Abstract
Single nucleotide variants (SNVs) within and surrounding the complement receptor 1 (CR1) gene show some of the strongest genome-wide association signals with late-onset Alzheimer’s disease. Some studies have suggested that this association signal is due to a duplication allele (CR1-B) of a low copy repeat (LCR) within the CR1 gene, which increases the number of complement C3b/C4b-binding sites in the mature receptor. In this study, we develop a triplex paralogue ratio test assay for CR1 LCR copy number allowing large numbers of samples to be typed with a limited amount of DNA. We also develop a CR1-B allele-specific PCR based on the junction generated by an historical non-allelic homologous recombination event between CR1 LCRs. We use these methods to genotype CR1 and measure CR1-B allele frequency in both late-onset and early-onset cases and unaffected controls from the United Kingdom. Our data support an association of late-onset Alzheimer’s disease with the CR1-B allele, and confirm that this allele occurs most frequently on the risk haplotype defined by SNV alleles. Furthermore, regression models incorporating CR1-B genotype provide a better fit to our data compared to incorporating the SNV-defined risk haplotype, supporting the CR1-B allele as the variant underlying the increased risk of late-onset Alzheimer’s disease.
Similar content being viewed by others
Introduction
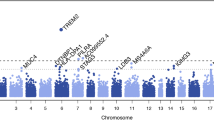
Alzheimer’s disease (AD) is a common neurodegenerative disease with an increasing disease burden in an aging population (Ballard et al. 2011). Familial early-onset AD can be caused by autosomal dominant variants in, for example, the amyloid precursor protein gene APP, the presenilin 1 gene PSEN1, and the presenilin 2 gene PSEN1 (Campion et al. 1999). Sporadic early onset AD (EOAD), with an age-of-onset of 65 years or less, is defined as disease in the absence of these classical familial early-onset AD mutations. However, 99% of AD cases are late-onset AD (LOAD), which is a complex disease with multiple environmental and genetic contributions to its etiology. The most important genetic variant affecting LOAD risk is the APOE*4 allele, which is a haplotype formed by rs429358-C and rs7412-C, generating a protein called apolipoprotein E4 (APOE4) carrying arginine residues at position 130 and position 176 (Corder et al. 1993, 1998). This variant is associated with a 2–3-fold increase in LOAD risk for carriers, and a 15-fold increase in risk for individuals homozygous for this variant (Farrer et al. 1997). Genome-wide association studies (GWAS) on large cohorts have robustly identified 23 other variants with smaller effect sizes (Lambert et al. 2009, 2013). Many of the genetic associations are with variants that lie within or near genes involved in the immune response. This has highlighted the importance of the immune response to amyloid plaque formation in Alzheimer’s disease, possibly mediated by microglial cells (Efthymiou and Goate 2017; Naj and Schellenberg 2017; Villegas-Llerena et al. 2016).
One of the genes implicated in LOAD risk by GWAS is the complement C3b/C4b receptor 1 gene CR1. The receptor encoded by this gene is expressed on the surface of leukocytes and erythrocytes, and binds the C3b fragment of complement C3, and the C4b fragment of complement C4, as well as complement C1q. These interactions are important in the clearance of antibody-antigen immune complexes from the blood circulation, and in the phagocytosis of complement-tagged pathogens. Complement receptor 1 is also involved in the inflammatory response to injured tissue (Holers 2014).
Alleles at several SNVs both proximal, distal and within the CR1 gene have been identified as associated with LOAD, and these alleles are on a single risk haplotype that spans the CR1 gene (Corneveaux et al. 2010; Lambert et al. 2009; Luo et al. 2014). Identifying the variant within this haplotype that is functionally responsible for the genetic association is challenging, yet correct identification will allow a functional genetic approach to determine the consequences of the variation in CR1 function and, therefore, how that variation contributes to LOAD risk. As previously observed, there are at least 60 missense variants within the risk haplotype (Corneveaux et al. 2010). and it has been suggested that a rare missense variant rs4844609 might be responsible for the observed association (Keenan et al. 2012) but this observation has not been supported (Van Cauwenberghe et al. 2013).
CR1 is known to contain an intragenic copy number variant (CNV) that alters the number of exons while maintaining the reading frame of the protein. The copy number variant is due to variable numbers of a tandemly arranged 18 kb repeat unit called a low copy repeat (LCR) (Crehan et al. 2012; Vik and Wong 1993; Wong et al. 1989; Wong et al. 1983). Each LCR contains eight exons, which together encode a C3b/C4b binding domain such that high copy numbers of the LCR result in a longer CR1 molecule with more C3b/C4b binding domains (Fig. 1). The CR1 CNV has four alleles: CR1-A with two LCRs, CR1-B with three LCRs, CR1-C with one LCR and CR1-D with four LCRs. Each allele can be, therefore, represented by the copy number of the LCR domains. Alleles CR1-A, CR1-B and CR1-C are also known as CR1-F, CR1-S and CR1-F′, respectively, in the literature, based on their mobilities in protein electrophoresis. Previous studies have shown that CR1-A is the most frequent allele in individuals of European origin with a frequency of 0.87. CR1-B is the next most frequent, at a frequency of 0.11, with CR1-C and CR1-D at frequencies of 0.02 and < 0.01, respectively (Moulds et al. 1996).
