Abstract
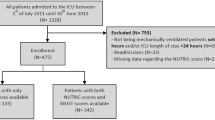
Feed intolerance (FI) is significantly associated with poor prognosis in critically ill patients. This study aimed to understand the characteristics of children with FI and identify the factors predicting FI in critically ill children. This retrospective cohort study was conducted between January 2017 and June 2022 in the Pediatric Intensive Care Unit of a specialized children’s hospital. Eighteen factors, including age, body mass index for age z-score (BAZ) < -2, paediatric index of mortality (PIM)3 score, Glasgow coma scale score, mechanical ventilation (MV), enteral nutrition delay, vasoactive drugs, sedatives, sepsis, heart disease, neurological disease, hypokalemia, arterial PH < 7.35, arterial partial pressure of oxygen (PaO2), blood glucose, hemoglobin, total protein, and albumin, were retrieved to predict FI. The outcome was FI during PICU stay. During the study period, a total of 854 children were included, of which 215 children developed FI. Six predictors of FI were selected: PIM3 score, MV, sepsis, hypokalemia, albumin, and PaO2. Multivariate logistic regression analysis showed that higher PIM3 score, MV, sepsis, hypokalemia, and lower PaO2 were independent risk factors for FI, whereas higher albumin was an independent protective factor for FI. The C-index of the predictive nomogram of 0.943 was confirmed at internal validation to be 0.940, indicating a good predictive value of the model. Decision curve analysis shows good clinical applicability of the nomogram in predicting FI.
Conclusion: The nomogram was verified to have a good prediction performance based on discrimination, calibration, and clinical decision analysis.
What is Known: • Research has demonstrated that gastrointestinal (GI) dysfunction is not only a fundamental element of Multiple Organ Dysfunction Syndrome (MODS), but also the initiator of MODS. • Previous study has demonstrated a significant association between FI and poor prognosis in critically ill patients. | |
What is New: • We excluded patients with primary gastrointestinal tract disease from our study, and we observed an incidence of FI of 25.2% in the Pediatric Intensive Care Unit (PICU). • Our study revealed that PIM3 score, MV, sepsis, hypokalemia, albumin, and PaO2 are significant predictors of FI. |




Similar content being viewed by others
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BAZ:
-
Body mass index for age z-score
- DCA:
-
Decision curve analysis
- EN:
-
Enteral nutrition
- FI:
-
Feed intolerance
- GCS:
-
Glasgow coma scale
- GI:
-
Gastrointestinal
- ICU:
-
Intensive care unit
- LASSO:
-
Least absolute shrinkage and selection operator
- MODS:
-
Multiple Organ Dysfunction Syndrome
- MV:
-
Mechanical ventilation
- PaO2 :
-
Arterial partial pressure of oxygen
- PICU:
-
Pediatric Intensive Care Unit
- PIM:
-
Paediatric index of mortality
References
Zeeshan A, Nairn Q, Jawwad M et al (2023) Impact of Nutrition Support Team in Achieving Target Calories in Children Admitted in Pediatric Intensive Care Unit. J Pediatr Gastroenterol Nutr 74:830–836. https://doi.org/10.1097/MPG.00000000000034381
Leite P, de Lima F, de Oliveira IB et al (2013) Malnutrition may worsen the prognosis of critically ill children with hyperglycemia and hypoglycemia. J Parenter Enteral Nutr 37:335–341. https://doi.org/10.1177/01486071124581241
Bechard J, Staffa J, Zurakowski D et al (2021) Time to achieve delivery of nutrition targets is associated with clinical outcomes in critically ill children. Am J Clin Nutr 114:1859–1867. https://doi.org/10.1093/ajcn/nqab2441
Eveleens D, Hulst M, de Koning E et al (2021) Achieving enteral nutrition during the acute phase in critically ill children: Associations with patient characteristics and clinical outcome. Clin Nutr 40:1911–1919. https://doi.org/10.1016/j.clnu.2020.09.0051
Cederholm T, Barazzoni R, Austin P et al (2017) ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr 36:49–64. https://doi.org/10.1016/j.clnu.2016.09.0041
Schörghuber M, Fruhwald S (2018) Effects of enteral nutrition on gastrointestinal function in patients who are critically ill. Lancet Gastroenterol Hepatol 34:281–287. https://doi.org/10.1016/S2468-1253(18)30036-0
Quiroz-Olguín G, Gutiérrez-Salmeán G, Posadas-Calleja G et al (2021) The effect of enteral stimulation on the immune response of the intestinal mucosa and its application in nutritional support. Eur J Clin Nutr 75:1533–1539. https://doi.org/10.1038/s41430-021-00877-7
