Abstract
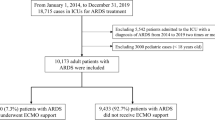
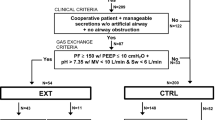
The main objective of this study was to describe the current mechanical ventilation (MV) settings during extracorporeal membrane oxygenation (ECMO) for pediatric acute respiratory distress syndrome (P-ARDS) in six European centers. This is a retrospective observational cohort study performed in six European centers from January 2009 to December 2019. Children > 1 month to 18 years supported with ECMO for refractory P-ARDS were included. Collected data were as follows: patients’ pre-ECMO medical condition, pre-ECMO adjunctive therapies for P-ARDS, pre-ECMO and during ECMO MV settings on day (D) 1, D3, D7, and D14 of ECMO, use of adjunctive therapies during ECMO, duration of ECMO, pediatric intensive care unit length of stay, and survival. A total of 255 patients with P-ARDS were included. The multivariate analysis showed that PEEP on D1 (OR = 1.13, 95% CI [1.03–1.24], p = 0.01); D3 (OR = 1.17, 95% CI [1.06–1.29], p = 0.001); and D14 (OR = 1.21, 95% CI [1.05–1.43], p = 0.02) and DP on D7 were significantly associated with higher odds of mortality (OR = 0.82, 95% CI [0.71–0.92], p = 0.001). Moreover, DP on D1 above 15 cmH2O (OR 2.23, 95% CI (1.09–4.71), p = 0.03) and native lung FiO2 above 60% on D14 (OR 10.36, 95% CI (1.51–116.15), p = 0.03) were significantly associated with higher odds of mortality.
Conclusion: MV settings during ECMO for P-ARDS varied among centers; however, use of high PEEP levels during ECMO was associated with higher odds of mortality as well as a DP above 15 cmH2O and a native lung FiO2 above 60% on D14 of ECMO.
What is Known: • Invasive ventilation settings are well defined for pediatric acute respiratory distress syndrome; however, once the children required an extracorporeal respiratory support, there is no recommendation how to set the mechanical ventilator. • Impact of invasive ventilator during extracorporeal respiratory support ad only been during the first days of this support but the effects of these settings later in the assistance are not described. | |
What is New: • It seems to be essential to early decrease FiO2 on native lung once the ECMO flow allows an efficient oxygenation. • Tight control to limit the driving pressure at 15 cmH20 during ECMO run seems to be associated with better survival rate. |




Similar content being viewed by others
Data availability
All data are available on demand.
Abbreviations
- CI:
-
Confidence intervals
- DP:
-
Driving pressure
- ECMO:
-
Extracorporeal membrane oxygenation
- ELSO:
-
Extracorporeal Life Support Organization
- MAP:
-
Mean airways pressure
- MV:
-
Mechanical ventilation
- NMB:
-
Neuromuscular blockers
- OR:
-
Odds ratio
- PALICC:
-
Pediatric Acute Lung Injury Consensus Conference
- P-ARDS:
-
Pediatric acute respiratory distress syndrome
- PEEP:
-
Positive end expiratory pressure
- PELOD:
-
Pediatric Logistic Organ Dysfunction score
- PICU:
-
Pediatric intensive care unit
- PIM II:
-
Pediatric Index of Mortality 2 score
- Ppeak:
-
Peak airway pressure
- VFD-28:
-
Ventilator-free days at 28 days
- Vt:
-
Tidal volume
- VV:
-
Veno-venous
References
Khemani RG, Smith L, Lopez-Fernandez YM, Kwok J, Morzov R, Klein MJ et al (2018) Paediatric acute respiratory distress syndrome incidence and epidemiology (PARDIE): an international, observational study. Lancet Respir Med 7:115–128
Beltramo F, Khemani RG (2019) Definition and global epidemiology of pediatric acute respiratory distress syndrome. Ann Transl Med 7:502
Kollisch-Singule M, Ramcharran H, Satalin J, Blair S, Gatto LA, Andrews PL et al (2021) Mechanical ventilation in pediatric and neonatal patients. Front Physiol 12:805620
Emeriaud G, López-Fernández YM, Iyer NP, Bembea MM, Agulnik A, Barbaro RP et al (2023) Executive summary of the second International Guidelines for the Diagnosis and Management of Pediatric Acute Respiratory Distress Syndrome (PALICC-2). Pediatr Crit Care Med 24:143–168