Structure of the human CR1 and CR1L region showing the different CNV alleles. The CR1 and CR1L genes are shown, with SNVs that have been reported as associated with late-onset Alzheimer’s disease in GWAS shown in green. The duplicated structure of the region is shown, with pale/dark orange boxes showing repeated regions that are ~ 92% similar between CR1 and CR1L, and pale/dark blue boxes showing the LCR regions that are ~ 99% similar. The genome assembly shows a CR1-B allele, comprised of LCR1, LCR2 and LCR1′ which is a fusion of LCR2 and LCR1. The structure of the alternative alleles (CR1-A, CR1-C and CR1-D) are shown below, with hatching indicating unclear origin of the LCR. The location of the amplification products for the three PRT assays are indicated, with the test amplicons generated from the pale orange CR1 repeats, and the reference amplicons generated from the dark orange CR1L repeat. Based in part on the UCSC Genome browser hg38 assembly
Although the CR1 LCR CNV affects protein sequence quite dramatically, it is not directly assayed by current GWAS. Nevertheless, the association signal observed with SNV haplotypes might be due to a CR1 LCR CNV allele if that allele was on that particular SNV haplotype and, therefore, in linkage disequilibrium with the SNV alleles that show association with LOAD. A previous study tested the association of the CR1-B allele with LOAD on a cohort of Flemish Belgian patients (n = 1039) and controls (n = 844), and showed that CR1-B carriers showed an increased risk of LOAD (OR 1.32, 95% CI 1.03–1.69, p = 0.028). They replicated their result on a sample of French patients (n = 1393) and controls (n = 610) (OR = 1.33, 1.02–1.74, p = 0.039), and showed that this represented the same association signal as that for the SNVs rs4844610 and rs1408077 (Brouwers et al. 2012).
Our study aimed first to develop a robust assay based on the paralogue ratio test and junction-fragment PCR for CR1 LCR CNV, in particular for the intragenic duplication allele CR1-B, to facilitate further studies. Second, we aimed to use our methods to replicate the previous association of CR1 and LOAD in a larger cohort. We also investigate the association of CR1-B in a cohort of EOAD to test for a stronger risk effect as a result of a more pronounced phenotype.
Methods
Samples
Lymphoblastoid cell lines derived from the 1000 Genomes project samples (Coriell Cell Repositories, Camben, NJ) were grown using the standard conditions recommended by the supplier, and DNA isolated using a standard phenol–chloroform-based approach. UK samples were purchased as part of Human Random Controls plate 1 (HRC-1) from Public Health England.
Human DNA samples were obtained from the Alzheimer’s Research Trust (ART) Collaboration [University of Nottingham; University of Manchester; University of Southampton; University of Bristol; Queen’s University, Belfast; the Oxford Project to Investigate Memory and Ageing (OPTIMA), Oxford University]; All case samples were diagnosed as either definite (post mortem confirmed) or probable Alzheimer’s disease (AD) according to National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association (NINCDS-ADRDA), and the Consortium to Establish a Registry for Alzheimer’s Disease (CERAD) guidelines. All samples used in this study were received with informed consent and were approved by the local Ethics Committee.
The 449 sporadic EOAD samples had an age of disease onset (AAO) ≤ 65 years of age, the 1436 LOAD samples had an AAO > 65 years of age and the 1359 controls had an age at death (AAD) > 65 years of age. Where AAO was not documented, it was derived assuming 8 years disease duration from age at death (Brookmeyer et al. 2002), or age at sampling (AAS) was used with the understanding it would approximate to disease onset (Tables 1, 3).
DNA was extracted from blood or brain tissue using a standard phenol chloroform extraction method. DNA quality and quantity was assessed via gel electrophoresis and NanoDrop™ 3300 spectrometer, respectively.
CR1 copy number estimation from sequence read depth data
Sequence alignment files in .bam format and corresponding index files in .bai format were downloaded from the European Bioinformatics Institute (ftp.1000genomes.ebi.ac.uk/vol1/ftp/data_collections/1000_genomes_project/). Using samtools software (using the command samtools view -c -F 4 input.bam target_region), the number of mapped reads was counted across two intervals (GRCh37 chr1:207, 697, 239–207, 751, 921 test region, GRCh37 chr1:207, 953, 949–208, 008, 574 reference) for each of the samples analysed as part of the 1000 Genomes project (CEU individuals for Salt Lake City, Utah, Chinese individuals from Beijing, Japanese individuals for Tokyo and Yoruba individuals from Ibadan, Nigeria). A ratio of the reads from the copy number variable region:non-copy number variable region was taken as an estimate of CR1 intragenic copy number. Data are available in dbvar accession nstd159 at ncbi.nlm.nih.gov/dbvar.
CR1 paralogue ratio test
To determine CR1 intragenic copy number on large numbers, we decided to design three specific assay using the paralogue ratio test (PRT), a form of competitive PCR that amplifies a test and reference locus using common primers, and uses the ratio of test and reference amplification products as a measure of copy number (Armour et al. 2007; Hollox 2017) (Supplementary Table 1). For each PCR, 5–10 ng genomic DNA was amplified in a final volume of 10 µl, containing 0.5 units Taq DNA polymerase (KAPA), 0.5 µl of 10 µM forward primer, 0.5 µl of 10 µM reverse primer and 1 µl of 10xPCR mix (10xPCR mix = 50 mM TrisHCl pH8.8@25 °C, 12.5 mM ammonium sulphate, 1.4 mM MgCl2, 125 µg/ml BSA (Ambion), 7.5 mM 2-mercaptoethanol and each dNTP (Promega) at a concentration of 200 µM). Following PCR amplification in an Applied Biosystems Veriti thermal cycler at 95 °C for 2 min, followed by between 24 and 27 cycles of 95 °C for 20 s, 61–63 °C for 20 s and 72 °C for 20 s, and finally an elongation step at 72 °C for 10 min. Cycle number and annealing temperatures for each assay are given in supplementary Table 1.
Between 0.5 and 1 µl of the final product from each assay was combined and added to HiDi Formamide (Applied Biosystems) containing 1% MapMarker ROX-labelled size standard. Following denaturation of the mixture at 96 °C for 3 min and snap cooling on ice, the products were run on an Applied Biosystems 3130xl capillary sequencer following the manufacturer’s instructions, and areas of the test and reference peaks recorded using Genemapper software. For each assay, seven samples of known CR1 LCR copy number were analysed with each experiment (Supplementary Table 2). These samples were chosen from the HapMap phase I panel, with copy number inferred from previous array CGH data (Conrad et al. 2009) or from preliminary experiments with multiple PRTs. PRT values were normalised using the values from the seven positive controls to generate an estimated copy number value.
