xiao X, Da-Zhi W (2010) MicroRNA-1 and microRNA-206 regulate skeletal muscle satellite cell proliferation and differentiation by repressing Pax7. J Cell Biol 190:867–879
Coley WD, Bogdanik L, Vila MC, Yu Q, Van Der Meulen JH, Rayavarapu S, Novak JS, Nearing M, Quinn JL, Saunders A, Dolan C, Andrews W, Lammert C, Austin A, PartridgeTA CGA, Lutz C, Nagaraju K (2016) Effect of genetic background on the dystrophic phenotype in mdx mice. Hum Mol Genet 25:130–145
Dietze D, Ramrath S, Ritzeler O, Tennagels N, Hauner H, Eckel J (2004) Inhibitor 휅B kinase is involved in the paracrine crosstalk between human fat and muscle cells. Int J Obes 28:985–992
Eberhart J, Swartz ME, Koblar SA, Pasquale EB, Krull CE (2002) EphA4 constitutes a population-specific guidance cue for motor neurons. Dev Biol 247:89–101
Folker ES, Schulman VK, Baylies MK (2014) Translocating myonuclei have distinct leading and lagging edges that require kinesin and dynein. Development 141:355–366
Formigli L, Meacci E, Sassoli C, Squecco R, Nosi D, Chellini F, Naro F, Francini F, Zecchi-Orlandini S (2007) Cytoskeleton/stretch-activated ion channel interaction regulates myogenic differentiation of skeletal myoblasts. J Cell Physiol 211:296–306
Gallo G, Letourneau PC (2004) Regulation of growth cone actin filaments by guidance cues. J Neurobiol 58:92–102
Gautel M, Djinović-Carugo K (2016) The sarcomeric cytoskeleton: from molecules to motion. J Exp Biol 219:135–145
Grabiec K, Milewska M, Błaszczyk M, Gajewska M, Grzelkowska-Kowalczyk K (2015) Palmitate exerts opposite effects on proliferation and differentiation of skeletal myoblasts. Cell Biol Int 39:1044–1052
Gray SR, Kamolrat T (2011) The effect of exercise induced cytokines on insulin stimulated glucose transport in C2C12 cells. Cytokine 55:221–228
Grzelkowska-Kowalczyk K, Wieteska-Skrzeczyńska W (2010) Treatment with TNF-alpha and IFN-gamma alters the activation of Ser/Thr protein kinases and the metabolic response to IGF-I in mouse C2C12 myogenic cells. Cell Mol Biol Lett 15:13–31
Grzelkowska-Kowalczyk K, Grabiec K, Tokarska J, Gajewska M, Błaszczyk M, Milewska M (2015a) Insulin-like growth factor-i increases laminin, integrin subunits and metalloprotease ADAM12 in mouse myoblasts. Folia Biol (Krakow) 63:241–247
Grzelkowska-Kowalczyk K, Wicik Z, Majewska A, Tokarska J, Grabiec K, Kozłowski M, Milewska M, Błaszczyk M (2015b) Transcriptional regulation of important cellular processes in skeletal myogenesis through interferon-γ. J Interf Cytokine Res 35:89–99
Hansen CG, Nichols BJ (2010) Exploring the caves: cavins, caveolins and caveolae. Trends Cell Biol 20:177–186
Hawke TJ, Garry DJ (2001) Myogenic satellite cells: physiology to molecular biology. J Appl Physiol 91:534–551
Henderson CA, Gomez CG, Novak SM, Mi-Mi L, Gregorio CC (2018) Overview of the muscle cytoskeleton. Compr Physiol 7:891–944
Iresjö BM, Svensson J, Ohlsson C, Lundholm K (2013) Liver derived endocrine IGF-I is not sufficient for activation of skeletal muscle protein synthesis following oral feeding. BMC Physiol. https://doi.org/10.1186/1472-6793-13-7
Jacobson MD, Burne JF, Raff MC (1994) Programmed cell death and Bcl-2 protection in the absence of a nucleus. EMBO J 13:1899–1910
Joe AW, Yi L, Natarajan A, Le Grand F, So L, Wang J, Rudnicki MA, Rossi FM (2010) Muscle injury activates resident fibro/adipogenic progenitors that facilitate myogenesis. Nat Cell Biol 12:153–163
Kalantari R, Chiang C-M, Corey DR (2016) Regulation of mammalian transcription and splicing by nuclear RNAi. Nucleic Acids Res 44:524–537
Karalaki M, Fili S, Philippou A, Koutsilieris M (2009) Muscle regeneration: cellular and molecular events. In Vivo 23:779–796
Krauss RS (2010) Regulation of promyogenic signal transduction by cell-cell contact and adhesion. Exp Cell Res 316:3042–3049
Lee FX, Houweling PJ, North KN, Quinlan KG (2016) How does α-actinin-3 deficiency alter muscle function? Mechanistic insights into ACTN3, the 'gene for speed'. Biochim Biophys Acta 1863:686–693
