Abstract
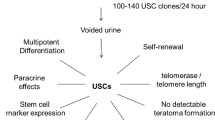
Tissue-engineered urethra with autologous cells seeded on biodegradable scaffolds offers an alternative for lower urinary tract reconstruction. Rabbit is most commonly used as an animal model in urethra and bladder tissue repair. The goal of this study is to characterize rabbit urine-derived stem cells (rUSC) and induce these cells to differentiate into urothelial and smooth muscle cells as an autologous cell source for potential use in lower urinary tract tissue regeneration in a rabbit model. We successfully cultured rUSC from 12 urine samples and 13 bladder wash samples of six rabbits. rUSC colonies appeared more in the bladder wash solution (2–4/15 ml) than those in the urine samples (1–2 clones/15 ml urine). The cells displayed rice grain-like in morphology. Mean population doubling of rUSC was 48.5 ± 6.2 and average doubling time was 25.7 ± 8.4 h, indicating that a single of rUSC clone generated about 4 × 1014 cells in 50 days. The rUSC were positive for CD29, CD90 and CD105 but negative for CD31, CD34 and CD45 in flow cytometry. When exposed to PDGF-BB and TGF-β1, these cells could differentiate into spindle-like cells, expressing smooth muscle-specific proteins, including α-smooth muscle action, desmin and myosin. Urothelially differentiated rUSC expressed urothelial-specific proteins, i.e., AE1/AE3 and E-cadherin when exposed to epidermal growth factor (EGF). Osteogenic-differentiated rUSC expressed osteogenic marker, i.e., alkaline phosphatase when exposed to serum containing DMEM low-glucose medium with osteogenic supplements. In conclusion, rUSC can be isolated from bladder wash or urine samples and cultured in vitro. There stem cells possess strong proliferative ability and are capable of differentiating in urothelial, myogenic and osteogenic lineages. Thus, rUSC are a potential alternative autologous cell source for lower urinary tract repair with tissue engineering technology in a rabbit model.









Similar content being viewed by others
References
Atala A, Bauer SB, Soker S, Yoo JJ, Retik AB (2006) Tissue-engineered autologous bladders for patients needing cystoplasty. Lancet 367:1241–1246
Bharadwaj S, Liu G, Shi Y, Markert C, Andersson KE, Atala A, Zhang Y (2011) Characterization of urine-derived stem cells obtained from upper urinary tract for use in cell-based urological tissue engineering. Tissue Eng Part A 17:2123–2132
Bharadwaj S, Liu G, Shi Y, Wu R, Yang B, He T, Fan Y, Lu X, Zhou X, Liu H, Atala A, Rohozinski J, Zhang Y (2013) Multipotential differentiation of human urine-derived stem cells: potential for therapeutic applications in urology. Stem Cells 31:1840–1856
Bodin A, Bharadwaj S, Wu S, Gatenholm P, Atala A, Zhang Y (2010) Tissue-engineered conduit using urine-derived stem cells seeded bacterial cellulose polymer in urinary reconstruction and diversion. Biomaterials 31:8889–8901
Dong X, Zhang T, Liu Q, Zhu J, Zhao J, Li J, Sun B, Ding G, Hu X, Yang Z, Zhang Y, Li L (2016) Beneficial effects of urine-derived stem cells on fibrosis and apoptosis of myocardial, glomerular and bladder cells. Mol Cell Endocrinol 427:21–32
Dublin N, Stewart LH (2004) Oral complications after buccal mucosal graft harvest for urethroplasty. BJU Int 94:867–869
Fu Y, Guan J, Guo S, Guo F, Niu X, Liu Q, Zhang C, Nie H, Wang Y (2014) Human urine-derived stem cells in combination with polycaprolactone/gelatin nanofibrous membranes enhance wound healing by promoting angiogenesis. J Transl Med 12:274
Guan JJ, Niu X, Gong FX, Hu B, Guo SC, Lou YL, Zhang CQ, Deng ZF, Wang Y (2014) Biological characteristics of human-urine-derived stem cells: potential for cell-based therapy in neurology. Tissue Eng Part A 20:1794–1806
Guan J, Zhang J, Guo S, Zhu H, Zhu Z, Li H, Wang Y, Zhang C, Chang J (2015a) Human urine-derived stem cells can be induced into osteogenic lineage by silicate bioceramics via activation of the Wnt/beta-catenin signaling pathway. Biomaterials 55:1–11
Guan J, Zhang J, Zhu Z, Niu X, Guo S, Wang Y, Zhang C (2015b) Bone morphogenetic protein 2 gene transduction enhances the osteogenic potential of human urine-derived stem cells. Stem Cell Res Ther 6:5
Lang R, Liu G, Shi Y, Bharadwaj S, Leng X, Zhou X, Liu H, Atala A, Zhang Y (2013) Self-renewal and differentiation capacity of urine-derived stem cells after urine preservation for 24 hours. PLoS One 8:e53980
Lee JN, Chun SY, Lee HJ, Jang YJ, Choi SH, Kim DH, Oh SH, Song PH, Lee JH, Kim JK, Kwon TG (2015) Human urine-derived stem cells seeded surface modified composite scaffold grafts for bladder reconstruction in a rat model. J Korean Med Sci 30:1754–1763
Liu G, Pareta RA, Wu R, Shi Y, Zhou X, Liu H, Deng C, Sun X, Atala A, Opara EC, Zhang Y (2013a) Skeletal myogenic differentiation of urine-derived stem cells and angiogenesis using microbeads loaded with growth factors. Biomaterials 34:1311–1326
