Abstract
Background
The distance between tumor and bronchial resection margin (DBTM) had no clear standard in lung cancer surgery. We aimed to select the optimal cut-off value to provide a standard for surgery of the patients with primary endobronchial neoplasm.
Methods
We retrospectively analyzed patients with primary endobronchial neoplasm who underwent surgical resection between 2005 and 2012. The receiver operating characteristic curves and the Youden index were used to calculate the optimal cut-off value of the DBTM. Propensity score matching was applied to reduce selection bias. Survival was assessed with Kaplan–Meier analysis, log-rank test and Cox proportional hazards model.
Results
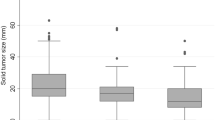
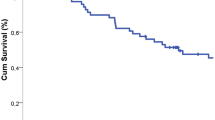
A total of 1048 patients comprised in the study cohort and 1.7 cm was determined the optimal cut-off value, including 531 grouped in DBTM ≤ 1.7 cm and 517 grouped in DBTM > 1.7 cm. Before propensity score matching, the 5-year recurrence-free survival was 38.7% in DBTM ≤ 1.7 cm group and 67.1% in DBTM > 1.7 cm (hazard ratio 0.48, P < 0.001), while the 5-year overall survival was 30.1% and 50.7%, respectively (hazard ratio 0.64, P < 0.001). After propensity score matching, the 5-year recurrence-free survival was 38.8% in DBTM ≤ 1.7 cm group and 66.1% in DBTM > 1.7 cm (hazard ratio 0.51, P < 0.001), while the 5-year overall survival was 34.7% and 50%, respectively (hazard ratio 0.81, P = 0.012). Multivariable cox model showed that the DBTM was an independent predictor for recurrence-free survival (hazard ratio 0.51, P = 0.001) and overall survival (hazard ratio 0.84, P = 0.026).
Conclusions
The DBTM was an independent predictor for outcomes in primary endobronchial neoplasm, and patients with the DBTM ≤ 1.7 cm should actively receive adjuvant therapy after surgery.
Graphical abstract

The distance between tumor and bronchial resection margin (DBTM), the distance between the most proximal border of the macroscopic tumor and bronchial resection margin was measured by pathologist in the fresh specimens before formalin fixation. The DBTM less than 1.7cm had higher recurrence-free survival and overall survival and was an independent prognostic factor for patients with primary endobronchial neoplasm



Similar content being viewed by others
Availability of data and materials
The data of this article will be shared on reasonable request to the corresponding author.
Abbreviations
- IASLC:
-
International Association for the Study of Lung Cancer
- NSCLC:
-
Non-small cell lung cancer
- DBTM:
-
The distance between tumor and bronchial resection margin
- PSM:
-
Propensity score matching
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the ROC curve
- IQR:
-
Interquartile range
- SMD:
-
Standardized mean difference
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- RFS:
-
Recurrence-free survival
- OS:
-
Overall survival
References
Arriagada R, Auperin A, Burdett S, Higgins JP, Johnson DH, Le Chevalier T et al (2010) Adjuvant chemotherapy, with or without postoperative radiotherapy, in operable non-small-cell lung cancer: two meta-analyses of individual patient data. Lancet 375:1267–1277
Austin PC, Mamdani MM (2006) A comparison of propensity score methods: a case-study estimating the effectiveness of post-AMI statin use. Stat Med 25:2084–2106
Dai C, Shen J, Ren Y, Zhong S, Zheng H, He J et al (2016) Choice of surgical procedure for patients with non-small-cell lung cancer ≤ 1 cm or > 1 to 2 cm among lobectomy, segmentectomy, and wedge resection: a population-based study. J Clin Oncol 34:3175–3182
Detterbeck FC, Chansky K, Groome P, Bolejack V, Crowley J, Shemanski L et al (2016) The IASLC lung cancer staging project: methodology and validation used in the development of proposals for revision of the stage classification of NSCLC in the forthcoming (Eighth) edition of the TNM classification of lung cancer. J Thorac Oncol 11:1433–1446
Eguchi T, Kameda K, Lu S, Bott MJ, Tan KS, Montecalvo J et al (2019) Lobectomy is associated with better outcomes than sublobar resection in spread through air spaces (stas)-positive T1 lung adenocarcinoma: a propensity score-matched analysis. J Thorac Oncol 14:87–98
Gagliasso M, Migliaretti G, Ardissone F (2017) Assessing the prognostic impact of the international association for the study of lung cancer proposed definitions of complete, uncertain, and incomplete resection in non-small cell lung cancer surgery. Lung Cancer 111:124–130
