Abstract
Purpose
To evaluate the outcome of patients with spinal metastases, treated under palliative considerations by spinal decompression and sole posterior instrumentation, in respect to survival, neurological symptomatology, pain, ECOG grade, and Tomita’s prognostic score (TPS).
Patients and methods
Fifty-seven consecutive patients with metastatic vertebral tumors were treated using a posterolateral approach for decompression combined with posterior instrumentation. Mean age was 58.6 years. In average, 3.4 vertebral segments were involved in instrumentation.
Results
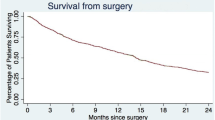
Preoperative mean TPS was 5.9. The majority of the patients (70.2%) presented with an ECOG grade ≤2. The distribution of the metastatic lesions that needed surgical treatment was: 7.8% cervical, 60.9% thoracical, and 31.3% lumbar. In 52.6% the tumor led to pathological vertebral fractures. Mean pain VAS scores improved significantly in all but one patient from 6.6 preoperatively to 3.1 postoperatively. Post-surgical Frankel grades decreased. Mean postoperative survival was 11.4 months. Ten patients survived until now. Forty-seven patients have died with a mean survival of 9 months. Complication rate was only 5.3% with two superficial wound infections and one seroma. Not a single case of posterior spinal instrumentation fatigue failure was detected.
Conclusions
Palliative surgical treatment for metastatic spinal tumors using a decompressive posterolateral approach combined with sole posterior instrumentation achieved convincing clinical results. All patients with intractable pain showed significant improvement postoperatively, and neurological deterioration was avoided. Since patients with spinal metastases enter the terminal stage of their disease, it is generally agreed that they require only palliative surgical treatments. Accordingly, spinal decompression and stabilization may be performed to improve the quality of the remaining life of cancer patients.






Similar content being viewed by others
Abbreviations
- CT:
-
Computerized tomography
- CUP:
-
Cancer of unknown primary origin
- ECOG:
-
Eastern cooperative oncology group
- KPS:
-
Karnowsky performance scale
- MRI:
-
Magnetic resonance imaging
- NHL:
-
Non Hodgkin lymphoma
- PDL:
-
Posterior decompressive laminectomy
- RT:
-
Radiation therapy
- TES:
-
Total en-bloc spondylectomy
- TPS:
-
Tomita’s prognostic score
- VAS:
-
Visual analog scale
References
Bridwell KH, Jenny AB, Saul T, Rich KM, Grubb RL (1988) Posterior segmental spinal instrumentation (PSSI) with posterolateral decompression and debulking for metastatic thoracic and lumbar spine disease. Limitations of the technique. Spine (Phila Pa 1976) 13(12):1383–1394
Catz A, Goldin D, Fishel B, Ronen J, Bluvshtein V, Gelernter I (2004) Recovery of neurologic function following nontraumatic spinal cord lesions in Israel. Spine (Phila Pa 1976) 29(20):2278–2282 (discussion 2283)
Cho DC, Sung JK (2009) Palliative surgery for metastatic thoracic and lumbar tumors using posterolateral transpedicular approach with posterior instrumentation. Surg Neurol 71(4):424–433 (epub 30 Jun 2008)
Decroisette C, Monnet I, Berard H, Quere G, Le Caer H, Bota S, Audigier-Valette C, Geriniere L, Vernejoux JM, Chouaid C, Groupe Français de Pneumo-Cancérologie 0601 Team (2011) Epidemiology and treatment costs of bone metastases from lung cancer: a French prospective, observational, multicenter study (GFPC 0601). J Thorac Oncol 6(3):576–582
Delank KS, Wendtner C, Eich HT, Eysel P (2011) The treatment of spinal metastases. Dtsch Arztebl Int 108(5):71–79; quiz 80 (epub 4 Feb 2011)
Eastern Cooperative Oncology Group (1998) Eastern Cooperative Oncology Group performance status scale. Revised 25 Mar 1998
Ebmeier K, Giest K, Kalff R (2003) Intraoperative computerized tomography for improved accuracy of spinal navigation in pedicle screw placement of the thoracic spine. Acta Neurochir Suppl 85:105–113
Gerszten PC, Welch WC (2000) Current surgical management of metastatic spinal disease. Oncology (Williston Park) 14(7):1013–1024 (discussion 1024, 1029–1030)
Gerszten PC, Welch WC (2007) Combined percutaneous transpedicular tumor debulking and kyphoplasty for pathological compression fractures. Technical note. J Neurosurg Spine 6(1):92–95
Greenlee RT, Murray T, Bolden S, Wingo PA (2000) Cancer statistics, 2000. CA Cancer J Clin 50(1):7–33
Haberland N, Ebmeier K, Hliscs R, Grnewald JP, Silbermann J, Steenbeck J, Nowak H, Kalff R (2000) Neuronavigation in surgery of intracranial and spinal tumors. J Cancer Res Clin Oncol 126(9):529–541
Ibrahim A, Crockard A, Antonietti P, Boriani S, Bünger C, Gasbarrini A, Grejs A, Harms J, Kawahara N, Mazel C, Melcher R, Tomita K (2008) Does spinal surgery improve the quality of life for those with extradural (spinal) osseous metastases? An international multicenter prospective observational study of 223 patients. Invited submission from the joint section meeting on disorders of the spine and peripheral nerves, March 2007. J Neurosurg Spine 8(3):271–278
