Abstract
Purpose
To investigate the best lymph node (LN) metastasis predictor for overall survival (OS) in head neck cancer (HNC): pN classification, number of positive lymph nodes (PNOD), lymph node ratio (LNR), or log odds of positive lymph nodes (LODDS).
Methods
In total, 225 surgically treated HNC patients were evaluated for the different LN classifications and OS.
Results
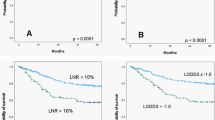
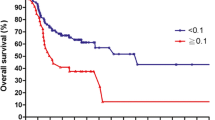
Five-year OS was 71.8 %. Mean number of yielded LN and PNOD was 25.3 ± 16.7 and 2.7 ± 5.9, respectively. 64.8 % had a LNR > 0.10 and 64.4 % a LODDS > 10. In univariable analysis, multimodal therapy (p = 0.039), advanced pT (p < 0.0001), advanced UICC stage (p = 0.029), LNR > 0.10 (p = 0.049), and LODDS > −1.0 (p = 0.021) were associated with lower OS. In multivariable analysis, advanced pT [hazard ratio (HR) 2.194; 95 % confidence interval (CI) 1.294–3.722; p = 0.004] and LODDS > −1.0 (HR 1.634; 95 % CI 1.002–2.665; p = 0.059) remained independent predictors for lower OS.
Conclusions
It seems useful to analyze the prognostic significance of LODDS in other samples of HNC.

Similar content being viewed by others
References
Argiris A, Karamouzis MV, Raben D, Ferris RL (2008) Head and neck cancer. Lancet 371:1695–1709
Bernier J et al (2005) Defining risk levels in locally advanced head and neck cancers: a comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (#22931) and RTOG (# 9501). Head Neck 27:843–850
Brannan AG, Johnstone PA, Cooper J (2011) Extracapsular tumor extension in cervical lymph nodes: reconciling the literature and seer data. Head Neck 33:525–528. doi:10.1002/hed.21487
Burusapat C, Jarungroongruangchai W, Charoenpitakchai M (2015) Prognostic factors of cervical node status in head and neck squamous cell carcinoma. World J Surg Oncol 13:51. doi:10.1186/s12957-015-0460-6
Chan AT, Grégoire V, Lefebvre JL, Licitra L, Hui EP, Leung SF, Felip E, EHNS–ESMO–ESTRO Guidelines Working Group (2012) Nasopharyngeal cancer: EHNS–ESMO–ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 23(Suppl 7):vii83–vii85
Chen YL et al (2015) Prognostic influences of lymph node ratio in major cancers of Taiwan: a longitudinal study from a single cancer center. J Cancer Res Clin Oncol 141:333–343
Ebrahimi A, Clark JR, Zhang WJ, Elliott MS, Gao K, Milross CG, Shannon KF (2011a) Lymph node ratio as an independent prognostic factor in oral squamous cell carcinoma. Head Neck 33:1245–1251
Ebrahimi A, Zhang WJ, Gao K, Clark JR (2011b) Nodal yield and survival in oral squamous cancer: defining the standard of care. Cancer 117:2917–2925
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A (2010) AJCC cancer staging manual. Springer, New York
Ghadjar P et al (2010) Quantitative analysis of extracapsular extension of metastatic lymph nodes and its significance in radiotherapy planning in head and neck squamous cell carcinoma. Int J Radiat Oncol Biol Phys 76:1127–1132
Gil Z, Carlson DL, Boyle JO, Kraus DH, Shah JP, Shaha AR, Singh B, Wong RJ, Patel SG (2009) Lymph node density is a significant predictor of outcome in patients with oral cancer. Cancer 115:5700–5710
Grégoire V, Lefebvre JL, Licitra L, Felip E, EHNS–ESMO–ESTRO Guidelines Working Group (2010) Squamous cell carcinoma of the head and neck: EHNS–ESMO–ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 21(Suppl 5):v184–v186
Harari PM et al (2014) Postoperative chemoradiotherapy and cetuximab for high-risk squamous cell carcinoma of the head and neck: Radiation Therapy Oncology Group RTOG-0234. J Clin Oncol 32:2486–2495
Harrell FE Jr (2015) rms: regression modeling strategies. R package version 4.3-1. http://CRAN.R-project.org/package=rms
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Hua YH, Hu QY, Piao YF, Tang Q, Fu ZF (2015) Effect of number and ratio of positive lymph nodes in hypopharyngeal cancer. Head Neck 37:111–116
Kunzel J, Mantsopoulos K, Psychogios G, Agaimy A, Grundtner P, Koch M, Iro H (2015) Lymph node ratio is of limited value for the decision-making process in the treatment of patients with laryngeal cancer. Eur Arch Otorhinolaryngol 272:453–461. doi:10.1007/s00405-014-2997-3
