Abstract
Purpose
The optimal waiting period between neoadjuvant treatment completion and surgery in locally advanced rectal cancer (LARC) is controversial. The specific purpose of this study was to evaluate the effect of prolonging this interval on the pathologic response, postoperative morbidity, and long-term oncologic outcomes.
Methods
Retrospective data analysis is reported from LARC patients who had been treated with chemoradiation followed by surgery and intra-operative radiotherapy, between February 1995 and December 2012. In total, two groups were studied, according to the time elapsed between neoadjuvant treatment and surgery: conventional interval (CI; <6 weeks) and delayed interval (DI; ≥6 weeks). Clinicopathological data related to tumor response, postoperative morbidity, and oncologic outcomes were compared.
Results
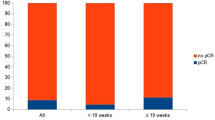
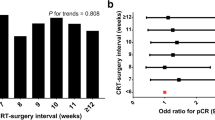
This study included 335 consecutive LARC patients. There was a higher proportion of patients with clinical staging nodal involvement (cN+) in the DI group (76.6 vs. 64.1 %; p = 0.01). The pathologic complete response (pCR) was not significantly different among groups (8.8 vs. 12.1 %; p = 0.34). Longer intervals did not affect complication incidence or severity or hospital admission length. Certain postneoadjuvant tumor effect parameters were significantly increased in the DI group, including N-downstaging and T-downsizing. After a median follow-up of 71 months, patients in the DI group presented with superior 5-year overall survival (OS) (55.9 vs. 70.4 %, p = 0.014); however, no statistically significant differences were observed in 5-year disease-free survival (DFS) or 5-year local control (LC) (69.9 vs. 74.9 %, p = 0.223; 90.4 vs. 94.5 %, p = 0.123, respectively).
Conclusions
A modest surgical interval delay (≥6 weeks) did not increase postoperative complications and was identified as a favorable prognostic factor for OS, although no differences were observed in pCR, LC, or DFS. Innovative multidisciplinary strategies incorporating further time extension of the surgical interval can be safely explored.



Similar content being viewed by others
References
Calvo FA, Gomez-Espí M, Diaz-González JA et al (2002) Intraoperative presacral electron boost following preoperative chemoradiation in T3-4 Nx rectal cancer: initial local effects and clinical outcome analysis. Radiother Oncol 62:201–206
Calvo FA, Serrano FJ, Diaz-Gonzalez JA et al (2006) Improved incidence of pT0 downstaged surgical specimens in locally advanced rectal cancer (LARC) treated with induction oxaliplatin plus 5-fluorouracil and preoperative chemoradiation. Ann Oncol 17:1103–1110
Calvo FA, Sole CV, Serrano J et al (2014) Preoperative chemoradiation with or without induction oxaliplatin plus 5-fluorouracil in locally advanced rectal cancer. Strahlenther Onkol 190:149–157
Campos-Lobato LF, Geisler DP, Moreira AL, Stocchi L, Dietz D, Kalady MF (2011) Neoadjuvant therapy for rectal cancer: the impact of longer interval between chemoradiation and surgery. J Gastrointest Surg 15:444–450
Demicheli R, Retsky MW, Hrushesky WJM, Baum M, Gukas ID (2008) The effects of surgery on tumor growth: a century of investigations. Ann Oncol 19:1821–1828
Dhadda AS, Zaitoun AM, Bessell EM (2009) Regression of rectal cancer with radiotherapy with or without concurrent capecitabine—optimizing the timing of surgical resection. Clin Oncol 21:23–31
Dolinsky CM, Mahmoud NN, Mick R et al (2007) Effect of time interval between surgery and preoperative chemoradiotherapy with 5-fluorouracil or 5-fluorouracil and oxaliplatin on outcomes in rectal cancer. J Surg Oncol 96:207–212
Edge S, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A (2010) AJCC cancer staging manual, 7th edn. Springer, New York
Fiorica F, Cartei F, Licata A et al (2010) Can chemotherapy concomitantly delivered with radiotherapy improve survival of patients with resectable rectal cancer? A meta-analysis of literature data. Cancer Treat Rev 36:539–549
Fisher B, Gunduz N, Saffer E (1983) Influence of the interval between primary tumor removal and chemotherapy on the kinetics of growth of metastasis. Cancer Res 43:1488–1492
Fisher B, Gunduz N, Coyle J, Rudock C, Saffer E (1989) Presence of a growth-stimulating factor in serum following primary tumor removal in mice. Cancer Res 49:1996–2001
François Y, Nemoz CJ, Baulieux J et al (1999) Influence of the interval between preoperative radiation therapy and surgery on downstaging and on the rate of sphincter-sparing surgery for rectal cancer: the Lyon R90-01 randomized trial. J Clin Oncol 17:2396–2402
Garcia-Aguillar J, Smith DD, Avila K et al (2011) Optimal timing of surgery after chemoradiation for advanced rectal cancer: preliminary results of a multi-center, non-randomized phase II prospective trial. Ann Surg 254:97–102
Garland ML, Vather R, Bunkley N, Pearse M, Bissett IP (2014) Clinical tumor size and nodal status predict pathologic complete response following neoadjuvant chemoradiotherapy for rectal cancer. Int J Colorectal Dis 29:301–307