Calling integer copy number from CR1 PRT data
Data from PRT1, PRT2 and PRT3 were concordant across the 1000 Genomes samples analysed so an average was taken to represent copy number, and normalised so that the standard deviation of the data was 1. For each cohort, a Gaussian mixture model of four or five components was fitted to the data using the CNVtools software implemented in the statistical language R v.3.2.3, with each component representing a integer copy number class (Barnes et al. 2008). Samples were then assigned to each component with a posterior probability, and the component to which they were assigned reflected integer copy number call. A statistic Q, which is defined as the ratio of the separation of adjacent component means divided by the within-component standard deviation, averaged across all components of the mixture model, was calculated for each cohort. This represents the degree of clustering of the raw normalised data about integer copy number values (Barnes et al. 2008). PRT data from the 1000 Genomes samples analysed is available at dbvar accession nstd159 at ncbi.nlm.nih.gov/dbvar.
CR1 junction fragment analysis
PCR products were amplified from 5 to 10 ng genomic DNA in a final volume of 10ul, with 0.5 µl of 2.5 mM of each of dATP, dCTP, dGTP and dTTP, 0.5 units Taq DNA polymerase (KAPA Biosciences) and 0.5 µl of a 10 µM solution of each PCR primer. The PCR primers were 5′-AATGTGTTTTGATTTCCCAAGATCAG-3′ and 5′-CTCAACCTCCCAAAGGTGCTA-3′, with a terminal 3′ locked nucleic acid base (underlined) to increase paralogue-specificity (Latorra et al. 2003). A touch-down PCR protocol was used, with an initial denaturation step of 95 °C for 2 min, followed by 20 cycles of 95 °C for 30 s, 70 °C for 30 s decreasing by 0.5 °C every cycle to 60 °C, and 70 °C for 30 s. These 20 cycles were then followed by 15 cycles of 95 °C for 30 s, 60 °C for 30 s and 70 °C for 30 s, then a final extension step of 70 °C for 5 min. Products were analysed using standard ethidium bromide stained agarose gels and visualisation under ultraviolet light. Specificity of the PCR for CR1-B alleles was confirmed on a panel of 40 UK samples from the HRC-1 collection previously typed using PRT.
SNP genotyping and linkage disequilibrium analysis
Genotyping for the CR1 GWAS index SNP (Lambert et al. 2013), rs6656401, and rs3818361 was carried out using KASP assays using standard protocols (LGC, Middlesex). Pairwise linkage disequilibrium was calculated using a cubic exact equation approach implemented in CubeX (Gaunt et al. 2007).
Statistical analysis and sequence alignment
Clustal Omega was used for sequence alignment provided by the European bioinformatics Institute web server (www.ebi.ac.uk), using default DNA options (Li et al. 2015; Sievers et al. 2011). Case–control analysis was performed using logistic regression implemented in the statistical package RStudio v.1.0 implementing R v3.2.3.
Results
Development and validation of PRT assays for CR1 copy number
Our first aim was to develop a simple robust approach to determine the diploid copy number of the LCRs within the CR1 gene, which could use small amounts of DNA from large clinical cohorts. The 92% similarity between the LCRs within CR1 and part of the CR1L gene allowed the design of three PRT assays to independently measure the copy number of LCR (Fig. 2a).
Design and validation of paralogue ratio test to detect CR1 LCR copy number. a Measuring copy number using the paralogue ratio test. A primer pair is designed so that it amplifies from the LCR regions (test) and also from a 92% similar region in CR1L (reference). Three independent tests are normalised against seven controls of known copy number, and average to obtain an estimate of copy number. b Comparison of CR1 PRT copy number estimate (x axis and histogram) against estimates from Illumina sequence read depth (y axis and histogram). Each point represents a different individual, points are distinguished by shape and colour indicating the final integer copy number call: red cross—3, green x-cross—4, blue diamond—5, cyan triangle—6
Analysis of 275 samples from the 1000 Genomes collection showed high pairwise concordance (~ 80%) pairwise between the three individual PRT results, allowing an average to be taken of the three PRT results for each sample as representative of the copy number of the LCR. For each sample, the copy number estimate from the PRT was compared against the copy number estimated from Illumina sequencing read depth data. The data showed a high degree of concordance, with data for both estimates clustering around integer copy number estimates. In particular, the PRT data shows clear distinct clusters, suggesting that it will call copy number accurately (Fig. 2b).
Because our study was focused on the CR1-B duplication, distinguishing the CR1-A/CR1-B heterozygotes (diploid LCR copy number 5) from the CR1-A/CR1-A homozygotes (diploid LCR copy number 4) was particularly critical. To improve the reliability of distinguishing these genotypes, we developed a junction fragment PCR to specifically amplify the LCR1′ repeat. If the LCR1′ repeat was generated in the past by an equal crossover between the 98% identical LCR1 and LCR2 sequences, we would expect a switch from LCR1-like sequence to LCR2-like sequence within the LCR1′ sequence (Fig. 3). Using a multiple alignment strategy on LCR1, LCR1′ and LCR2 sequences from the human reference genome GRCh37, we identified the switch point and confirmed that this is the same switch point found in early characterisations of the CR1-B allele (Vik and Wong 1993). Designing PCR primers flanking the switch point, with a forward PCR primer specific to the LCR2 sequence and a reverse PCR primer specific to the LCR1 will generate an amplification product from CR1-B alleles but not from CR1-A alleles (Fig. 3).