Le Tourneau C, Velten M, Jung GM, Bronner G, Flesch H, Borel C (2005) Prognostic indicators for survival in head and neck squamous cell carcinomas: analysis of a series of 621 cases. Head Neck 27:801–808
Lee CC, Ho HC, Su YC, Lee MS, Hung SK, Chen YL (2015) The prognostic ability of log odds of positive lymph nodes in oral cavity squamous cell carcinoma. Medicine 94:e1069. doi:10.1097/MD.0000000000001069
Lewis JS Jr, Carpenter DH, Thorstad WL, Zhang Q, Haughey BH (2011) Extracapsular extension is a poor predictor of disease recurrence in surgically treated oropharyngeal squamous cell carcinoma. Mod Pathol 24:1413–1420
Marres CC, de Ridder M, Hegger I, van Velthuysen ML, Hauptmann M, Navran A, Balm AJ (2014) The influence of nodal yield in neck dissections on lymph node ratio in head and neck cancer. Oral Oncol 50:59–64
Patel SG et al (2013) Lymph node density in oral cavity cancer: results of the International Consortium for Outcomes Research. Br J Cancer 109:2087–2095
Prabhu RS et al (2015) Lymph node ratio influence on risk of head and neck cancer locoregional recurrence after initial surgical resection: implications for adjuvant therapy. Head Neck 37:777–782
Preuss SF, Klussmann JP, Wittekindt C, Damm M, Semrau R, Drebber U, Guntinas-Lichius O (2007) Long-term results of the combined modality therapy for advanced cervical metastatic head and neck squamous cell carcinoma. Eur J Surg Oncol 33:358–363
Qiu MZ et al (2012) The tumor-log odds of positive lymph nodes-metastasis staging system, a promising new staging system for gastric cancer after D2 resection in China. PLoS ONE 7:e31736. doi:10.1371/journal.pone.0031736
RC Team (2104) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Royston P, Altman DG, Sauerbrei W (2006) Dichotomizing continuous predictors in multiple regression: a bad idea. Stat Med 25:127–141
Shrime MG et al (2009) Nodal ratio as an independent predictor of survival in squamous cell carcinoma of the oral cavity. Head Neck 31:1482–1488
Sobin LH, Gospodarowicz MK, Wittekind C (2010) TNM classification of malignant tumours. Blackwell, Oxford
Song YX et al (2011) Which is the most suitable classification for colorectal cancer, log odds, the number or the ratio of positive lymph nodes? PLoS ONE 6:e28937. doi:10.1371/journal.pone.0028937
Stennert E, Kisner D, Jungehuelsing M, Guntinas-Lichius O, Schröder U, Eckel HE, Klussmann JP (2003) High incidence of lymph node metastasis in major salivary gland cancer. Arch Otolaryngol Head Neck Surg 129:720–723
Sun Z et al (2010) Log odds of positive lymph nodes: a novel prognostic indicator superior to the number-based and the ratio-based N category for gastric cancer patients with R0 resection. Cancer 116:2571–2580
Vaidya AM, Petruzzelli GJ, Clark J, Emami B (2001) Patterns of spread in recurrent head and neck squamous cell carcinoma. Otolaryngol Head Neck Surg 125:393–396
Vander Poorten V, Bradly PJ, Takes RP, Rinaldo A, Woolgar JA, Ferlito A (2012) Diagnosis and management of parotid carcinoma with a special focus on recent advances in molecular biology. Head Neck 34:429–440
Vinh-Hung V et al (2004) Ratios of involved nodes in early breast cancer. Breast Cancer Res 6:R680–R688. doi:10.1186/bcr934
Wang J, Hassett JM, Dayton MT, Kulaylat MN (2008) The prognostic superiority of log odds of positive lymph nodes in stage III colon cancer. J Gastrointest Surg 12:1790–1796
Wittekind C, Compton C, Brierley J, Sobin LH (2012) TNM supplement: a commentary on uniform use. Wiley-Blackwell, Oxford
Acknowledgments
We like to thank all outpatient clinics that were involved in the treatment and data collection of the patients for the cancer registry. We thank the coordinator of the Jena cancer registry, Mrs. Ulrike Burger, for her collaboration.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yildiz, M.M., Petersen, I., Eigendorff, E. et al. Which is the most suitable lymph node predictor for overall survival after primary surgery of head and neck cancer: pN, the number or the ratio of positive lymph nodes, or log odds?. J Cancer Res Clin Oncol 142, 885–893 (2016). https://doi.org/10.1007/s00432-015-2104-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-015-2104-1