Abstract
Purpose
To examine the incidence, prognosis, clinical and histological characteristics, treatment, and outcome of patients with bilateral testicular cancer in the referral center in Hungary, to determine which parameters might predict a second testicular tumor.
Methods
Clinical parameters—such as time of original surgery, histology of primary tumor, extent of the disease, serum marker concentrations, history of testicular abnormalities, treatment, response to treatment, follow-up period, data on second carcinoma—of bilateral testicular tumors among the 2,386 patients with testicular cancer treated between November 1988 and November 1998 were analyzed.
Results
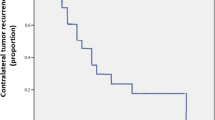
The incidence of patients with synchronous testicular tumor was 0.8% (19 of 2,386 patients). The clinical stages were 8 I/A, 5 I/B, 1 II/A, 2 II/B, 1 III/A, and 2 III/B. Median follow-up time was 93 months and the 5-year overall survival was 84%. The incidence of patients with metachronous testicular cancer (median age 28 years and 35 years at first and second tumor diagnosis) was 2.2% (53 of 2,386 patients) and the median time to second tumor was 76 months (range 18–203 months). The clinical stages at the first and second tumor diagnosis were: 14 I/A, 21 I/B, 15 II/A, 2 II/B, and 1 III/B, and 26 I/A, 16 I/B, 3 II/A, 1 II/B, 7 III/B, respectively. The median follow-up time was 42 months and the 5-year overall survival was 93%. In thirteen patients with metachronous cancers, two family histories of testicular cancer, five cases of undescended testicles, seven cases of testicular atrophy, and one case of azoospermia were detected. There was a non-significant trend to a longer cancer interval after chemotherapy and radiotherapy and a tendency to a greater incidence of asynchronous seminoma after chemotherapy. Clinical stage I tumors were more frequent in the surveyed group than among patients not followed up according to the institutional protocol (P = 0.01), but the survival rate was good in both groups. Seminoma as a second tumor was diagnosed in an older age group (median 38 years, range 25–49 years) than nonseminoma (median 32 years, range 21–51 years, P < 0.045).The interval till the appearance of a metachronous testicular cancer depended on tumor histology: in seminoma cases it was longer than in nonseminoma cases (median time: 121 months versus 50 months, P = 0.002).
Conclusions
The overall incidence of bilateral testicular cancer in the referral center in Hungary was 3%. We could not identify clinical factors which predicted a higher risk for metachronous testicular cancer. With regular follow-up the early diagnosis of second testicular tumors is probable; therefore education, self-examination of the remaining testicle, and long-term follow-up are important in early detection.


Similar content being viewed by others
References
Alberts P, Göl A, Bierhoff E, et al (1999) Clinical course and histopathology risk factor assessment in patients with bilateral testicular germ cell tumors. Urology 54:714–718
Bergstrom R, Adami HO, Mohler M, et al (1996) Increase in testicular cancer incidence in six European countries: a birth cohort phenomenon. J Natl Cancer Inst 88:727–733
Bokemayer C, Schmoll HJ, Schöffski P, et al (1993) Bilateral testicular tumors: prevalence and clinical implications. Eur J Cancer 6:874–876
Colls BM, Harvey VJ, Skelton L, et al (1996) Bilateral germ cell testicular tumors in New Zealand: experience in Auckland and Christchurch 1978–1994. J Clin Oncol 14:2061–2065
Coogan CL, Foster RS, Simmons GR, et al (1998) Bilateral testicular tumors. Cancer 83:547–552
Dieckmann KP, Loy V (1996) Prevalence of contralateral testicular intraepithelial neoplasia in patients with testicular germ cell neoplasms. J Clin Oncol 14:3126–3132
Einhorn LH (1997) Testicular cancer: an oncological success story. Clin Cancer Res 3:2630–2632
Géczi L, Gomez F, Horváth Z, et al (2001) Three-year results of the first educational and early detection program for testicular cancer. Oncology 60:228–234
Harland SJ, Cook PA, Fossa SD, et al (1993) Risk factors for carcinoma in situ of the contralateral testis in patients with testicular cancer. An Interim report. Eur Urol 23:115–119
Hartmann JT, Kanz L, Bokemayer C (1999) Diagnosis and treatment of patients with testicular germ cell cancer. Drugs 58:257–281
Loy V, Dieckmann KP (1993) Prevalence of contralateral testicular intraepithelial neoplasia (carcinoma in situ) in patients with germ cell tumor. Results of the German Multicentre Study. Eur Urol 23:120–122
Mostofi FK, Sesterhenn IA, Davis C (1986) World Health Organisation international histological classification of germ cell tumors of the testis. In: Jones WG, Milford WA, Anderson CK (eds) Germ-cell tumours, vol. 2. Pergamon, Oxford, pp 1–23
Osterlind A, Berthelsen JG, Abildgaard N, et al (1991) Risk of bilateral testicular germ cell cancer in Denmark: 1960–1984. J Natl Cancer Inst 83:1391–1395
Reinberg Y, Manivel JC, Zhang G, et al (1991) Synchronous bilateral testicular germ cell tumors of different histologic type. Pathogenetic and practical implication of bilaterality in testicular germ cell tumors. Cancer 68:1085–1085
Sobin LH, Wittekind C (1997) UICC TNM Classification of malignant tumors. Wiley-Liss, New York, pp 174–179
Sokal M, Peckham MJ, Hendry F (1980) Bilateral germ cell tumours of the testis. Br J Urology 52:158–162
Sonneveld DJA, Schraffordt Koops H, Sleifer DTh, et al (1998) Bilateral testicular germ cell tumours in patients with initial stage I disease: prevalence and prognosis—a single centre's 30-years' experience. Eur J Cancer 34:1363–1367
Tekin A, Aygun YC, Aki FT, et al (2000) Bilateral germ cell cancer of the testis: a report of 11 patients with long-term follow-up. BJU Int 85:864–868
Thompson Y, Williams CJ, Whitehouse JMA, et al (1988) Bilateral testicular germ cell tumors: an increasing incidence and prevention by chemotherapy. Brit J Urol 62:374–376
Van Basten JPA, Hoekstra HJ, Van Driel MF, et al (1997) Cisplatin-based chemotherapy changes the incidence of bilateral testicular cancer. Ann Surg Oncol 4:342–348
Wanderas EH, Fossa SD, Tretli S (1997) Risk of a second germ cell cancer after treatment of a primary germ cell cancer in 2201 Norwegian male patients. Eur J Cancer 33:244–52
Acknowledgements
The authors thank Prof. Ian Tannock (Princess Margaret Hospital and University of Toronto, Canada) for his help in the correction of the manuscript. The authors also thank the urological, surgical, and oncological centers whose cooperation makes it possible to have a centralized treatment strategy for testicular cancer in Hungary.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Géczi, L., Gomez, F., Bak, M. et al. The incidence, prognosis, clinical and histological characteristics, treatment, and outcome of patients with bilateral germ cell testicular cancer in Hungary. J Cancer Res Clin Oncol 129, 309–315 (2003). https://doi.org/10.1007/s00432-003-0437-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-003-0437-7