Li J, Johnson SE (2013) Ephrin-A5 promotes bovine muscle progenitor cell migration before mitotic activation1. J Anim Sci 91:1086–1093
Li K, Pu C, Huang X, Liu J, Mao Y, Lu X (2014) Proteomic study of sporadic inclusion body myositis. Proteome Sci 12:45
Livak KJ, Schmittgen TD (2001) Analyzis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25:402–408
Majewska A, Domoradzki T, Grzelkowska-Kowalczyk K (2019) Transcriptomic profiling during myogenesis. In: Rønning SB (ed) Myogenesis. Methods and Protocols. Methods Mol Biol, 1889. Springer, New York, pp 127–168
McDaneld TG, Smith T, Doumit ME, Miles JR, Coutinho LL, Sonstegard TS, Matukumalli LK, Nonneman DJ, Wiedmann RT (2009) MicroRNA transcriptome profiles during swine skeletal muscle development. BMC Genomics. https://doi.org/10.1186/1471-2164-10-77
Milewska M, Domoradzki T, Majewska A, Błaszczyk M, Gajewska M, Hulanicka M, Grzelkowska-Kowalczyk K (2019a) Interleukin-6 modifies the expression profile of microRNA in rat primary skeletal muscle cells. Gene Expression Omnibus Data Repository //www.ncbi.nlm.nih.gov/geo/query/acc.cgi/, accession no: GSE126237
Milewska M, Domoradzki T, Majewska A, Błaszczyk M, Gajewska M, Hulanicka M, Ciecierska A, Grzelkowska-Kowalczyk K (2019b) Interleukin-8 enhances myocilin expression, Akt-FoxO3 signaling and myogenic differentiation in rat skeletal muscle cells. J Cell Physiol 2019:1–16. https://doi.org/10.1002/jcp.28568
Minami M, Koyama T, Wakayama Y, Fukuhara S, Mochizuki N (2011) EphrinA/EphA signal facilitates insulin-like growth factor-I-induced myogenic differentiation through suppression of the Ras/extracellular signal-regulated kinase 1/2 cascade in myoblast cell lines. Mol Biol Cell 18:3508–3519
Modregger J, Ritter B, Witter B, Paulsson M, Plomann M (2000) All three PACSIN isoforms bind to endocytic proteins and inhibit endocytosis. J Cell Sci 113:4511–4521
Nielsen S, Åkerström T, Rinnov A, Yfanti C, Scheele C, Pedersen BK, Laye MJ (2014) The miRNA plasma signature in response to acute aerobic exercise and endurance training. PLoS One 9:e87308. https://doi.org/10.1371/journal.pone.0087308
Nystrom G, Pruznak A, Huber D, Frost RA, Lang CH (2009) Local insulin-like growth factor I prevents sepsis-induced muscle atrophy. Metabolism 58:787–797
Pasquale EB (2010) Eph receptors and ephrins in cancer: bidirectional signalling and beyond. Nat Rev Cancer 10:165–180
Pedersen BK, Febraio MA (2008) Muscle as an endocrine organ: focus on muscle-derived interleukin-6. Physiol Rev 88:1379–1406
Peltier HJ, Latham GJ (2008) Normalization of microRNA expression levels in quantitative RT-PCR assays: identification of suitable reference RNA targets in normal and cancerous human solid tissues. RNA 14:844–852
Quinlan KG, Seto JT, Turner N, Vandebrouck A, Floetenmeyer M, Macarthur DG, Raftery JM, Lek M, Yang N, Parton RG, Cooney GJ, North KN (2010) Alpha-actinin-3 deficiency results in reduced glycogen phosphorylase activity and altered calcium handling in skeletal muscle. Hum Mol Genet 19:1335–1346
Raschke S, Eckel J (2013) Adipo-myokines: two sides of the same coin – mediators of inflammation and mediators of exercise. Mediat Inflamm 2013:16. https://doi.org/10.1155/2013/320724
Rodgers BD (2005) Insulin-like growth factor-I downregulates embryonic myosin heavy chain (eMYHC) in myoblast nuclei. Growth Hormon IGF Res 15:377–383
Rosendal L, Søgaard K, Kjær M, Sjøgaard G, Langberg H, Kristiansen J (2005) Increase in interstitial interleukin-6 of human skeletal muscle with repetitive low-force exercise. J Appl Physiol 98:477–481
Rotter V, Nagaev I, Smith U (2003) Interleukin-6 (IL-6) induces insulin resistance in 3T3-L1 adipocytes and is, like IL-8 and tumor necrosis factor-alpha, overexpressed in human fat cells from insulin-resistant subjects. J Biol Chem 278:45777–45784
Sasi Kumar K, Ramadhas A, Nayak SC, Kaniyappan S, Dayma K, Radha V (2015) C3G (RapGEF1), a regulator of actin dynamics promotes survival and myogenic differentiation of mouse mesenchymal cells. Biochim Biophys Acta 1853:2629–2639