Kudsk A (2021) Current aspects of mucosal immunology and its influence by nutrition. Am J Surg 183:390–398. https://doi.org/10.1016/s0002-9610(02)00821-8
Klingensmith J, Coopersmith M (2016) The Gut as the Motor of Multiple Organ Dysfunction in Critical Illness. Crit Care Clin 32:203–212. https://doi.org/10.1016/j.ccc.2015.11.004
Eveleens D, Joosten M, de Koning E et al (2020) Definitions, predictors and outcomes of feeding intolerance in critically ill children: A systematic review. Clin Nutr 39:685–693. https://doi.org/10.1016/j.clnu.2019.03.026
Mehta M, Bechard J, Cahill N et al (2012) Nutritional practices and their relationship to clinical outcomes in critically ill children– an international multicenter cohort study. Crit Care Med 40:2204–2211. https://doi.org/10.1097/CCM.0b013e31824e18a8
Tume LN, Valla FV (2018) A review of feeding intolerance in critically ill children. Eur J Pediatr 177:1675–1683. https://doi.org/10.1007/s00431-018-3229-4
Sanchez C, Lopez-Herce J, Moreno de Guerra M et al (2000) The use of transpyloric enteral nutrition in the critically ill child. J Intensive Care Med 15:247–254. https://doi.org/10.1177/088506660001500503
Lu M, Jia S, Wang R et al (2022) Development of a prediction model for enteral feeding intolerance in intensive care unit patients: A prospective cohort study. World J Gastrointest Surg 14:1363–1374. https://doi.org/10.4240/wjgs.v14.i12.1363
Wolf E, Jeschke G, Rose K et al (1997) Enteral feeding intolerance: an indicator of sepsis-associated mortality in burned children. Arch Surg 132:1310–1313. https://doi.org/10.1001/archsurg.1997.01430360056010
Gungabison U, Hacquoil K, Bains C et al (2015) Prevalence, risk factors, clinical consequences, and treatment of enteral feed intolerance during critical illness. J Parenter Enteral Nutr 39:41–48. https://doi.org/10.1177/0148607114526450
Mittal R, Coopersmith M (2014) Redefining the gut as the motor of critical illness. Trends Mol Med 20:214–223. https://doi.org/10.1016/j.molmed.2013.08.004
Straney L, Clements A, Parslow C et al (2013) Paediatric index of mortality 3: an updated model for predicting mortality in pediatric intensive care. Pediatr Crit Care Med 14:673–681. https://doi.org/10.1016/j.jpeds.2020.05.016
Jacobs A, Flechet M, Vanhorebeek I et al (2019) Performance of Pediatric Mortality Prediction Scores for PICU Mortality and 90-Day Mortality. Pediatr Crit Care Med 20:113–119. https://doi.org/10.1097/PCC.0000000000001764
Wong M, Hornik P, Mok H et al (2018) Performance of the Paediatric Index of Mortality 3 and Paediatric Logistic Organ Dysfunction 2 Scores in Critically III Children. Ann Acad Med Singap 47:285–90. https://doi.org/10.47102/annals-acadmedsg.V47N8p285
Hsu HP, Shan YS, Hsieh YH et al (2006) Impact of etiologic factors and APACHE II and POSSUM scores in management and clinical outcome of acute intestinal ischemic disorders after surgical treatment. World J Surg 30:2152–2162. https://doi.org/10.1007/s00268-005-0716-3
Gajic O, Urrutia LE, Sewani H et al (2002) Acute abdomen in the medical intensive care unit. Crit Care Med 30:1187–1190. https://doi.org/10.1097/00003246-200206000-00001
Sun JK, Liu Y, Zou L et al (2020) Acute gastrointestinal injury in critically ill patients with COVID-19 in Wuhan, China. World J Gastroenterol 26:6087–97. https://doi.org/10.3748/wjg.v26.i39.6087
Takedani Y, Nakamura T, Fukiwake N et al (2021) Clinical characteristics and factors related to antibiotic-associated diarrhea in elderly patients with pneumonia: a retrospective cohort study. BMC Geriatr 21:317. https://doi.org/10.1186/s12877-021-02267-x
Wennogle SA, Priestnall SL, Suárez-Bonnet A et al (2019) Lymphatic endothelial cell immunohistochemical markers for evaluation of the intestinal lymphatic vasculature in dogs with chronic inflammatory enteropathy. J Vet Intern Med 33:1669–1676. https://doi.org/10.1111/jvim.15545
Sestan M, Kifer N, Frkovic M et al (2021) Gastrointestinal involvement and its association with the risk for nephritis in IgA vasculitis. Ther Adv Musculoskelet Dis 13:1759720. https://doi.org/10.1177/1759720X211024828
Nagamori T, Oka H, Koyano S et al (2014) Construction of a scoring system for predicting the risk of severe gastrointestinal involvement in Henoch-Schönlein Purpura. Springerplus 3:171. https://doi.org/10.1186/2193-1801-3-171
