Abstract
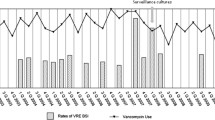
In order to determine the extent of vancomycin resistant enterococcus (VRE) colonisation within a paediatric oncology unit, the risk factors for the acquisition of the organism, the molecular epidemiology of the isolates and the impact of infection control measures, extensive patient and environmental surveillance was undertaken with identification, antibiotic susceptibility testing and pulsed-field gel electrophoresis (PFGE) of all VRE isolates. A matched case control study was carried out. Fourteen patients (19% of screened patients) with VRE colonisation were identified (12 with Enterococcus faecium). All isolates manifested the Van A phenotype. Extensive environmental contamination with VRE was present. PFGE of E. faecium isolates from 10 patients and from five of six environmental cultures revealed patterns suggesting genetic relatedness. Following comparison of the 14 cases with 41 controls matched for age (±4 years) and cohabitation on the oncology unit, risk factors for colonisation with VRE included duration of neutropenia, (OR, 3.72; 95% CI, 1.0–13.1), and antibiotic therapy, (OR, 4.07; 95% CI, 1.08–15.3), the number of antibiotic agents received, (OR, 8.4; 95% CI, 1.34–34.3) and the duration of therapy with amikacin, (OR, 10.7; 95% CI, 1.4–81.5), ceftazidime, (OR, 11.5; 95% CI, 2.2–59.9) or teicoplanin, (OR, 12.3; 95% CI, 2.25–67.4). Implementation of stringent infection control measures reduced environmental contamination from 25% of samples in week 1 to none in week 11. Two additional colonised patients were identified during the subsequent 6 months.
Conclusion Risk factors for VRE colonization in paediatric oncology patients included duration of neutropenia, duration of any antibiotic therapy, exposure to ceftazidime, amikacin or teicoplanin and the number of antibiotics used. The study suggests that environmental contamination played an important role in patient-to-patient transmission of VRE and interventions including implementation of infection control measures were associated with a decreased incidence of gastro-intestinal colonisation.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Received: 18 February 1997 and in revised form: 6 May 1997 / Accepted: 13 May 1997
An erratum to this article is available at http://dx.doi.org/10.1007/s004310050839.
Rights and permissions
About this article
Cite this article
Nourse, C., Murphy, H., Byrne, C. et al. Control of a nosocomial outbreak of vancomycin resistant Enterococcus faecium in a paediatric oncology unit: risk factors for colonisation. Eur J Pediatr 157, 20–27 (1998). https://doi.org/10.1007/s004310050760
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s004310050760