Gérard JP, Azria D, Gourgou-Bourgade S et al (2010) Comparison of two neoadjuvant chemotherapy regimens for locally advanced rectal cancer: results of the phase III trial ACCORD 12/0405—Prodige 2. J Clin Oncol 28:1638–1644
Hofheinz RD, Wenz F, Post S et al (2012) Chemoradiotherapy with capecitabine versus fluorouracil for locally advanced rectal cancer: a randomized, multicenter, non-inferiority, phase 3 trial. Lancet Oncol 13:579–588
Jeong DH, Lee HB, Hur H, Min BS, Baik SH, Kim NK (2013) Optimal timing of surgery after neoadjuvant chemoradiation therapy in locally advanced rectal cancer. J Korean Surg Soc 84:338–345
Kalady MF, Campos-Lobato LF, Stocchi L et al (2009) Predictive factors of pathologic complete response after neoadjuvant chemoradiation for rectal cancer. Ann Surg 250:582–589
Kusters M, Valentini V, Calvo FA et al (2010) Results of European pooled analysis of IORT-containing multimodality treatment for locally advanced rectal cancer: adjuvant chemotherapy prevents local recurrence rather than distant metastasis. Ann Oncol 21:1279–1284
Lim SB, Choi HS, Jeong SY et al (2008) Optimal surgery time after preoperative chemoradiotherapy for locally advanced rectal cancers. Ann Surg 248:243–251
Moore HG, Gittleman AE, Minsky BD et al (2004) Rate of pathologic complete response with increased interval between preoperative combined modality therapy and rectal cancer resection. Dis Colon Rectum 47:279–286
O’Connell MJ (1989) A phase III trial of 5-fluorouracil and leucovorin in the treatment of advanced colorectal cancer. Cancer 63:1026–1030
Rodel C, Liersch T, Becker H et al (2012) Preoperative chemoradiotherapy and postoperative chemotherapy with fluorouracil and oxaplatin versus fluorouracil alone in locally advanced rectal cancer: initial results of the German CAO/ARO/AIO-04 randomized phase 3 trial. Lancet Oncol 13:679–687
Roh MS, Colangelo KH, O’Connell MJ et al (2009) Preoperative multimodality therapy improves disease-free survival in patients with carcinoma of the rectum: NSABP R-03. J Clin Oncol 27:5124–5130
Roh MS, Yothers GA, O’Connell MJ, et al. (2011) The impact of capecitabine and oxaliplatin in the preoperative multimodality treatment in patients with carcinoma of the rectum: NSABP R-04 [abstract]. J Clin Oncol 29 (suppl): abstract 3503
Saglam S, Bugra D, Saglam EK et al (2014) Fourth versus eighth week surgery after neoadjuvant radiochemotherapy in T3-4/N0+ rectal cancer: Istanbul R-01 study. J Gastrointest Oncol 5:9–17
Sauer R, Becker H, Hohenberger W et al (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Eng J Med 351:1731–1740
Sloothaak DAM, Geijsen DE, van Leersum NJ et al (2013) Optimal time interval between neoadjuvant chemoradiotherapy and surgery for rectal cancer. Br J Surg 100:993–999
Sormani MP (2009) The Will Roger phenomenon: the effect of different diagnostic criteria. J Neurol Sci 287(1 Suppl):S46–S49
Stein DE, Mahmoud NN, Anné PR et al (2003) Longer time interval between completion of neoadjuvant chemoradiation and surgical resection does not improve downstaging of rectal carcinoma. Dis Colon Rectum 46:448–453
Tran CL, Udani S, Holt A, Arnell T, Kumar R, Stamos MJ (2006) Evaluation of the safety of increased time interval between chemoradiation and resection for rectal cancer. Am J Surg 192:873–877
Tulchinsky H, Shmueli E, Figer A, Klausner JM, Rabau M (2008) An interval >7 weeks between neoadjuvant therapy and surgery improves pathologic complete response and disease-free survival in patients with locally advanced rectal cancer. Ann Surg Oncol 15:2661–2667
Veenhof AAFA, Kropman RHJ, Engel AF et al (2007) Preoperative radiation therapy for locally advanced rectal cancer: a comparison between two different time intervals to surgery. Int J Colorectal Dis 22:507–513
Wothuis AM, Penninckx F, Haustermans K et al (2012) Impact of interval between neoadjuvant chemoradiotherapy and TME for locally advanced rectal cancer on pathologic response and oncologic outcome. Ann Surg Oncol 19:2833–2841
Common Toxicity Criteria Manual version 2.0 (1999). http://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/ctcmanual_v4_10-4-99.pdf. Accessed 29 May 2014
Zorcolo L, Rosman AS, Restivo A et al (2012) Complete pathologic response after combined modality treatment for rectal cancer and long-term survival: a meta-analysis. Ann Surg Oncol 19:2822–2832
Conflict of interest
The authors report no conflicts of interest. Authors also state that they have complete control of all primary data and they agree the journal to review it, if requested.
Ethical standard
This research was performed in accordance with ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Calvo, F.A., Morillo, V., Santos, M. et al. Interval between neoadjuvant treatment and definitive surgery in locally advanced rectal cancer: impact on response and oncologic outcomes. J Cancer Res Clin Oncol 140, 1651–1660 (2014). https://doi.org/10.1007/s00432-014-1718-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-014-1718-z