Association analysis of the CR1-B allele with Alzheimer’s disease
We typed 449 EOAD cases and 184 controls for copy number using our PRT approach (Table 1), resulting in a dataset that showed clear clustering around integer copy numbers and good separation of clusters (Fig. 4a). The Q value, a measure of clustering quality of the resulting data, was 5.56, above the minimum threshold of 4 previously suggested to be adequate for case–control studies (Barnes et al. 2008). By calling the individuals with LCR diploid copy numbers of 5 and 6 (CR1-B heterozygotes and CR1-B homozygotes, respectively), we could infer CR1-B allele dose for each individual. We then used logistic regression with sex and ApoE*4 genotype as covariates to test for the association of CR1-B allele with EOAD, assuming an additive effect of the allele. We found no evidence of association (p = 0.936, Table 2).
Distributions of PRT copy number data. Histograms showing the distribution of copy number values generated by PRT in a early onset cases and controls and b late onset cases and controls. X axis represents normalised PRT ratio, with Gaussian curves superimposed to indicate the calling of CR1 LCR integer copy number, from left to right: black—3 copies, green 4 copies, cyan, 5 copies, yellow 6 copies and black (right hand side) > 6 copies
We then typed 1436 LOAD cases and 1175 controls for copy number using our PRT approach (Table 3). The Q value for this cohort was lower (Q = 4.05), and this is reflected in the clustering of values (Fig. 4b), where there is significant overlap between copy number clusters. To improve calling of copy numbers 4 and 5 (i.e. CR1-B heterozygotes and homozygotes) the junction fragment PCR assay was also used on the LOAD cohort. We used logistic regression with sex, age and APOE*4 genotype as covariates to test for the association of CR1-B allele with LOAD, assuming an additive effect of the allele (Table 4). We confirmed the effect of APOE*4 allele on increasing LOAD risk (p < 2 × 10−16, odds ratio 3.25, 95% confidence intervals for odds ratio 2.78, 3.82), and evidence of association of the CR1-B allele with an increased risk of LOAD (p = 0.0151, odds ratio 1.21, 95% confidence intervals for odds ratio 1.04, 1.42).
Relationship of CR1-B with flanking SNV alleles
We next attempted to address whether the association we see explains the association at SNVs flanking the CR1 gene seen in genome-wide association studies. The strength of effect that we observe for the CR1-B allele (odds ratio 1.21, 1.04–1.42 95% CI) is consistent with the effect seen for rs6701713-A allele [odds ratio 1.16, 1.11–1.22 95% CI, (Naj et al. 2011)] and rs3818361-T allele [odds ratio 1.18, 1.13–1.24 95% CI, (Hollingworth et al. 2011)]. We analysed the pairwise linkage disequilibrium between these two SNVs in a subset of the LOAD cohort (526 cases, 101 controls). We found complete linkage disequilibrium (D′ = 1, r2 = 1) between rs6701713 and rs3818361, indicating an A–T risk haplotype and a G–C non-risk haplotype, similar to previous findings (Mahmoudi et al. 2015). Linkage disequilibrium between both SNVs and CR1-B showed LD (D′ = 0.806, r2 = 0.576) with the CR1-B allele. The CR1-B allele occurred on the A–T risk haplotype (CR1B-rs6701713A- rs3818361T haplotype frequency 0.16) with CR1-B on the non-risk haplotype (CR1B-rs6701713G- rs3818361C) infrequent at a frequency of 0.03. This pattern of LD is consistent with the CR1-B allele explaining the association observed at the flanking SNP alleles.
If the association of LOAD with the CR1-B allele explains the association at flanking SNP alleles then we would expect a stronger association of disease with the CR1 duplication compared to the SNP alleles. We analysed a subset of our cohort that had genotypes for rs6701713 and rs3818361 as well as CR1-B genotype, using the same model used to analyse the full LOAD cohort. Due to limited DNA availability, this subset was small (478 cases and 96 controls) and underpowered to detect evidence for an association a priori. Nevertheless, the association with CR1-B was stronger (p = 0.067, OR 1.52, 95% CI 0.99–2.44) than with either rs6701713A or rs3818361T (p = 0.56, OR = 1.13 95% CI 0.76–1.72), and incorporating CR1-B rather than rs6701713A or rs3818361T into the logistic regression model provides a better fit to the data (Akaike’s information criterion = 469.99 vs 473.26).
Discussion
In this study, we develop a new approach to measuring the copy number variation (CNV) of LCRs within the CR1 gene using the paralogue ratio test (PRT), together with a junction fragment PCR specific for the CR1-B allele that carries three copies of the LCR. Accurate typing of multiallelic CNV at a large scale can be challenging (Cantsilieris et al. 2014) and two other approaches have been developed to measure this particular CNV. One approach uses multiplex amplicon quantification (Brouwers et al. 2012), and the other uses a PRT approach with a reference amplicon within LCR2 of the CR1 gene and a test amplicon within LCR1 of the CR1 gene, distinguished by sequence variants, and quantifying the amounts of test amplicon using DNA duplex melting profiles (Kisserli et al. 2017). A large scale comparison between these approaches has not yet been made, but by making our PRT data publically available on some 1000 Genomes DNA samples, which are themselves publically available, we hope to facilitate a comparison between these methods.
Using our PRT and junction fragment PCR approaches, we typed a case–control cohort of early-onset Alzheimer’s disease and a case–control cohort of late-onset Alzheimer’s disease for copy number of the LCR within the CR1 gene, inferring the CR1-B genotype. An association study of the CR1-B allele with EOAD showed no evidence of association, but an association study of the CR1-B allele with LOAD provided evidence of association of the CR1-B allele with increased LOAD risk, in agreement with previous studies. We also show that the CR1-B allele is on the LOAD risk haplotype identified by SNV-based GWAS, and that the CR1-B allele shows stronger evidence of association with LOAD than the risk SNV alleles identified by GWAS.
