Abstract
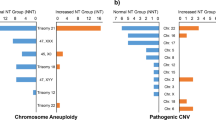
Increased fetal nuchal translucency (NT) is a common ultrasonic manifestation during pregnancy. Many studies have confirmed that NT ≥ 3 mm is a high risk factor for adverse pregnancy outcome. However, when NT is between 2.5 and 2.9 mm, will it increase the risk of fetal chromosome abnormalities and other diseases? What is the most appropriate method for prenatal chromosome evaluation? At present, it has not been widely reported in the literature, and the conclusion is also controversial. This prospective cohort study included fetal samples from women who underwent amniocentesis from 2017 to 2020. The samples of the experimental group were fetuses with NT ≥ 2.5 mm at 11 to 13 + 6 weeks of gestation, with or without ultrasonographic anomaly. The control group contained fetal NT < 2.5 mm without ultrasonographic anomalies. All amniotic fluid samples were tested by copy number variants sequencing. In 262 fetal samples with isolated NT from 2.5 to 2.9 mm, the detection rate of aneuploidy was 3.4% (9/262), and the risk of aneuploidy was significantly higher than that of the control group (1.4%, 32/2331) (relative risk 2.5, 95% CI 1.2–5.2). The detection rates of other pathogenic/likely pathogenic copy number variants in the two groups were 0.8% (2/262) and 1.3% (31/2331), respectively, which was not statistically significant (relative risk 0.6, 95% CI 0.1–2.4). Our results showed that isolated NT from 2.5 to 2.9 mm increased the risk of fetal chromosome aneuploidy. Therefore, noninvasive prenatal screening is recommended as the first choice for prenatal chromosome evaluation in this population.
Similar content being viewed by others
References
Alanen J, Leskinen M, Sairanen M, Korpimaki T, Kouru H, Gissler M et al (2019) Fetal nuchal translucency in severe congenital heart defects: experiences in Northern Finland. J Matern Fetal Neonatal Med 32(9):1454–1460
Al-Hamed MH, Kurdi W, Khan R, Tulbah M, AlNemer M, AlSahan N et al (2022) Prenatal exome sequencing and chromosomal microarray analysis in fetal structural anomalies in a highly consanguineous population reveals a propensity of ciliopathy genes causing multisystem phenotypes. Hum Genet 141(1):101–126
American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics; Committee on Genetics; Society for Maternal-Fetal Medicine (2020) Screening for Fetal Chromosomal Abnormalities: ACOG Practice Bulletin, Number 226. Obstet Gynecol 136(4):e48–e69
Brady PD, Delle Chiaie B, Christenhusz G, Dierickx K, Van Den Bogaert K, Menten B et al (2014) A prospective study of the clinical utility of prenatal chromosomal microarray analysis in fetuses with ultrasound abnormalities and an exploration of a framework for reporting unclassified variants and risk factors. Genet Med 16(6):469–476
Croonen EA, Nillesen WM, Stuurman KE, Oudesluijs G, van de Laar IM, Martens L et al (2013) Prenatal diagnostic testing of the Noonan syndrome genes in fetuses with abnormal ultrasound findings. Eur J Hum Genet 21(9):936–942
Giorlandino C, Cignini P, Padula F, Giannarelli D, d’Emidio L, Aloisi A et al (2015) Effects of exogenous progesterone on fetal nuchal translucency: an observational prospective study. Am J Obstet Gynecol 212(3):335.e1–7
Grande M, Jansen FA, Blumenfeld YJ, Fisher A, Odibo AO, Haak MC et al (2015) Genomic microarray in fetuses with increased nuchal translucency and normal karyotype: a systematic review and meta-analysis. Ultrasound Obstet Gynecol 46(6):650–658
Hellmuth SG, Pedersen LH, Miltoft CB, Petersen OB, Kjaergaard S, Ekelund C et al (2017) Increased nuchal translucency thickness and risk of neurodevelopmental disorders. Ultrasound Obstet Gynecol 49(5):592–598
Hu T, Tian T, Zhang Z, Wang J, Hu R, Xiao L et al (2021) Prenatal chromosomal microarray analysis in 2466 fetuses with ultrasonographic soft markers: a prospective cohort study. Am J Obstet Gynecol 224(5):516.e1–16
Hui L, Pynaker C, Bonacquisto L, Lindquist A, Poulton A, Kluckow E et al (2021) Reexamining the optimal nuchal translucency cutoff for diagnostic testing in the cell-free DNA and microarray era: results from the Victorian Perinatal Record Linkage study. Am J Obstet Gynecol 225(5):527.e1–12
Iwarsson E, Jacobsson B, Dagerhamn J, Davidson T, Bernabé E, Heibert AM (2017) Analysis of cell-free fetal DNA in maternal blood for detection of trisomy 21, 18 and 13 in a general pregnant population and in a high risk population—a systematic review and meta-analysis. Acta Obstet Gynecol Scand 96(1):7–18
Khalil A, Pajkrt E, Chitty LS (2011) Early prenatal diagnosis of skeletal anomalies. Prenat Diagn 31(1):115–124
Kim MH, Park SH, Cho HJ, Choi JS, Kim JO, Ahn HK et al (2006) Threshold of nuchal translucency for the detection of chromosomal aberration: comparison of different cut-offs. J Korean Med Sci 21(1):11–14
