Abstract
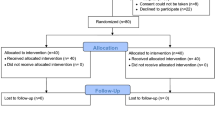
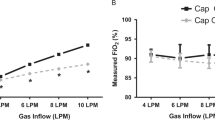
The establishment of adequate ventilation is the cornerstone of neonatal resuscitation in the delivery room (DR). This parallel-group, accessor-blinded randomized controlled trial compared the changes in peripheral oxygen saturation (SpO2), heart rate (HR), and cerebral regional oxygen saturation (crSO2) with the use of a T-piece resuscitator (TPR) versus self-inflating bag (SIB) as a mode of providing positive pressure ventilation (PPV) during DR resuscitation in preterm neonates. Seventy-two preterm neonates were randomly allocated to receive PPV with TPR (n = 36) or SIB (n = 36). The primary outcome was SpO2 (%) at 5 min. The secondary outcomes included the time to achieve a SpO2 ≥ 80% and > 85%, HR > 100/min, fractional-inspired oxygen (FiO2) requirement, minute-specific SpO2, HR and FiO2 trends for the first 5 min of life, need for DR-intubation, crSO2, need and duration of respiratory support, and other in-hospital morbidities. Mean SpO2 at 5 min was 74.5 ± 17.8% and 69.4 ± 22.4%, in TPR and SIB groups, respectively [Mean difference, 95% Confidence Interval 5.08 (-4.41, 14.58); p = 0.289]. No difference was observed in the time to achieve a SpO2 ≥ 80% and > 85%, HR > 100/min, the requirement of FiO2, DR-intubation, and the need and duration of respiratory support. There was no significant difference in the minute-specific SpO2, HR, and FiO2 requirements for the first 5 min. CrSO2 (%) at one hour was lower by 5% in the TPR group compared to SIB; p = 0.03. Other complications were comparable.
Conclusions: TPR and SIB resulted in comparable SpO2 at 5 min along with similar minute-specific SpO2, HR, and FiO2 trends.
Clinical Trial Registration: Clinical trial registry of India, Registration no: CTRI/2021/10/037384, Registered prospectively on: 20/10/2021, https://ctri.icmr.org.in/.
What is Known: • Compared to self-inflating bags (SIB), T-piece resuscitators (TPR) provide more consistent inflation pressure and tidal volume as shown in animal and bench studies. • There is no strong recommendation for one device over the other in view of low certainty evidence. | |
What is New: • TPR and SIB resulted in comparable peripheral oxygen saturation (SpO2) at 5 min along with similar minute-specific SpO2, heart rate, and fractional-inspired oxygen requirement trends. • Short-term complications and mortality rates were comparable with both devices. |



Similar content being viewed by others
Availability of data and material
Deidentified individual participant data (including data dictionaries) will be made available, in addition to study protocols, the statistical analysis plan, and the informed consent form. The data will be made available upon publication to researchers who provide a methodologically sound proposal for use in achieving the goals of the approved proposal. Proposals should be submitted to: bhrajishna@gmail.com.
Code availability
N/A.
Abbreviations
- DR:
-
Delivery room
- PPV:
-
Positive pressure ventilation
- GA:
-
Gestational age
- SIB:
-
Self-inflating bag
- FIB:
-
Flow-inflating bag
- TPR:
-
T-piece resuscitator
- PIP:
-
Peak inspiratory pressure
- VT :
-
Tidal volume
- PEEP:
-
Positive end-expiratory pressure
- SpO2 :
-
Peripheral oxygen saturation
- HR:
-
Heart rate
- IVH:
-
Intraventricular hemorrhage
- CrSO2 :
-
Cerebral regional oxygen saturation
- RCT:
-
Randomized controlled trial
- CTRI:
-
Clinical Trial Registry of India
- AHA-NRP:
-
American Heart Association-Neonatal Resuscitation Program
- FiO2 :
-
Fractional inspired oxygen
- NIRS:
-
Near-infrared spectroscopy
- MAP:
-
Mean arterial pressure
- hs-PDA:
-
Hemodynamically significant patent ductus arteriosus
- NEC:
-
Necrotizing enterocolitis
- SIP:
-
Spontaneous intestinal perforation
- PVL:
-
Periventricular leukomalacia
- ROP:
-
Retinopathy of prematurity
- BPD:
-
Bronchopulmonary dysplasia
- NICU:
-
Neonatal intensive care unit
- SD:
-
Standard deviation
- ITT:
-
Intention to treat
- IQR:
-
Interquartile range
