Abstract
Background
Mammographic density (MD) is a risk factor for breast cancer (BC) development, and recurrence. However, its predictive value has been less studied. Herein, we challenged MD as a biomarker associated with response in patients treated with neoadjuvant therapy (NAT).
Methods
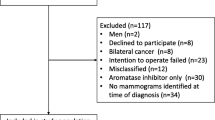
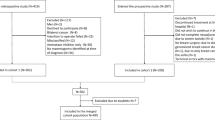
Data on all NAT treated BC patients prospectively collected in the registry of Fondazione IRCCS Istituto Nazionale dei Tumori, Milano, Italy (2009–2019) were identified. Diagnostic mammograms were used to evaluate and score MD as categorized by the Breast Imaging-Reporting and Data System (BI-RADS), which identifies 4 levels of MD in keeping with relative increase of fibro-glandular over fat tissue. Each case was classified according to the following categories a (MD < 25%), b (26–50%), c (51–75%), and d (> 75%). The association between MD and pathological complete response (pCR), i.e., absence of BC cells in surgical specimens, was analyzed in multivariable setting used logistic regression models with adjustment for clinical and pathological variables.
Results
A total of 442 patients were analyzed, 120 of which (27.1%) attained a pCR. BI-RADS categories a, b, c, and d accounted for 10.0%, 37.8%, 37.1% and 15.2% of cases. Corresponding pCR were 20.5%, 26.9%, 30.5%, 23.9%, respectively. At multivariable analysis, when compared to cases classified as BI-RADS a, those with denser breast showed an increased likelihood of pCR with odds ratio (OR) of 1.70, 2.79, and 1.47 for b, c and d categories, respectively (p = 0.0996), independently of age, BMI [OR underweight versus (vs) normal = 3.76], clinical nodal and tumor status (OR T1/Tx vs T4 = 3.87), molecular subtype (HER2-positive vs luminal = 10.74; triple-negative vs luminal = 8.19). In subgroup analyses, the association of MD with pCR was remarkable in triple-negative (ORs of b, c and d versus a: 1.85, 2.49 and 1.55, respectively) and HER2-positive BC cases (ORs 2.70, 3.23, and 1.16).
Conclusion
Patients with dense breast are more likely to attain a pCR at net of other predictive factors. The potential of MD to assist decisions on BC management and as a stratification factor in neoadjuvant clinical trials should be considered.
Similar content being viewed by others
References
Baili P, Torresani M, Agresti R, Rosito G, Daidone MG, Veneroni S, Cavallo I, Funaro F, Giunco M, Turco A, Amash H, Scavo A, Minicozzi P, Bella F, Meneghini E, Sant M. A breast cancer clinical registry in an Italian comprehensive cancer center: an instrument for descriptive, clinical, and experimental research. Tumori. 2015 Jul-Aug;101(4):440–6. doi: https://doi.org/10.5301/tj.5000341.
Cain H, Macpherson IR, Beresford M, Pinder SE, Pong J, Dixon JM (2017) Neoadjuvant therapy in early breast cancer: treatment considerations and common debates in practice. Clin Oncol (r Coll Radiol) 29(10):642–652
Castaneda CA, Flores R, Rojas K, Flores C, Castillo M, Milla E (2014) Association between mammographic features and response to neoadjuvant chemotherapy in locally advanced breast carcinoma. Hematol Oncol Stem Cell Ther 7(4):149–156
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, Bonnefoi H, Cameron D, Gianni L, Valagussa P (2014) Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 384(9938):164–172
Curigliano G, Burstein HJ, Winer EP, Gnant M, Dubsky P, Loibl S, et al. De-escalating and escalating treatments for early-stage breast cancer: the St. Gallen International Expert Consensus Conference on the Primary Therapy of Early Breast Cancer 2017 . Ann Oncol. 2017 Aug 1;28(8):1700–1712. doi: https://doi.org/10.1093/annonc/mdx308.