Sauer E, Babion I, Madea B, Courts C (2014) An evidence based strategy for normalization of quantitative PCR data from miRNA expression analysis in forensic organ tissue identification. Forensic Sci Int Genet 13:217–223
Sela I, Milman Krentsis I, Shlomai Z, Sadeh M, Dabby R, Argov Z, Ben-Bassat H, Mitrani-Rosenbaum S (2011) The proteomic profile of hereditary inclusion body myopathy. PLoS One 6(1):e16334. https://doi.org/10.1371/journal.pone.0016334
Senn JJ, Klover PJ, Nowak IA, Mooney RA (2002) Interleukin-6 induces cellular insulin resistance in hepatocytes. Diabetes 51:3391–3399
Shah SB, Davis J, Weisleder N, Kostavassili I, McCulloch AD, Ralston E, Capetanaki Y, Lieber RL (2004) Structural and functional roles of desmin in mouse skeletal muscle during passive deformation. Biophys J 86:2993–3008
Siegel AL, Atchison K, Fisher KE, Davis GE, Cornelison DD (2009) 3-D timelapse analysis of muscle satellite cell motility. Stem Cells 27:2527–2538
Sjöblom B, Salmazo A, Djinović-Carugo K (2008) Alpha-actinin structure and regulation. Cell Mol Life Sci 65:2688–2701
Stark DA, Karvas RM, Siegel AL, Cornelison DD (2011) Eph/ephrin interactions modulate muscle satellite cell motility and patterning. Development 138:5279–5289
Swartz ME, Eberhart J, Pasquale EB, Krull CE (2001) EphA4/ephrin-A5 interactions in muscle precursor cell migration in the avian forelimb. Development 128:4669–4680
Takei K, Slepnev VI, Haucke V, De Camilli P (1999) Functional partnership between amphiphysin and dynamin in clathrin-medited endocytosis. Nat Cell Biol 1:33–39
Tatsumi R (2010) Mechano-biology of skeletal muscle hypertrophy and regeneration: possible mechanism of stretch-induced activation of resident myogenic stem cells. Anim Sci J 81:11–20
Tidball JG (2011) Mechanisms of muscle injury, repair, and regeneration. Compr Physiol 1:2029–2062
Trayhurn P, Drevon CA, Eckel J (2011) Secreted proteins from adipose tissue and skeletal muscle - adipokines, myokines and adipose/muscle cross-talk. Arch Physiol Biochem 117:47–56
Unger A, Beckendorf L, Böhme P, Kley R, von Frieling-Salewsky M, Lochmüller H, Schröder R, Fürst DO, Vorgerd M, Linke WA (2017) Translocation of molecular chaperones to the titin springs is common in skeletal myopathy patients and affects sarcomere function. Acta Neuropathol Commun 5:72
Van Hall G, Steensberg A, Sacchetti M, Fischer C, Keller C, Schjerling P, Hiscock N, Møller K, Saltin B, Febbraio MA, Pedersen BK (2003) Interleukin-6 stimulates lipolysis and fat oxidation in humans. J Clin Endocrinol Metab 88:3005–3010
White J, Barro MV, Makarenkova HP, Sanger JW, Sanger JM (2014) Localization of sarcomeric proteins during myofibril assembly in cultured mouse primary skeletal myotubes. Anat Rec (Hoboken) 297:1571–1584
Whiteley G, Collins RF, Kitmitto A (2012) Characterization of the molecular architecture of human caveolin-3 and interaction with the skeletal muscle ryanodine receptor. J Biol Chem 287:40302–40316
Wieteska-Skrzeczyńska W, Grzelkowska-Kowalczyk K, Rejmak E (2011) Growth factor and cytokine interactions in myogenesis. Part I. The effect of TNF-alpha and IFN-gamma on IGF-I-dependent differentiation in mouse C2C12 myogenic cells. Pol J Vet Sci 14:417–424
Wilhelmsen K, Litjens SHM, Kuikman I, Tshimbalanga N, Janssen H, Van den Bout I, Raymond K, Sonnenberg A (2005) Nesprin-3, a novel outer nuclear membrane protein, associates with the cytoskeletal linker protein plectin. J Cell Biol 171:799–810
Williams AH, Liu N, van Rooij E, Olson EN (2009) MicroRNA control of muscle development and disease. Curr Opin Cell Biol 21:461–466
Yamada T, Steinz MM, Kenne E, Lanner JT (2017) Muscle weakness in rheumatoid arthritis: the role of Ca2+ and free radical signaling. EBioMedicine 23:12–19
Yang W, Hu P (2018) Skeletal muscle regeneration is modulated by inflammation. J Orthopaed Trans 13:25e32
Yin H, Price F, Rudnicki MA (2013) Satellite cells and the muscle stem cell niche. Physiol Rev 93:23–67
Funding
This study was funded by the National Science Centre Poland (grant no: 2013/09/B/NZ/00115).