- MD:
-
Mean difference
- CI:
-
Confidence interval
- RR:
-
Risk Ratio
- OR:
-
Odds ratio
References
Aziz K, Lee CHC, Escobedo MB, Hoover AV, Kamath-Rayne BD, Kapadia VS et al (2021) Part 5: Neonatal Resuscitation 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics 147:e2020038505E. https://doi.org/10.1542/peds.2020-038505E
Ersdal HL, Mduma E, Svensen E, Perlman JM (2012) Early initiation of basic resuscitation interventions including face mask ventilation may reduce birth asphyxia related mortality in low-income countries: a prospective descriptive observational study. Resuscitation 83:869–873. https://doi.org/10.1016/j.resuscitation.2011.12.011
Bjorland PA, Øymar K, Ersdal HL, Rettedal SI (2019) Incidence of newborn resuscitative interventions at birth and short-term outcomes: a regional population-based study. BMJ Paediatr Open 3:e000592. https://doi.org/10.1136/bmjpo-2019-000592
Niles DE, Cines C, Insley E, Foglia EE, Elci OU, Skåre C et al (2017) Incidence and characteristics of positive pressure ventilation delivered to newborns in a US tertiary academic hospital. Resuscitation 115:102–109. https://doi.org/10.1016/j.resuscitation.2017.03.035
Roehr CC, O’Shea JE, Dawson JA, Wyllie JP (2018) Devices used for stabilisation of newborn infants at birth. Arch Dis Child Fetal Neonatal Ed 103:F66-71. https://doi.org/10.1136/archdischild-2016-310797
Tracy MB, Halliday R, Tracy SK, Hinder MK (2019) Newborn self-inflating manual resuscitators: precision robotic testing of safety and reliability. Arch Dis Child Fetal Neonatal Ed 104:F403–F408. https://doi.org/10.1136/archdischild-2018-315391
Hinder M, McEwan A, Drevhammer T, Donaldson S, Tracy MB (2019) T-piece resuscitators: how do they compare? Arch Dis Child Fetal Neonatal Ed 104:F122–F127. https://doi.org/10.1136/archdischild-2018-314860
Rafferty AR, Johnson L, Maxfield D, Dawson JA, Davis PG, Thio M (2016) The accuracy of delivery of target pressures using self-inflating bag manometers in a benchtop study. Acta Paediatr 105:e247–e251. https://doi.org/10.1111/apa.13397
Hartung JC, Dold SK, Thio M, tePas A, Schmalisch G, Roehr CC (2014) Time to adjust to changes in ventilation settings varies significantly between different T-piece resuscitators, self-inflating bags, and manometer equipped self-inflating bags. Am J Perinatol 31:505–512. https://doi.org/10.1055/s-0033-1354562
Roehr CC, Kelm M, Fischer HS, Bührer C, Schmalisch G, Proquitté H (2010) Manual ventilation devices in neonatal resuscitation: tidal volume and positive pressure-provision. Resuscitation 81:202–205. https://doi.org/10.1016/j.resuscitation.2009.10.008
Hawkes CP, Ryan CA, Dempsey EM (2012) Comparison of the T-piece resuscitator with other neonatal manual ventilation devices: a qualitative review. Resuscitation 83:797–802. https://doi.org/10.1016/j.resuscitation.2011.12.020
Wyckoff MH, Wyllie J, Aziz K, de Almeida MF, Fabres JW, Fawke J: Neonatal Life Support Collaborators, et al (2020) Neonatal Life Support 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation 156:A156–A187. https://doi.org/10.1016/j.resuscitation.2020.09.015
Madar J, Roehr CC, Ainsworth S, Ersdal H, Morley C, Rüdiger M et al (2021) European Resuscitation Council Guidelines 2021: Newborn resuscitation and support of transition of infants at birth. Resuscitation 161:291–326. https://doi.org/10.1016/j.resuscitation.2021.02.014
Katheria AC, Hassen K, Rich W, Poeltler D, Finer N (2019) Resuscitation outcomes of infants that do not achieve a 5 min target SpO2 saturation. J Perinatol 39:1635–1639. https://doi.org/10.1038/s41372-019-0491-x
Oei JL, Finer NN, Saugstad OD, Wright IM, Rabi Y, Tarnow-Mordi W et al (2018) Outcomes of oxygen saturation targeting during delivery room stabilisation of preterm infants. Arch Dis Child Fetal Neonatal Ed 103:F446–F454. https://doi.org/10.1136/archdischild-2016-312366
Dawson JA, Schmölzer GM, Kamlin CO, Te Pas AB, O'Donnell CP, Donath SM et al (2011) Oxygenation with T-piece versus self-inflating bag for ventilation of extremely preterm infants at birth: a randomized controlled trial. J Pediatr 158:912–8.e1–2. https://doi.org/10.1016/j.jpeds.2010.12.003
