Abstract
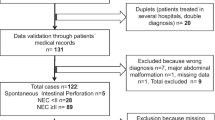
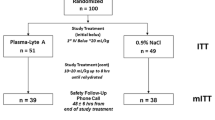
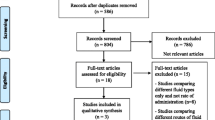
Acute gastroenteritis is one of the main causes of electrolyte imbalance in infants. We aimed to determine the frequency of and factors associated with dysnatremia at presentation and establish the ideal intravenous treatment scheme. The records of hospitalized infants aged 1–12 months with community-acquired acute gastroenteritis between January 2017 and March 2021 were retrospectively reviewed. Factors associated with dysnatremia at presentation were analyzed by multivariable logistic regression analysis. Subsequent sodium levels 4–24 h after intravenous fluid treatments, which were categorized into 2 groups, were determined in the subgroup of infants with normal sodium levels at presentation. A total of 347 infants with a median age of 8.0 (5.0–10.0) months were included. The frequency of dysnatremia at presentation was 14% (hyponatremia 12% and hypernatremia 2.0%). Severe dehydration was associated with dysnatremia at presentation (p = 0.048). Among 68 infants with normal sodium levels at presentation, the median sodium change was highest in the 5% dextrose in saline group, with changes of + 3 (0.5–5) and + 1 (− 2 to 2) mmol/L in infants who received 5% dextrose in saline and 5% dextrose in 1/3–1/2 saline, respectively (p = 0.001). Four out of 47 infants (8.5%) developed hyponatremia while receiving 5% dextrose in 1/3–1/2 saline. None of those who received 5% dextrose in saline developed subsequent dysnatremia.
Conclusion: The frequency of dysnatremia at presentation among infants with acute gastroenteritis was 14%. Severe dehydration was associated with dysnatremia at presentation, so electrolyte levels need to be assessed in these patients. The use of isotonic solution did not promote acquired dysnatremia. This study supports once more that current guidelines recommending isotonic solution for children, and, especially, infant rehydration, are important also for infants in Thailand.
What is Known: • There were a wide variation in the incidence of dysnatremia at presentation in children with acute gastroenteritis in previous pediatric series. • The AAP guidelines recommend using isotonic solution in children with acute illness from 28 days to 18 years of age to prevent acquired hyponatremia. | |
What is New: • The incidence of dysnatremia at presentation in infants with acute gastroenteritis was 14% (hyponatremia 12% and hypernatremia 2.0%). • The use of isotonic solution did not promote acquired dysnatremia in infants with acute gastroenteritis. |
Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
Abbreviations
- AAP:
-
American Academy of Pediatrics
- ADH:
-
Antidiuretic hormone
- D5-NS:
-
5% Dextrose in saline
- D5-1/2NS:
-
5% Dextrose in 1/2 saline
- D5-1/3NS:
-
5% Dextrose in 1/3 saline
- D5-1/4NS:
-
5% Dextrose in 1/4 saline
- D5-1/5NS:
-
5% Dextrose in 1/5 saline
- IV:
-
Intravenous
- IQR:
-
Interquartile ranges
- ORs:
-
Odds ratios
- ORS:
-
Oral rehydration solutions
- SD:
-
Standard deviation
- SPSS:
-
PASW Statistics
References
Farthing M, Salam MA, Lindberg G et al (2013) Acute diarrhea in adults and children: a global perspective. J Clin Gastroenterol 47:12–20. https://doi.org/10.1097/MCG.0b013e31826df662
Charoenwat B, Suwannaying K, Paibool W, Laoaroon N, Sutra S, Thepsuthammarat K (2022) Burden and pattern of acute diarrhea in Thai children under 5 years of age: a 5-year descriptive analysis based on Thailand National Health Coverage (NHC) data. BMC Public Health 22:1161. https://doi.org/10.1186/s12889-022-13598-8
Granado-Villar D, Cunill-De Sautu B and Granados A (2012) Acute gastroenteritis. Pediatr Rev 33:487–494 quiz 495. https://doi.org/10.1542/pir.33-11-487
Gattineni J, Baum M (2015) Developmental changes in renal tubular transport-an overview. Pediatr Nephrol 30:2085–2098. https://doi.org/10.1007/s00467-013-2666-6
Neville KA, Verge CF, O’Meara MW, Walker JL (2005) High antidiuretic hormone levels and hyponatremia in children with gastroenteritis. Pediatrics 116:1401–1407. https://doi.org/10.1542/peds.2004-2376
Neville KA, Verge CF, Rosenberg AR, O’Meara MW, Walker JL (2006) Isotonic is better than hypotonic saline for intravenous rehydration of children with gastroenteritis: a prospective randomised study. Arch Dis Child 91:226–232. https://doi.org/10.1136/adc.2005.084103
Hayajneh WA, Jdaitawi H, Al Shurman A, Hayajneh YA (2010) Comparison of clinical associations and laboratory abnormalities in children with moderate and severe dehydration. J Pediatr Gastroenterol Nutr 50:290–294. https://doi.org/10.1097/MPG.0b013e31819de85d
Hanna M, Saberi MS (2010) Incidence of hyponatremia in children with gastroenteritis treated with hypotonic intravenous fluids. Pediatr Nephrol 25:1471–1475. https://doi.org/10.1007/s00467-009-1428-y
Freedman SB, Geary DF (2013) Bolus fluid therapy and sodium homeostasis in paediatric gastroenteritis. J Paediatr Child Health 49:215–222. https://doi.org/10.1111/jpc.12120