Zhao X, Wang Y, Yang Y et al (2022) Association between preoperative nutritional status, inflammation, and intestinal permeability in elderly patients undergoing gastrectomy: a prospective cohort study. J Gastrointest Oncol 13:997–1006. https://doi.org/10.21037/jgo-22-367
van der Hulst RR, von Meyenfeldt MF, van Kreel BK et al (1998) Gut permeability, intestinal morphology, and nutritional depletion. Nutrition 14:1–6. https://doi.org/10.1016/s0899-9007(97)00385-7
Steiner M, Bourges HR, Freedman LS et al (1968) Effect of starvation on the tissue composition of the small intestine in the rat. Am J Physiol 215:75–77. https://doi.org/10.1152/ajplegacy.1968.215.1.75
Sherman P, Forstner J, Roomi N et al (1985) Mucin depletion in the intestine of malnourished rats. Am J Physiol 248:G418–G423. https://doi.org/10.1152/ajpgi.1985.248.4.G418
Dive A, Moulart M, Jonard P et al (1994) Gastroduodenal motility in mechanically ventilated critically ill patients: a manometric study. Crit Care Med 22:441–447. https://doi.org/10.1097/00003246-199403000-00014
Ukleja A (2010) Altered GI motility in critically ill patients: current understanding of pathophysiology, clinical impact, and diagnostic approach. Nutr Clin Pract 25:16–25. https://doi.org/10.1177/0884533609357568
Garcia-Alvarez M, Marik P, Bellomo R (2014) Sepsis-associated hyperlactatemia. Crit Care 18(5):503. https://doi.org/10.1186/s13054-014-0503-3
Haussner F, Chakraborty S, Halbgebauer R et al (2019) Challenge to the Intestinal Mucosa During Sepsis. Front Immunol 10:891. https://doi.org/10.3389/fimmu.2019.00891
Heyland DK, Ortiz A, Stoppe C et al (2021) Incidence, Risk Factors, and Clinical Consequence of Enteral Feeding Intolerance in the Mechanically Ventilated Critically Ill: An Analysis of a Multicenter, Multiyear Database. Crit Care Med 49:49–59. https://doi.org/10.1097/CCM.0000000000004712
Clausen MJ, Poulsen H (2013) Sodium/potassium homeostasis in the cell. Met Ions Life Sci 12:41–67. https://doi.org/10.1007/978-94-007-5561-1_3
Sigrid AR, Sonali PB, Jegan G et al (2007) Na-K-ATPase regulates tight junction permeability through occluding phosphorylation in pancreatic epithelial cells. Am J Physiol Gastrointest Liver Physiol 292:G124-133. https://doi.org/10.1152/ajpgi.00297.2006
Liu D, Lin Y, Gong N et al (2021) Degree and duration of hypokalemia associated with peritonitis in patients undergoing peritoneal dialysis. Int J Clin Pract 75:e14188. https://doi.org/10.1111/ijcp.14188
Wu H, Huang R, Fan J et al (2022) Low potassium disrupt intestinal barrier and result in bacterial translocation. J Transl Med 20:309. https://doi.org/10.1186/s12967-022-03499-0
Szabo JS, Stonestreet BS, Oh W (1985) Effects of hypoxemia on gastrointestinal blood flow and gastric emptying in the newborn piglet. Pediatr Res 19:466–471. https://doi.org/10.1203/00006450-198505000-00012
Acknowledgements
We appreciate all of participants who enrolled in this study.
Funding
This work was funded by Tianjin Key Medical Discipline (Specialty) Construction Project (TJYXZDXK-040A) and Tianjin Natural Science Fund (21JCYBJC00890).
Author information
Authors and Affiliations
Contributions
Ying Lin designed the research.Ying Lin, Junhong Yang, and Xiaomin Wang conducted the research.Ying Lin and Junhong Yang provided data analysis.Ying Lin, Liping Zhang, Lijing Wang, Lingyan Li, and Yun Gou conducted data collection.Liping Zhang and Lijing Wang provided data interpretation.Ying Lin drafted the manuscript. Junhong Yang and Xiaomin Wang revised the manuscript. All authors contributed to writing and editing the final paper.
Corresponding author
Ethics declarations
Ethical approval
The study was conducted in accordance with the ethical principles laid down in the “Declaration of Helsinki”. It was approved by the hospital Ethics Committee (Ethics Committee of Tianjin Children’s Hospital, No.: L2023-005). Due to the retrospective nature of this study, the ethics committee was exempted from signing the subject informed consent form.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, Y., Wang, X., Li, L. et al. Nomogram to predict feeding intolerance in critically ill children. Eur J Pediatr 182, 5293–5302 (2023). https://doi.org/10.1007/s00431-023-05205-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05205-8