One limitation of the PRT approach, a limitation also shared by the two other methods mentioned above, is that it reports diploid copy number—i.e., the copy number summed over both alleles, rather than the true genotype. So, for example, a copy number of 5 could be a 3 allele and a 2 allele, or a 4-1 or a 5-0. We assumed that all 5 copy individuals were 3-2, that is CR1-B/CR1-A and all 6 copy individuals were 3-3 CR1-B/CR1-B not 4-2 CR1-A/CR1-D. This could be an incorrect assumption leading to an overestimation of the frequency of the CR1-B allele. Previous work has shown, by western blotting of the CR1 protein, that in three out of eight individuals the true genotype was CR1-A/CR1-D not CR1-B/CR1-B, suggesting that a significant proportion of 6 copy individuals may not be homozygous for CR1-B as we assume (Brouwers et al. 2012). To assess the validity of our assumption in our population, we estimated the population allele frequencies from the diploid copy number data of the EOAD cohort using the R script CNVice, which simultaneously tests for any departure of the inferred genotype frequencies from Hardy–Weinberg equilibrium (Zuccherato et al. 2017). The relative probability of a genotype given the individual’s copy number was also calculated from these results. We found that 4-copy individuals had a 99.2% probability of being CR1-A homozygotes, 5-copy individuals had a 100% probability of being CR1-A/CR1-B heterozygotes and 6-copy individuals had a 100% probability of being CR1-B homozygotes, supporting our assumptions used in this study.
Although complement appears to have an important role in brain development and pathology, the mechanistic basis for the association of the CR1-B allele with LOAD remains unclear (Morgan 2018). From RNA-seq analysis, the CR1 gene is mainly expressed in peripheral blood leucocytes and the spleen (Lappalainen et al. 2013) but the CR1 protein is also detected in the brain, probably restricted to astrocytes (Fonseca et al. 2016; Gasque et al. 1996). It has been suggested that, because of its extra C3b-binding site, the CR1-B protein is more effective at inhibiting C3b complement fragments, leading to a reduction in C3b-mediated opsonisation of Ab1-42 fragments (Brouwers et al. 2012). However, in the brain the CR1-B isoform is expressed at lower levels than CR1-A and is probably associated with increased complement activation; indeed, complement system is activated by Ab (Hazrati et al. 2012; Mahmoudi et al. 2015; Rogers et al. 1992). Future studies need to focus on the functional effect of CR1-B allele in vivo, in combination with structural studies to determine the difference in protein structure encoded by the different CR1 alleles.
References
Armour JAL, Palla R, Zeeuwen PLJM, den Heijer M, Schalkwijk J, Hollox EJ (2007) Accurate, high-throughput typing of copy number variation using paralogue ratios from dispersed repeats. Nucleic Acids Res 35:e19–e25
Ballard C, Gauthier S, Corbett A, Brayne C, Aarsland D, Jones E (2011) Alzheimer’s disease. Lancet 377:1019–1031. https://doi.org/10.1016/s0140-6736(10)61349-9
Barnes C, Plagnol V, Fitzgerald T, Redon R, Marchini J, Clayton D, Hurles ME (2008) A robust statistical method for case-control association testing with copy number variation. Nat Genet 40:1245–1252
Brookmeyer R, Corrada MM, Curriero FC, Kawas C (2002) Survival following a diagnosis of Alzheimer disease. Arch Neurol 59:1764–1767
Brouwers N, Van Cauwenberghe C, Engelborghs S, Lambert JC, Bettens K, Le Bastard N, Pasquier F, Montoya AG, Peeters K, Mattheijssens M, Vandenberghe R, Deyn PP, Cruts M, Amouyel P, Sleegers K, Van Broeckhoven C (2012) Alzheimer risk associated with a copy number variation in the complement receptor 1 increasing C3b/C4b binding sites. Mol Psychiatry 17:223–233. https://doi.org/10.1038/mp.2011.24
Campion D, Dumanchin C, Hannequin D, Dubois B, Belliard S, Puel M, Thomas-Anterion C, Michon A, Martin C, Charbonnier F (1999) Early-onset autosomal dominant Alzheimer disease: prevalence, genetic heterogeneity, and mutation spectrum. Am J Hum Genet 65:664–670
Cantsilieris S, Western PS, Baird PN, White SJ (2014) Technical considerations for genotyping multi-allelic copy number variation (CNV), in regions of segmental duplication. BMC Genomics 15:329
Conrad DF, Pinto D, Redon R, Feuk L, Gokcumen O, Zhang Y, Aerts J, Andrews TD, Barnes C, Campbell P, Fitzgerald T, Hu M, Ihm C, Kristiansson K, Macarthur D, Macdonald J, Onyiah I, Pang A, Robson S, Stirrups K, Valsesia A, Walter K, Wei J, Tyler-Smith C, Carter N, Lee C, Scherer S, Hurles M, WTCCC (2009) Origins and functional impact of copy number variation in the human genome. Nature 464:704–712
Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small G, Roses AD, Haines J, Pericak-Vance MA (1993) Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science 261:921–923