Szyld E, Aguilar A, Musante GA, Vain N, Prudent L, Fabres J et al, Delivery Room Ventilation Devices Trial Group (2014) Comparison of devices for newborn ventilation in the delivery room. J Pediatr 165:234–239.e3. https://doi.org/10.1016/j.jpeds.2014.02.035
Cimatti AG, Martini S, Galletti S, Vitali F, Aceti A, Frabboni G et al (2020) Cerebral Oxygenation and Autoregulation in Very Preterm Infants Developing IVH During the Transitional Period: A Pilot Study. Front Pediatr 8:381. https://doi.org/10.3389/fped.2020.00381
Wolfsberger CH, Pichler-Stachl E, Höller N, Mileder LP, Schwaberger B, Avian A et al (2023) Cerebral oxygenation immediately after birth and long-term outcome in preterm neonates-a retrospective analysis. BMC Pediatr 23:145. https://doi.org/10.1186/s12887-023-03960-z
Schwaberger B, Pichler G, Binder C, Avian A, Pocivalnik M, Urlesberger B (2014) Even mild respiratory distress alters tissue oxygenation significantly in preterm infants during neonatal transition. Physiol Meas 35:2085–2099. https://doi.org/10.1088/0967-3334/35/10/2085
Mariani G, Dik PB, Ezquer A, Aguirre A, Esteban ML, Perez C et al (2007) Pre-ductal and post-ductal O2 saturation in healthy term neonates after birth. J Pediatr 150(4):418–421. https://doi.org/10.1016/j.jpeds.2006.12.015
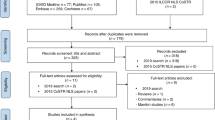
Tribolet S, Hennuy N, Rigo V (2023) Ventilation devices for neonatal resuscitation at birth: A systematic review and meta-analysis. Resuscitation 183:109681. https://doi.org/10.1016/j.resuscitation.2022.109681
Trevisanuto D, Roehr CC, Davis PG, Schmölzer GM, Wyckoff MH, Liley HG: INTERNATIONAL LIAISON COMMITTEE ON RESUSCITATION NEONATAL LIFE SUPPORT TASK FORCE, et al (2021) Devices for Administering Ventilation at Birth: A Systematic Review. Pediatrics 148:e2021050174. https://doi.org/10.1542/peds.2021-050174
Bellos I, Pillai A, Pandita A (2022) Providing Positive End Expiratory Pressure during Neonatal Resuscitation: A Meta-analysis. Am J Perinatol. https://doi.org/10.1055/a-1933-7235
Evans N, Kluckow M (1996) Early determinants of right and left ventricular output in ventilated preterm infants. Arch Dis Child Fetal Neonatal Ed 74:F88-94. https://doi.org/10.1136/fn.74.2.f88
Pichler G, Urlesberger B, Baik N, Schwaberger B, Binder-Heschl C, Avian A et al (2016) Cerebral Oxygen Saturation to Guide Oxygen Delivery in Preterm Neonates for the Immediate Transition after Birth: A 2-Center Randomized Controlled Pilot Feasibility Trial. J Pediatr 170:73–8.e1–4. https://doi.org/10.1016/j.jpeds.2015.11.053
Acknowledgements
We would like to thank all the study infants and their families who accepted joining this study.
Funding
There is no external funding source.
Author information
Authors and Affiliations
Contributions
S.B., B.P., M.P., P.S., S.K., and S.C. conceptualized and designed the study, coordinated, and supervised data collection, drafted the initial manuscript, and reviewed and revised the manuscript. All authors reviewed and approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institute Ethics Committee of All India Institute of Medical Sciences, Rishikesh, India (AIIMS/IEC/21/518, Dated 02/09/2021).
Consent for publication
Written informed consent was obtained from all the parents of the study participants for publication of their data.
Consent to participate
Written informed consent was obtained from all the parents of the study participants.
Competing interest
The research was not sponsored by any funding organization and none of the authors have any financial disclosure to make.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pallapothu, B., Priyadarshi, M., Singh, P. et al. T-Piece resuscitator versus self-inflating bag for delivery room resuscitation in preterm neonates: a randomized controlled trial. Eur J Pediatr 182, 5565–5576 (2023). https://doi.org/10.1007/s00431-023-05230-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05230-7