Author information
Authors and Affiliations
Contributions
M.Milewska – performing experiments, microRNA qPCR and immunoblotting analyses, T.Domoradzki – qPCR analyses, wound healing assay, A.Majewska – microRNA microarray analyses, microarray data deposition at GEO data repository, M.Błaszczyk – MTT tests, phase-contrast microscopy analyses, M.Gajewska – confocal microscopy analyses, M.Hulanicka – bioinformatic analyses, K.Grzelkowska-Kowalczyk – project supervision, research design, figures and manuscript preparation. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Fig. S1
Gene ontology groups (ten-top list) in terms of protein classes, enriched in potential targets of miRNAs with expression modified by IL-6 treatment (1 ng/ml, 11 days of exposure) in rat primary muscle cells. The potential target genes were identified using TargetScan database and ontological analysis was performed using Panther Classification System (PNG 111 kb)
Fig. S2
Gene ontology groups in terms of molecular function, enriched in potential targets of miRNAs with expression modified by IL-6 treatment (1 ng/ml, 11 days of exposure) in rat primary muscle cells. The potential target genes were identified using TargetScan database and ontological analysis was performed using Panther Classification System (PNG 101 kb)
Fig. S3
Gene ontology groups (ten-top list) in terms of involvement in biological processes, enriched in potential targets of miRNAs with expression modified by IL-6 treatment (1 ng/ml, 11 days of exposure) in rat primary muscle cells. The potential target genes were identified using TargetScan database and ontological analysis was performed using Panther Classification System (PNG 146 kb)
Table S1
List of potential target genes of miR-154-3p and miR-338-3p. Target genes for two miRNA species separately were identified using TargetScan database. Then, two lists of genes were combined, repeating inputs and inputs indicated as „uncharacterized protein”, were removed and remained set of genes was further analyzed using Panther Classification System. These genes are listed in alphabetical order and their functional classification to GO categories: Panther Family/Subfamily and Panther Protein Class are presented (XLSX 408 kb)
Table S2
Lists of genes which contribute to selected gene ontology categories associated with cytoskeleton organization and cell migration. Presented sets of genes were retrieved during ontological analysis in Panther Classification System. Subsequent sheets include: Structural constituent of cytoskeleton (GO:0005200), Cellular component organization or biogenesis (GO:0071840), Locomotion (GO:0040011) Actin family cytoskeletal protein (GO Protein Class: PC00041), Microtubule family cytoskeletal protein (GO Protein Class: PC00157) Intermediate filament binding protein (GO Protein Class: PC00129). (XLSX 72 kb)
Table S3
Panther statistical overrepresentation test of potential targets for miR-154-3p and miR-338-3p. The results are sorted by Fold enrichment value of GO categories and only records for FDR (False Discovery Rate) P<0.05 are presented (XLSX 16 kb)
Rights and permissions
About this article
Cite this article
Milewska, M., Domoradzki, T., Majewska, A. et al. Interleukin-6 affects pacsin3, ephrinA4 expression and cytoskeletal proteins in differentiating primary skeletal myoblasts through transcriptional and post-transcriptional mechanisms. Cell Tissue Res 380, 155–172 (2020). https://doi.org/10.1007/s00441-019-03133-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-019-03133-4