Corder E, Lannfelt L, Bogdanovic N, Fratiglioni L, Mori H (1998) The role of APOE polymorphisms in late-onset dementias. Cell Mol Life Sci 54:928–934
Corneveaux JJ, Myers AJ, Allen AN, Pruzin JJ, Ramirez M, Engel A, Nalls MA, Chen K, Lee W, Chewning K, Villa SE, Meechoovet HB, Gerber JD, Frost D, Benson HL, O’Reilly S, Chibnik LB, Shulman JM, Singleton AB, Craig DW, Van Keuren-Jensen KR, Dunckley T, Bennett DA, De Jager PL, Heward C, Hardy J, Reiman EM, Huentelman MJ (2010) Association of CR1, CLU and PICALM with Alzheimer’s disease in a cohort of clinically characterized and neuropathologically verified individuals. Hum Mol Genet 19:3295–3301. https://doi.org/10.1093/hmg/ddq221
Crehan H, Holton P, Wray S, Pocock J, Guerreiro R, Hardy J (2012) Complement receptor 1 (CR1) and Alzheimer’s disease. Immunobiology 217:244–250
Efthymiou AG, Goate AM (2017) Late onset Alzheimer’s disease genetics implicates microglial pathways in disease risk. Mol Neurodegener 12:43
Farrer LA, Cupples LA, Haines JL, Hyman B, Kukull WA, Mayeux R, Myers RH, Pericak-Vance MA, Risch N, van Duijn CM, APOE and Alzheimer Disease Meta Analysis Consortium (1997) Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis. JAMA 278:1349–1356
Fonseca MI, Chu S, Pierce AL, Brubaker WD, Hauhart RE, Mastroeni D, Clarke EV, Rogers J, Atkinson JP, Tenner AJ (2016) Analysis of the putative role of CR1 in Alzheimer’s disease: genetic association. Expression and function. PLoS One 11:e0149792. https://doi.org/10.1371/journal.pone.0149792
Gasque P, Chan P, Mauger C, Schouft MT, Singhrao S, Dierich MP, Morgan BP, Fontaine M (1996) Identification and characterization of complement C3 receptors on human astrocytes. J Immunol 156:2247–2255
Gaunt TR, Rodriguez S, Day IN (2007) Cubic exact solutions for the estimation of pairwise haplotype frequencies: implications for linkage disequilibrium analyses and a web tool ‘CubeX’. BMC Bioinform 8:428. https://doi.org/10.1186/1471-2105-8-428
Hazrati LN, Van Cauwenberghe C, Brooks PL, Brouwers N, Ghani M, Sato C, Cruts M, Sleegers K, St George-Hyslop P, Van Broeckhoven C, Rogaeva E (2012) Genetic association of CR1 with Alzheimer’s disease: a tentative disease mechanism. Neurobiol Aging 33:2949e5–2949e12. https://doi.org/10.1016/j.neurobiolaging.2012.07.001
Holers VM (2014) Complement and its receptors: new insights into human disease. Annu Rev Immunol 32:433–459. https://doi.org/10.1146/annurev-immunol-032713-120154
Hollingworth P, Harold D, Sims R, Gerrish A, Lambert JC, Carrasquillo MM, Abraham R, Hamshere ML, Pahwa JS, Moskvina V, Dowzell K, Jones N, Stretton A, Thomas C, Richards A, Ivanov D, Widdowson C, Chapman J, Lovestone S, Powell J, Proitsi P, Lupton MK, Brayne C, Rubinsztein DC, Gill M, Lawlor B, Lynch A, Brown KS, Passmore PA, Craig D, McGuinness B, Todd S, Holmes C, Mann D, Smith AD, Beaumont H, Warden D, Wilcock G, Love S, Kehoe PG, Hooper NM, Vardy ER, Hardy J, Mead S, Fox NC, Rossor M, Collinge J, Maier W, Jessen F, Ruther E, Schurmann B, Heun R, Kolsch H, van den Bussche H, Heuser I, Kornhuber J, Wiltfang J, Dichgans M, Frolich L, Hampel H, Gallacher J, Hull M, Rujescu D, Giegling I, Goate AM, Kauwe JS, Cruchaga C, Nowotny P, Morris JC, Mayo K, Sleegers K, Bettens K, Engelborghs S, De Deyn PP, Van Broeckhoven C, Livingston G, Bass NJ, Gurling H, McQuillin A, Gwilliam R, Deloukas P, Al-Chalabi A, Shaw CE, Tsolaki M, Singleton AB, Guerreiro R, Muhleisen TW, Nothen MM, Moebus S, Jockel KH, Klopp N, Wichmann HE, Pankratz VS, Sando SB, Aasly JO, Barcikowska M, Wszolek ZK, Dickson DW, Graff-Radford NR, Petersen RC et al (2011) Common variants at ABCA7, MS4A6A/MS4A4E, EPHA1, CD33 and CD2AP are associated with Alzheimer’s disease. Nat Genet 43:429–435. https://doi.org/10.1038/ng.803
Hollox EJ (2017) Analysis of copy number variation using the paralogue ratio test (PRT). Genotyping. Springer, New York, pp 127–146
Keenan BT, Shulman JM, Chibnik LB, Raj T, Tran D, Sabuncu MR, Allen AN, Corneveaux JJ, Hardy JA, Huentelman MJ, Lemere CA, Myers AJ, Nicholson-Weller A, Reiman EM, Evans DA, Bennett DA, De Jager PL (2012) A coding variant in CR1 interacts with APOE-epsilon4 to influence cognitive decline. Hum Mol Genet 21:2377–2388. https://doi.org/10.1093/hmg/dds054
Kisserli A, Tabary T, Cohen JHM, Duret V, Mahmoudi R (2017) High-resolution melting PCR for complement receptor 1 length polymorphism genotyping: an innovative tool for Alzheimer’s disease gene susceptibility assessment. J Vis Exp. https://doi.org/10.3791/56012