Liu G, Wang X, Sun X, Deng C, Atala A, Zhang Y (2013b) The effect of urine-derived stem cells expressing VEGF loaded in collagen hydrogels on myogenesis and innervation following after subcutaneous implantation in nude mice. Biomaterials 34:8617–8629
Liu G, Pareta R, Wu R, Shi Y, Deng C, Zhou X, Atala A, Opara EC, Zhang Y (2015) Skeletal myogenic differentiation of urine-derived stem cells, angiogenesis and innervation using hydrogel loaded with growth factors for potential in treatment of urinary incontinence. J Urol 193:e74
Liu Y, Ma W, Liu B, Wang Y, Chu J, Xiong G, Shen L, Long C, Lin T, He D, Butnaru D, Alexey L, Zhang Y, Zhang D, Wei G (2017) Urethral reconstruction with autologous urine-derived stem cells seeded in three-dimensional porous small intestinal submucosa in a rabbit model. Stem Cell Res Ther 8:63
Ouyang B, Sun X, Han D, Chen S, Yao B, Gao Y, Bian J, Huang Y, Zhang Y, Wan Z, Yang B, Xiao H, Songyang Z, Liu G, Zhang Y, Deng C (2014) Human urine-derived stem cells alone or genetically-modified with FGF2 improve type 2 diabetic erectile dysfunction in a rat model. PLoS One 9:e92825
Qin D, Long T, Deng J, Zhang Y (2014a) Urine-derived stem cells for potential use in bladder repair. Stem Cell Res Ther 5:69
Qin H, Zhu C, An Z, Jiang Y, Zhao Y, Wang J, Liu X, Hui B, Zhang X, Wang Y (2014b) Silver nanoparticles promote osteogenic differentiation of human urine-derived stem cells at noncytotoxic concentrations. Int J Nanomedicine 9:2469–2478
Sainio K, Raatikainen-Ahokas A (1999) Mesonephric kidney—a stem cell factory? Int J Dev Biol 43:435–439
Tran C, Tangada A, Balog B, Zhang Y, Damaser M (2015) Paracrine effects of human urine-derived stem cells in treatment of female stress urinary incontinence in a rodent model. Tissue Eng Part A 21:S-385
Wu S, Liu Y, Bharadwaj S, Atala A, Zhang Y (2011) Human urine-derived stem cells seeded in a modified 3D porous small intestinal submucosa scaffold for urethral tissue engineering. Biomaterials 32:1317–1326
Wu RP, Liu G, Shi YA, Bharadwaj S, Atala A, Zhang Y (2014) Human urine-derived stem cells originate from parietal stem cells. J Urol 191:e1–e958
Yang Q, Chen X, Zheng T, Han D, Zhang H, Shi Y, Bian J, Sun X, Xia K, Liang X, Liu G, Zhang Y, Deng C (2016) Transplantation of human urine-derived stem cells transfected with pigment epithelium-derived factor to protect erectile function in a rat model of cavernous nerve injury. Cell Transplant 25:1987–2001
Zhang Y, Kropp BP, Moore P, Cowan R, Furness PD 3rd, Kolligian ME, Frey P, Cheng EY (2000) Coculture of bladder urothelial and smooth muscle cells on small intestinal submucosa: potential applications for tissue engineering technology. J Urol 164:928–934 discussion 934-925
Zhang Y, McNeill E, Tian H et al (2008) Urine derived cells are a potential source for urological tissue reconstruction. J Urol 180:2226–2233
Zhang D, Wei G, Li P, Zhou X, Zhang Y (2014) Urine-derived stem cells: a novel and versatile progenitor source for cell-based therapy and regenerative medicine. Genes Dis 1:8–17
Zhang D, Chu J, Ma W, Gong M, Wei G, Zhang Y (2015) Urine-derived stem cells for potential use in treatment of urethral sphincter dysfunction. Int J Stem Cell Res 1. https://doi.org/10.16966/ijscr.16105
Acknowledgements
The authors acknowledge funding support from the National Natural Science Foundation of China (No. 81570650 and No. 81371704).
Author information
Authors and Affiliations
Contributions
Administrative support: HY.
Editorial help: DC, DJ and YYZ.
Conceived and designed the experiments: YYZ.
Performed the experiments: BC, GZ and LG.
Analyzed the data: CD, DJ, SW, PW, XW and YYZ.
Contributed reagents/materials/analysis tools: HY.
Writing the paper: BC, GL and YYZ.
Corresponding authors
Ethics declarations
The protocol for collection of human urine samples from healthy donors was approved by the Wake General Hospital of Guangzhou Military Area (GHGMA) Institutional Review Board. The study protocol conforms to the ethical guidelines of the Declaration of Helsinki. Written informed consent was obtained from the urine donors. Experiments in rabbit were approved by the Animal Care and Use Committee at GHGMA. All the animal experiments were conducted in accordance with guidelines of the international committee of use of laboratory animals.
Competing interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Yang, H., Chen, B., Deng, J. et al. Characterization of rabbit urine-derived stem cells for potential application in lower urinary tract tissue regeneration. Cell Tissue Res 374, 303–315 (2018). https://doi.org/10.1007/s00441-018-2885-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-018-2885-z