Jensen AØ, Jacobsen JB, Nørgaard M, Yong M, Fryzek JP, Sørensen HT (2011) Incidence of bone metastases and skeletal-related events in breast cancer patients: a population-based cohort study in Denmark. BMC Cancer 11:29
Kienstra GE, Terwee CB, Dekker FW, Canta LR, Borstlap AC, Tijssen CC, Bosch DA, Tijssen JG (2000) Prediction of spinal epidural metastases. Arch Neurol 57(5):690–695
Klimo P Jr, Dailey AT, Fessler RG (2004) Posterior surgical approaches and outcomes in metastatic spine-disease. Neurosurg Clin N Am 15(4):425–435
Klimo P Jr, Thompson CJ, Kestle JR, Schmidt MH (2005) A meta-analysis of surgery versus conventional radiotherapy for the treatment of metastatic spinal epidural disease. Neuro Oncol 7(1):64–76
Li H, Gasbarrini A, Cappuccio M, Terzi S, Paderni S, Mirabile L, Boriani S (2009) Outcome of excisional surgeries for the patients with spinal metastases. Eur Spine J 18(10):1423–1430 (epub 5 Aug 2009)
Liljenqvist U, Lerner T, Halm H, Buerger H, Gosheger G, Winkelmann W (2008) En bloc spondylectomy in malignant tumors of the spine. Eur Spine J 17(4):600–609 (epub 24 Jan 2008)
Lutz S, Berk L, Chang E, Chow E, Hahn C, Hoskin P, Howell D, Konski A, Kachnic L, Lo S, Sahgal A, Silverman L, von Gunten C, Mendel E, Vassil A, Bruner DW, Hartsell W, American Society for Radiation Oncology (ASTRO) (2011) Palliative radiotherapy for bone metastases: an ASTRO evidence-based guideline. Int J Radiat Oncol Biol Phys 79(4):965–976 (epub 27 Jan 2011)
Maranzano E, Latini P (1995) Effectiveness of radiation therapy without surgery in metastatic spinal cord compression: final results from a prospective trial. Int J Radiat Oncol Biol Phys 32(4):959–967
Melcher I, Disch AC, Khodadadyan-Klostermann C, Tohtz S, Smolny M, Stöckle U, Haas NP, Schaser KD (2007) Primary malignant bone tumors and solitary metastases of the thoracolumbar spine: results by management with total en bloc spondylectomy. Eur Spine J 16(8):1193–1202 (epub 25 Jan 2007)
Mukherjee D, Chaichana KL, Gokaslan ZL, Aaronson O, Cheng JS, McGirt MJ (2011) Survival of patients with malignant primary osseous spinal neoplasms: results from the Surveillance, Epidemiology, and End Results (SEER) database from 1973 to 2003. J Neurosurg Spine 14(2):143–150 (epub 24 Dec 2010)
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5(6):649–655
Placantonakis DG, Laufer I, Wang JC, Beria JS, Boland P, Bilsky M (2008) Posterior stabilization strategies following resection of cervicothoracic junction tumors. J Neurosurg Spine 9(2):111–119
Rades D, Schild SE, Abrahm JL (2010) Treatment of painful bone metastases. Nat Rev Clin Oncol 7(4):220–229 (epub 16 Mar 2010)
Rose PS, Buchowski JM (2011) Metastatic disease in the thoracic and lumbar spine: evaluation and management. J Am Acad Orthop Surg 19(1):37–48
Serlin RC, Mendoza TR, Nakamura Y, Edwards KR, Cleeland CS (1995) When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain 61(2):277–284
Siegal T, Siegal T (1989) Current considerations in the management of neoplastic spinal cord compression. Spine (Phila Pa 1976) 14(2):223–228
Sørensen S, Børgesen SE, Rohde K, Rasmusson B, Bach F, Bøge-Rasmussen T, Stjernholm P, Larsen BH, Agerlin N, Gjerris F et al (1990) Metastatic epidural spinal cord compression. Results of treatment and survival. Cancer 65(7):1502–1508
Tancioni F, Lorenzetti MA, Navarria P, Pessina F, Draghi R, Pedrazzoli P, Scorsetti M, Alloisio M, Santoro A, Rodriguez y Baena R (2011) Percutaneous vertebral augmentation in metastatic disease: state of the art. J Support Oncol 9(1):4–10
Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T (2001) Surgical strategy for spinal metastases. Spine (Phila Pa 1976) 26(3):298–306
Wang JC, Boland P, Mitra N, Yamada Y, Lis E, Stubblefield M, Bilsky MH (2004) Single-stage posterolateral transpedicular approach for resection of epidural metastatic spine tumors involving the vertebral body with circumferential reconstruction: results in 140 patients. Invited submission from the joint section meeting on disorders of the spine and peripheral nerves, March 2004. J Neurosurg Spine 1(3):287–298
Wiggins GC, Mirza S, Bellabarba C, West GA, Chapman JR, Shaffrey CI (2001) Perioperative complications with costotransversectomy and anterior approaches to thoracic and thoracolumbar tumors. Neurosurg Focus 11(6):e4
Young RF, Post EM, King GA (1980) Treatment of spinal epidural metastases. Randomized prospective comparison of laminectomy and radiotherapy. J Neurosurg 53(6):741–748
Acknowledgments
We would like to acknowledge the support and contribution of A. Depta, Dr. H. Schmalenberg, M.D., and co-workers from the Tumor Center of the Friedrich-Schiller-University, Jena.
Conflict of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walter, J., Reichart, R., Waschke, A. et al. Palliative considerations in the surgical treatment of spinal metastases. J Cancer Res Clin Oncol 138, 301–310 (2012). https://doi.org/10.1007/s00432-011-1100-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-011-1100-3