Lan L, Wu H, She L, Zhang B, He Y, Luo D et al (2020) Analysis of copy number variation by sequencing in fetuses with nuchal translucency thickening. J Clin Lab Anal 34(8):e23347
Mellis R, Eberhardt RY, Hamilton SJ, PAGE Consortium, McMullan DJ, Kilby MD, Maher ER et al (2022a) Fetal exome sequencing for isolated increased nuchal translucency: should we be doing it? BJOG 129(1):52–61
Mellis R, Oprych K, Scotchman E, Hill M, Chitty LS (2022b) Diagnostic yield of exome sequencing for prenatal diagnosis of fetal structural anomalies: a systematic review and meta-analysis. Prenat Diagn 42(6):662–685
Mogra R, Alabbad N, Hyett J (2012) Increased nuchal translucency and congenital heart disease. Early Hum Dev 88(5):261–267
Mohtisham FS, Sallam A, Shawli A (2019) Lethal multiple pterygium syndrome. BMJ Case Rep 12(5):e229045
Narava S, Balbir Singh S, Barpanda S, Bricker L (2022) Outcome of pregnancies with first-trimester increased nuchal translucency and cystic hygroma in a tertiary maternity hospital in United Arab Emirates. Int J Gynaecol Obstet https://doi.org/10.1002/ijgo.14222. Epub ahead of print
Nicolaides KH, Azar G, Byrne D, Mansur C, Marks K (1992) Fetal nuchal translucency: ultrasound screening for chromosomal defects in first trimester of pregnancy. BMJ 304(6831):867–869
Ozyuncu O, Tanacan A, Fadiloglu E, Unal C, Ziyadova G, Deren O (2021) Impact of increased nuchal translucency values on pregnancy outcomes: a tertiary center experience. Fetal Pediatr Pathol 40(3):189–197
Pauta M, Martinez-Portilla RJ, Borrell A (2022) Diagnostic yield of next-generation sequencing in fetuses with isolated increased nuchal translucency: systematic review and meta-analysis. Ultrasound Obstet Gynecol 59(1):26–32
Peng Y, Liang C, Xi H, Yang S, Hu J, Pang J et al (2021) Case report: novel NIPBL variants cause Cornelia de Lange syndrome in Chinese patients. Front Genet 12:699894
Petersen OB, Smith E, Van Opstal D, Polak M, Knapen MFCM, Diderich KEM et al (2020) Nuchal translucency of 3.0–3.4 mm an indication for NIPT or microarray? Cohort analysis and literature review. Acta Obstet Gynecol Scand 99(6):765–774
Riggs ER, Andersen EF, Cherry AM, Kantarci S, Kearney H, Patel A et al (2020) Technical standards for the interpretation and reporting of constitutional copy-number variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics (ACMG) and the Clinical Genome Resource (ClinGen). Genet Med 22(2):245–257
Sagi-Dain L, Singer A, Ben Shachar S, Josefsberg Ben Yehoshua S, Feingold-Zadok M et al (2021) Risk of clinically significant chromosomal microarray analysis findings in fetuses with nuchal translucency from 3.0 mm through 3.4 mm. Obstet Gynecol 137(1):126–131
Sparks TN, Lianoglou BR, Adami RR, Pluym ID, Holliman K, Duffy J et al (2020) Exome sequencing for prenatal diagnosis in nonimmune hydrops fetalis. N Engl J Med. 383(18):1746–1756
Tekesin I (2020) Pregnancy outcome in foetuses with increased nuchal translucency—10-years’ experience in a prenatal medical practice. J Obstet Gynaecol 40(4):455–460
Tonni G, Ventura A, De Felice C (2005) First trimester increased nuchal translucency associated with fetal achondroplasia. Am J Perinatol 22(3):145–148
Wang J, Chen L, Zhou C, Wang L, Xie H, Xiao Y et al (2018) Prospective chromosome analysis of 3429 amniocentesis samples in China using copy number variation sequencing. Am J Obstet Gynecol 219(3):287.e1-287.e18
Wapner RJ, Martin CL, Levy B, Ballif BC, Eng CM, Zachary JM et al (2012) Chromosomal microarray versus karyotyping for prenatal diagnosis. N Engl J Med 367(23):2175–2184
Zhang Z, Hu T, Wang J, Li Q, Wang H, Liu S (2019) Prenatal diagnostic value of chromosomal microarray in fetuses with nuchal translucency greater than 2.5 mm. Biomed Res Int 2019:6504159
Funding
This research was supported by the National Key Research and Development Program of China (No. 2021YFC1005300) and the Program of Science and Technology Department of Sichuan Province (No. 2022YFS0244).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This study was approved by the Medical Ethics Committee of the West China Second University Hospital, Sichuan University (medical research 2016–7). All experiments were performed in accordance with relevant guidelines and regulations. All pregnant women who underwent amniocentesis received comprehensive genetic counselling and provided written informed consent.
Additional information
Communicated by Shuhua Xu.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yin, D., Chen, L., Wang, L. et al. Does isolated nuchal translucency from 2.5 to 2.9 mm increase the risk of fetal chromosome disease?. Mol Genet Genomics 297, 1643–1648 (2022). https://doi.org/10.1007/s00438-022-01948-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00438-022-01948-5