Lambert JC, Heath S, Even G, Campion D, Sleegers K, Hiltunen M, Combarros O, Zelenika D, Bullido MJ, Tavernier B, Letenneur L, Bettens K, Berr C, Pasquier F, Fievet N, Barberger-Gateau P, Engelborghs S, De Deyn P, Mateo I, Franck A, Helisalmi S, Porcellini E, Hanon O, de Pancorbo MM, Lendon C, Dufouil C, Jaillard C, Leveillard T, Alvarez V, Bosco P, Mancuso M, Panza F, Nacmias B, Bossu P, Piccardi P, Annoni G, Seripa D, Galimberti D, Hannequin D, Licastro F, Soininen H, Ritchie K, Blanche H, Dartigues JF, Tzourio C, Gut I, Van Broeckhoven C, Alperovitch A, Lathrop M, Amouyel P (2009) Genome-wide association study identifies variants at CLU and CR1 associated with Alzheimer’s disease. Nat Genet 41:1094–1099. https://doi.org/10.1038/ng.439
Lambert J-C, Ibrahim-Verbaas CA, Harold D, Naj AC, Sims R, Bellenguez C, Jun G, DeStefano AL, Bis JC, Beecham GW (2013) Meta-analysis of 74,046 individuals identifies 11 new susceptibility loci for Alzheimer’s disease. Nat Genet 45:1452
Lappalainen T, Sammeth M, Friedländer MR, Hoen PAC‘t, Monlong J, Rivas MA, Gonzàlez-Porta M, Kurbatova N, Griebel T, Ferreira PG, Barann M, Wieland T, Greger L, van Iterson M, Almlöf J, Ribeca P, Pulyakhina I, Esser D, Giger T, Tikhonov A, Sultan M, Bertier G, MacArthur DG, Lek M, Lizano E, Buermans HPJ, Padioleau I, Schwarzmayr T, Karlberg O, Ongen H, Kilpinen H, Beltran S, Gut M, Kahlem K, Amstislavskiy V, Stegle O, Pirinen M, Montgomery SB, Donnelly P, McCarthy MI, Flicek P, Strom TM, The Geuvadis C, Lehrach H, Schreiber S, Sudbrak R, Carracedo Á, Antonarakis SE, Häsler R, Syvänen A-C, van Ommen G-J, Brazma A, Meitinger T, Rosenstiel P, Guigó R, Gut IG, Estivill X, Dermitzakis ET (2013) Transcriptome and genome sequencing uncovers functional variation in humans. Nature 501:506–511. https://doi.org/10.1038/nature12531
Latorra D, Campbell K, Wolter A, Hurley JM (2003) Enhanced allele-specific PCR discrimination in SNP genotyping using 3′ locked nucleic acid (LNA) primers. Hum Mutat 22:79–85
Li W, Cowley A, Uludag M, Gur T, McWilliam H, Squizzato S, Park YM, Buso N, Lopez R (2015) The EMBL-EBI bioinformatics web and programmatic tools framework. Nucleic Acids Res 43:W580–W584
Luo J, Li S, Qin X, Song L, Peng Q, Chen S, Xie Y, Xie L, Li T, He Y, Deng Y, Wang J, Zeng Z (2014) Meta-analysis of the association between CR1 polymorphisms and risk of late-onset Alzheimer’s disease. Neurosci Lett 578:165–170. https://doi.org/10.1016/j.neulet.2014.06.055
Mahmoudi R, Kisserli A, Novella JL, Donvito B, Drame M, Reveil B, Duret V, Jolly D, Pham BN, Cohen JH (2015) Alzheimer’s disease is associated with low density of the long CR1 isoform. Neurobiol Aging 36:1766e5–1766e12. https://doi.org/10.1016/j.neurobiolaging.2015.01.006
Morgan BP (2018) Complement in the pathogenesis of Alzheimer’s disease. Semin Immunopathol 40:113–124. https://doi.org/10.1007/s00281-017-0662-9
Moulds J, Reveille J, Arnett F (1996) Structural polymorphisms of complement receptor 1 (CR1) in systemic lupus erythematosus (SLE) patients and normal controls of three ethnic groups. Clin Exp Immunol 105:302–305
Naj AC, Schellenberg GD (2017) Genomic variants, genes, and pathways of Alzheimer’s disease: an overview. Am J Med Genet B 174:5–26
Naj AC, Jun G, Beecham GW, Wang LS, Vardarajan BN, Buros J, Gallins PJ, Buxbaum JD, Jarvik GP, Crane PK, Larson EB, Bird TD, Boeve BF, Graff-Radford NR, De Jager PL, Evans D, Schneider JA, Carrasquillo MM, Ertekin-Taner N, Younkin SG, Cruchaga C, Kauwe JS, Nowotny P, Kramer P, Hardy J, Huentelman MJ, Myers AJ, Barmada MM, Demirci FY, Baldwin CT, Green RC, Rogaeva E, St George-Hyslop P, Arnold SE, Barber R, Beach T, Bigio EH, Bowen JD, Boxer A, Burke JR, Cairns NJ, Carlson CS, Carney RM, Carroll SL, Chui HC, Clark DG, Corneveaux J, Cotman CW, Cummings JL, DeCarli C, DeKosky ST, Diaz-Arrastia R, Dick M, Dickson DW, Ellis WG, Faber KM, Fallon KB, Farlow MR, Ferris S, Frosch MP, Galasko DR, Ganguli M, Gearing M, Geschwind DH, Ghetti B, Gilbert JR, Gilman S, Giordani B, Glass JD, Growdon JH, Hamilton RL, Harrell LE, Head E, Honig LS, Hulette CM, Hyman BT, Jicha GA, Jin LW, Johnson N, Karlawish J, Karydas A, Kaye JA, Kim R, Koo EH, Kowall NW, Lah JJ, Levey AI, Lieberman AP, Lopez OL, Mack WJ, Marson DC, Martiniuk F, Mash DC, Masliah E, McCormick WC, McCurry SM, McDavid AN, McKee AC, Mesulam M, Miller BL et al (2011) Common variants at MS4A4/MS4A6E, CD2AP, CD33 and EPHA1 are associated with late-onset Alzheimer’s disease. Nat Genet 43:436–441. https://doi.org/10.1038/ng.801
Rogers J, Cooper NR, Webster S, Schultz J, McGeer PL, Styren SD, Civin WH, Brachova L, Bradt B, Ward P et al (1992) Complement activation by beta-amyloid in Alzheimer disease. Proc Natl Acad Sci USA 89:10016–10020
Sievers F, Wilm A, Dineen D, Gibson TJ, Karplus K, Li W, Lopez R, McWilliam H, Remmert M, Söding J (2011) Fast, scalable generation of high-quality protein multiple sequence alignments using Clustal Omega. Mol Syst Biol 7(1):539
Van Cauwenberghe C, Bettens K, Engelborghs S, Vandenbulcke M, Van Dongen J, Vermeulen S, Vandenberghe R, De Deyn PP, Van Broeckhoven C, Sleegers K (2013) Complement receptor 1 coding variant p.Ser1610Thr in Alzheimer’s disease and related endophenotypes. Neurobiol Aging 34(2235):e1–e6. https://doi.org/10.1016/j.neurobiolaging.2013.03.008