Elfgen C, Varga Z, Reeve K, Moskovszky L, Bjelic-Radisic V, Tausch C, Güth U (2019) The impact of distinct triple-negative breast cancer subtypes on misdiagnosis and diagnostic delay. Breast Cancer Res Treat 177(1):67–75
Elsamany S, Alzahrani A, Abozeed WN, Rasmy A, Farooq MU, Elbiomy MA, Rawah E, Alsaleh K, Abdel-Aziz NM (2015) Mammographic breast density: predictive value for pathological response to neoadjuvant chemotherapy in breast cancer patients. Breast 24(5):576–581
Freeman GH, Halton JH (1951) Note on exact treatment of contingency, goodness of fit and other problems of significance. Biometrika 38:141–149
Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S et al (2010) American Society of Clinical Oncology/College of American pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol 28:2784–2795
Huo CW, Chew G, Hill P, Huang D, Ingman W, Hodson L et al (2015) High mammographic density is associated with an increase in stromal collagen and immune cells within the mammary epithelium. Breast Cancer Res 17(1):79
Loibl S, Denkert C, von Minckwitz G (2015) Neoadjuvant treatment of breast cancer–Clinical and research perspective. Breast 24(Suppl 2):S73–S77
Maisonneuve P, Disalvatore D, Rotmensz N, Curigliano G, Colleoni M, Dellapasqua S et al (2014) Proposed new clinicopathological surrogate definitions of luminal A and luminal B (HER2-negative) intrinsic breast cancer subtypes. Breast Cancer Res 16(3):R65
Martin LJ, Boyd NF (2008) Potential mechanisms of breast cancer risk associated with mammographic density: hypotheses based on epidemiological evidence. Breast Cance Res 10(1):201
Maskarinec G, Takata Y, Chen Z, Gram IT, Nagata C, Pagano I, Hayashi K, Arendell L, Skeie G, Rinaldi S, Kaaks R (2007) IGF-I and mammographic density in four geographic locations: a pooled analysis. Int J Cancer 121(8):1786–1792
Maskarinec G, Ju D, Fong J, Horio D, Chan O, Loo LWM, Hernandez BY (2018) Mammographic density and breast tissue expression of inflammatory markers, growth factors, and vimentin. BMC Cancer 18:1191
McCormack VA, dos Santos SI (2006) Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomark Prev 15(6):1159–1169
Miglietta F, Dieci MV, Griguolo G, Guarneri V. Neoadjuvant approach as a platform for treatment personalization: focus on HER2-positive and triple-negative breast cancer. Cancer Treat Rev. 2021 Jul;98:102222.
Pike MC, Krailo MD, Henderson BE, Casagrande JT, Hoel DG (1983) Hormonal risk factors, breast tissue age and the age-incidence of breast cancer. Nature 303:767–770
Pinsky RW, Helvie MA (2010) Mammographic breast density: effect on imaging and breast cancer risk. J Natl Compr Canc Netw 8(10):1157–1164
Shawky MS, Huo CW, Henderson MA, Redfern A, Britt K, Thompson EW (2019) A review of the influence of mammographic density on breast cancer clinical and pathological phenotype. Breast Cancer Res Treat 177(2):251–276
Skarping I, Fornvik D, Sartor H, Heide-Jorgensen U, Zackrisson S, Borgquist S (2019) Mammographic density is a potential predictive marker of pathological response after neoadjuvant chemotherapy in breast cancer. BMC Canc 19(1):1272
Skarping I, Förnvik D, Heide-Jørgensen U, Sartor H, Hall P, Zackrisson S, Borgquist S (2021) Mammographic density as an image-based biomarker of therapy response in neoadjuvant-treated breast cancer patients. Cancer Causes Control 32(3):251–260
Sobin LH, Gospodarowicz MK, Wittekind CH (2010) TNM classification of malignant tumours, 7th edn. Wiley, Chichester
von Minckwitz G., Untch M., Ju Blohmer, Costa S.D., Eidtmann H., Fasching P.A., Gerber B., Eiermann W., Hilfrich J., Huober J. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30(15):1796–1804.
World Health Organization—Nutrition—Body mass index classification. 2020. Available from: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we do not have any conflict of interest.
Ethical approval
The present study has been reviewed and approved.
Research involving in human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Di Cosimo, S., Depretto, C., Miceli, R. et al. Mammographic density to predict response to neoadjuvant systemic breast cancer therapy. J Cancer Res Clin Oncol 148, 775–781 (2022). https://doi.org/10.1007/s00432-021-03881-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-021-03881-3