Shahrin L, Chisti MJ, Huq S, Nishath T, Christy MD, Hannan A, Ahmed T (2016) Clinical manifestations of hyponatremia and hypernatremia in under-five diarrheal children in a diarrhea hospital. J Trop Pediatr 62:206–212. https://doi.org/10.1093/tropej/fmv100
Qadori M, Flem E, Bekkevold T, Døllner H, Gilje AM, Rojahn A, Størdal K (2018) Hypoglycaemia was common in acute gastroenteritis in a prospective hospital-based study, but electrolyte imbalances were not. Acta Paediatr 107:1455–1460. https://doi.org/10.1111/apa.14318
Dastidar R and Konar N (2017) A study of electrolyte disturbances in a child presenting with acute gastroenteritis, with special emphasis on hyponatremic dehydration-a hospital based cross-sectional study. Pediatr Ther 07. https://doi.org/10.4172/2161-0665.1000322
Finberg L (1986) Too little water has become too much. The changing epidemiology of water balance and convulsions in infant diarrhea. Am J Dis Child 140:524. https://doi.org/10.1001/archpedi.1986.02140200034019
Mazzoni MB, Milani GP, Bernardi S et al (2019) Hyponatremia in infants with community-acquired infections on hospital admission. PLoS One 14:e0219299. https://doi.org/10.1371/journal.pone.0219299
Holliday MA, Segar WE (1957) The maintenance need for water in parenteral fluid therapy. Pediatrics 19:823–832
Feld LG, Neuspiel DR, Foster BA et al (2018) Clinical practice guideline: maintenance intravenous fluids in children. J Pediatr 142:e20183083. https://doi.org/10.1542/peds.2018-3083
Santi M, Lava SA, Camozzi P, Giannini O, Milani GP, Simonetti GD, Fossali EF, Bianchetti MG, Faré PB (2015) The great fluid debate: saline or so-called “balanced” salt solutions? Ital J Pediatr 41:47. https://doi.org/10.1186/s13052-015-0154-2
Steiner MJ, DeWalt DA, Byerley JS (2004) Is this child dehydrated? JAMA 291:2746–2754. https://doi.org/10.1001/jama.291.22.2746
Guarino A, Ashkenazi S, Gendrel D, Lo Vecchio A, Shamir R, Szajewska H (2014) European Society for Pediatric Gastroenterology, Hepatology, and Nutrition/European Society for Pediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe: update 2014. J Pediatr Gastroenterol Nutr 59:132–152. https://doi.org/10.1097/mpg.0000000000000375
Forman S, Crofton P, Huang H, Marshall T, Fares K, McIntosh N (2012) The epidemiology of hypernatraemia in hospitalised children in Lothian: a 10-year study showing differences between dehydration, osmoregulatory dysfunction and salt poisoning. Arch Dis Child 97:502–507. https://doi.org/10.1136/archdischild-2011-300305
Hasegawa H, Okubo S, Ikezumi Y, Uchiyama K, Hirokawa T, Hirano H, Uchiyama M (2009) Hyponatremia due to an excess of arginine vasopressin is common in children with febrile disease. Pediatr Nephrol 24:507–511. https://doi.org/10.1007/s00467-008-1053-1
Bichet DG (2019) Regulation of thirst and vasopressin release. Annu Rev Physiol 81:359–373. https://doi.org/10.1146/annurev-physiol-020518-114556
Vantyghem MC, Balavoine AS, Wémeau JL, Douillard C (2011) Hyponatremia and antidiuresis syndrome Ann Endocrinol (Paris) 72:500–512. https://doi.org/10.1016/j.ando.2011.10.001
Kaiser P, Borte M, Zimmer KP, Huppertz HI (2012) Complications in hospitalized children with acute gastroenteritis caused by rotavirus: a retrospective analysis. Eur J Pediatr 171:337–345. https://doi.org/10.1007/s00431-011-1536-0
Elliott EJ (2007) Acute gastroenteritis in children Bmj 334:35–40. https://doi.org/10.1136/bmj.39036.406169.80
Corsello A, Malandrini S, Bianchetti MG, Agostoni C, Cantoni B, Meani F, Faré PB, Milani GP (2022) Sodium assessment in neonates, infants, and children: a systematic review. Eur J Pediatr 181:3413–3419. https://doi.org/10.1007/s00431-022-04543-3
Lava SA, Bianchetti MG, Milani GP (2017) Testing Na(+) in blood. Clin Kidney J 10:147–148. https://doi.org/10.1093/ckj/sfw103
Malandrini S, Lava SAG, Bianchetti MG, Meani F, Faré PB, Camozzi P, Cugliari M, Agostoni C, Milani GP (2021) Which laboratory technique is used for the blood sodium analysis in clinical research? A systematic review. Clin Chem Lab Med 59:1501–1506. https://doi.org/10.1515/cclm-2021-0293
Author information
Authors and Affiliations
Contributions
T.C. designed the study and contributed to the methodology. W.S. collected the data. K.S. performed the analysis. W.S. and T.C. wrote the manuscript. W.S., K.S., A.S., A.P., S.S., N.P., K.L., Y.T., and T.C. contributed to the interpretation of data, participated in critical revision of the manuscript for important intellectual content, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. This protocol was approved by the Siriraj Hospital Ethics Board (Si 442/2021).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Gregorio Milani
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sakkongviseth, W., Sommai, K., Sumboonnanonda, A. et al. Dysnatremia and subsequent sodium level changes following various intravenous treatments in infants with acute gastroenteritis. Eur J Pediatr 182, 4741–4748 (2023). https://doi.org/10.1007/s00431-023-05151-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05151-5