Vik DP, Wong WW (1993) Structure of the gene for the F allele of complement receptor type 1 and sequence of the coding region unique to the S allele. J Immunol 151:6214–6224
Villegas-Llerena C, Phillips A, Garcia-Reitboeck P, Hardy J, Pocock JM (2016) Microglial genes regulating neuroinflammation in the progression of Alzheimer’s disease. Curr Opin Neurobiol 36:74–81
Wong WW, Wilson JG, Fearon DT (1983) Genetic regulation of a structural polymorphism of human C3b receptor. J Clin Investig 72:685–693. https://doi.org/10.1172/JCI111018
Wong WW, Cahill JM, Rosen MD, Kennedy CA, Bonaccio ET, Morris MJ, Wilson JG, Klickstein LB, Fearon DT (1989) Structure of the human CR1 gene. Molecular basis of the structural and quantitative polymorphisms and identification of a new CR1-like allele. J Exp Med 169:847–863. https://doi.org/10.1084/jem.169.3.847
Zuccherato LW, Schneider S, Tarazona-Santos E, Hardwick RJ, Berg DE, Bogle H, Gouveia MH, Machado LR, Machado M, Rodrigues-Soares F, Soares-Souza GB, Togni DL, Zamudio R, Gilman RH, Duarte D, Hollox EJ, Rodrigues MR (2017) Population genetics of immune-related multilocus copy number variation in Native Americans. J R Soc Interface. https://doi.org/10.1098/rsif.2017.0057
Acknowledgements
We would like to thank Daniel Zadik for help and advice, and Rachael Madison for technical support. All authors have read and approved the final manuscript. The ARUK Consortium was funded by Alzheimer’s Research UK, with the following members: Tulsi Patel: Schools of Life Sciences and Medicine, University of Nottingham, Nottingham, NG7 2UH, UK; Tamar Guetta-Baranes: Schools of Life Sciences and Medicine, University of Nottingham, Nottingham, NG7 2UH, UK; Keeley J. Brookes: Schools of Life Sciences and Medicine, University of Nottingham, Nottingham, NG7 2UH, UK; David M. Mann: Institute of Brain, Behaviour and Mental Health, Faculty of Medical and Human Sciences, University of Manchester, Manchester, M13 9PT, UK; Peter Passmore: Centre for Public Health, School of Medicine, Queen’s University Belfast, BT9 7BL, UK; David Craig: Centre for Public Health, School of Medicine, Queen’s University Belfast, BT9 7BL, UK; Janet Johnston: Centre for Public Health, School of Medicine, Queen’s University Belfast, BT9 7BL, UK; Bernadette McGuinness: Centre for Public Health, School of Medicine, Queen’s University Belfast, BT9 7BL, UK; Stephen Todd: Centre for Public Health, School of Medicine, Queen’s University Belfast, BT9 7BL, UK; Reinhard Heun: Centre for Public Health, School of Medicine, Queen’s University Belfast, BT9 7BL, UK; Heike Kölsch: Department of Psychiatry, University of Bonn, Bonn 53105, Germany; Patrick G. Kehoe: School of Clinical Sciences, John James Laboratories, University of Bristol, Bristol, BS16 1LE, UK; Emma R. L. C. VardySalford Royal NHS Foundation Trust; Nigel M. Hooper: Institute of Brain, Behaviour and Mental Health, Faculty of Medical and Human Sciences, University of Manchester, Manchester, M13 9PT, UK; Stuart Pickering-Brown: Institute of Brain, Behaviour and Mental Health, Faculty of Medical and Human Sciences, University of Manchester, Manchester, M13 9PT, UK; Julie Snowden: Cerebral Function Unit, Greater Manchester Neurosciences Centre, Salford Royal Hospital, Stott Lane, Salford, M6 8HD, UK; Anna Richardson: Cerebral Function Unit, Greater Manchester Neurosciences Centre, Salford Royal Hospital, Stott Lane, Salford, M6 8HD, UK; Matt Jones: Cerebral Function Unit, Greater Manchester Neurosciences Centre, Salford Royal Hospital, Stott Lane, Salford, M6 8HD, UK; David Neary: Cerebral Function Unit, Greater Manchester Neurosciences Centre, Salford Royal Hospital, Stott Lane, Salford, M6 8HD, UK; Jenny Harris: Cerebral Function Unit, Greater Manchester Neurosciences Centre, Salford Royal Hospital, Stott Lane, Salford, M6 8HD, UK; A. David Smith: University of Oxford (OPTIMA), Oxford, OX3 9DU, UK; Gordon Wilcock: University of Oxford (OPTIMA), Oxford, OX3 9DU, UK; Donald Warden: University of Oxford (OPTIMA), Oxford, OX3 9DU, UK; Clive Holmes: Clinical and Experimental Science, University of Southampton, Southampton, SO17 1BJ, UK; Kevin Morgan: Schools of Life Sciences and Medicine, University of Nottingham, Nottingham, NG7 2UH, UK.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
For full list of ARUK consortium members, see acknowledgements.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kucukkilic, E., Brookes, K., Barber, I. et al. Complement receptor 1 gene (CR1) intragenic duplication and risk of Alzheimer’s disease. Hum Genet 137, 305–314 (2018). https://doi.org/10.1007/s00439-018-1883-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-018-1883-2