Gunluoglu MZ, Kocaturk CI, Demir A, Urer HN, Dincer SI, Bedirhan MA (2018) Bronchial stump recurrence after complete resection of lung cancer: effect of the distance between the tumor and bronchial resection margin. Thorac Cardiovasc Surg 66:156–163
Hong TH, Kim J, Shin S, Kim HK, Choi YS, Zo JI et al (2020) Clinical outcomes of microscopic residual disease after bronchial sleeve resection for non-small cell lung cancer. J Thorac Cardiovasc Surg 29:30518–30523
Kadota K, Kushida Y, Kagawa S, Ishikawa R, Ibuki E, Inoue K et al (2019) Limited resection is associated with a higher risk of locoregional recurrence than lobectomy in stage I lung adenocarcinoma with tumor spread through air spaces. Am J Surg Pathol 43:1033–1041
Kara M, Sak SD, Orhan D, Yavuzer S (2000) Changing patterns of lung cancer; (3/4 in) 1.9 cm; still a safe length for bronchial resection margin? Lung Cancer 30:161–168
Kates M, Swanson S, Wisnivesky JP (2011) Survival following lobectomy and limited resection for the treatment of stage I non-small cell lung cancer<=1 cm in size: a review of SEER data. Chest 139:491–496
Kim D, Kim HK, Choi YS, Kim K, Kim J, Shim YM (2015) Central lung cancer management: impact of bronchial resection margin length. Thorac Cardiovasc Surg 63:583–588
Li C, Chen J, Qin G (2019) Partial youden index and its inferences. J Biopharm Stat 29:385–399
Lv T, Zou J, Liu H, Shen Q, Lu Z, Zhou X et al (2017) Detection of oncogenic mutations in resected bronchial margins by next-generation sequencing indicates early relapse in stage IA lung adenocarcinoma patients. Oncotarget 8:40643–40653
National Comprehensive Cancer Network. NCCN Guide-lines for surveillance following therapy for NSCLC. https://www.nccn.org/professionals/physician_gls/f_ guidelines.asp. Accessed July 30, 2016.
Pisters KM, Evans WK, Azzoli CG, Kris MG, Smith CA, Desch CE et al (2007) Cancer care ontario and American society of clinical oncology adjuvant chemotherapy and adjuvant radiation therapy for stages I-IIIA resectable non small-cell lung cancer guideline. J Clin Oncol 25:5506–5518
Rami-Porta R, Mateu-Navarro M, Freixinet J, de la Torre M, Torres-García AJ, Pun YW et al (2005) Type of resection and prognosis in lung cancer. Experience of a multicentre study. Eur J Cardiothorac Surg 28:622–628
Sato H, Toyooka S, Soh J, Hotta K, Katsui K, Shien K et al (2017) Advantage of induction chemoradiotherapy for lung cancer in securing cancer-free bronchial margin. Ann Thorac Surg 104:971–978
Shi W, Zhang W, Sun H, Shao Y (2012) Sleeve lobectomy versus pneumonectomy for non-small cell lung cancer: a meta-analysis. World J Surg Oncol 10:265
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA Cancer J Clin 72:7–33
Tomaszek SC, Kim Y, Cassivi SD, Jensen MR, Shen KH, Nichols FC et al (2011) Bronchial resection margin length and clinical outcome in non-small cell lung cancer. Eur J Cardiothorac Surg 40:1151–1156
Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB et al (2015) The 2015 world health organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 10:1243–1260
Acknowledgements
Not applicable.
Funding
This study was supported by the National Natural Science Foundations of China (NO. 82273119).
Author information
Authors and Affiliations
Contributions
ZX: conceptualization; Formal analysis; Methodology; Writing- original draft; Writing-review & editing. MZ: Investigation; Validation; Writing original-draft; Writing-review & editing. ZL, Investigation; Formal analysis; Writing-review & editing. XW, Investigation; Resources. ZL, Formal analysis; Data curation; Writing-review & editing. ZZ, Conceptualization; Project administration; Resources; Writing- original draft; Writing-review & editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. Our study was approved by the Ethic Committee of Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center for Cancer. Approve number: bc2021134. Consent of patients for this retrospective study was waived.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiao, Z., Zhang, M., Liu, Z. et al. Distance between tumor and bronchial resection margin is an independent predictor of recurrence-free survival and overall survival in primary endobronchial neoplasm. J Cancer Res Clin Oncol 149, 11171–11180 (2023). https://doi.org/10.1007/s00432-023-04917-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-04917-6