Grasso S, Stripoli T, Mazzone P, Pezzuto M, Lacitignola L, Centonze P et al (2014) Low respiratory rate plus minimally invasive extracorporeal Co2 removal decreases systemic and pulmonary inflammatory mediators in experimental acute respiratory distress syndrome. Crit Care Med 42:e451-460
Maratta C, Potera RM, van Leeuwen G, Castillo Moya A, Raman L, Annich GM et al (2020) Extracorporeal Life Support Organization (ELSO): 2020 Pediatric Respiratory ELSO Guideline. ASAIO J 66:975–979
Rozencwajg S, Guihot A, Franchineau G, Lescroat M, Bréchot N, Hékimian G et al (2019) Ultra-protective ventilation reduces biotrauma in patients on venovenous extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. Crit Care Med 47:1505–1512
Schmidt M, Stewart C, Bailey M, Nieszkowska A, Kelly J, Murphy L et al (2015) Mechanical ventilation management during extracorporeal membrane oxygenation for acute respiratory distress syndrome: a retrospective international multicenter study. Crit Care Med 43:654–664
Schmidt M, Pham T, Arcadipane A, Agerstrand C, Ohshimo S, Pellegrino V et al (2019) Mechanical ventilation management during ECMO for ARDS: an international multicenter prospective cohort. Am J Respir Crit Care Med 200:1002–1012
Guervilly C, Fournier T, Chommeloux J, Arnaud L, Pinglis C, Baumstarck K et al (2022) Ultra-lung-protective ventilation and biotrauma in severe ARDS patients on veno-venous extracorporeal membrane oxygenation: a randomized controlled study. Crit Care 26:383
Friedman ML, Barbaro RP, Bembea MM, Bridges BC, Chima RS, Kilbaugh TJ et al (2020) Mechanical ventilation in children on venovenous ECMO. Respir Care 65:271–280
Friedman ML, Abu-Sultaneh S, Slaven JE, Mastropietro CW et al (2022) Rest ventilator management in children on veno-venous extracorporeal membrane oxygenation. Int J Artif Organs 45:174–180
Blauvelt DG, Inany HS, Furlong-Dillard JM, Bailly DK, Oishi P, Steurer MA et al (2022) Association of ventilator settings with mortality in pediatric patients treated with extracorporeal life support for respiratory failure. ASAIO J 68:1536–1543
Miya TR, Furlong-Dillard JM, Sizemore JM, Meert KL, Dalton HJ, Reeder RW et al (2023) Association between mortality and ventilator parameters in children with respiratory failure on ECMO. Respir Care 68:592–601
Di Nardo M, De Piero ME, Hoskote A, Belohlavek J, Lorusso R et al (2022) EuroECMO neonatal and paediatric COVID-19 Working Group and EuroELSO Steering Committee Extracorporeal membrane oxygenation in children with COVID-19 and PIMS-TS during the second and third wave. Lancet Child Adolesc Health 6:e14–e15
Schmidt M, Combes A, Shekar K et al (2019) ECMO for immunosuppressed patients with acute respiratory distress syndrome: drawing a line in the sand. Intensive Care Med 45:1140–1142
Barbaro RP, Boonstra PS, Paden ML, Roberts LA, Annich GM, Bartlett RH et al (2016) Development and validation of the pediatric risk estimate score for children using extracorporeal respiratory support (Ped-RESCUERS). Intensive Care Med 42:879–888
Slater A, Shann F, Pearson G et al (2003) Paediatric Index of Mortality (PIM) Study Group. PIM2: a revised version of the Paediatric Index of Mortality Intensive Care Med 29:278‑285
Leteurtre S, Martinot A, Duhamel A, Proulx F, Grandbastien B, Cotting J et al (2003) Validation of the paediatric logistic organ dysfunction (PELOD) score: prospective, observational, multicentre study. Lancet 362:192–197
DesPrez K, McNeil JB, Wang C, Bastarache JA, Shaver CM, Ware LB et al (2017) Oxygenation saturation index predicts clinical outcomes in ARDS. Chest 152:1151–1158
Amato MBP, Meade MO, Slutsky AS, Brochard L, Costa ELV, Schoenfeld DA et al (2015) Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 372:747–755
van Buuren S, Groothuis-Oudshoorn K (2011) Mice: multivariate imputation by chained equations in R. J Stat Softw 1–67
Wood AM, White IR, Royston P et al (2008) How should variable selection be performed with multiply imputed data? Stat Med 27:3227–3246
Heinze G, Wallisch C, Dunkler D et al (2018) Variable selection - a review and recommendations for the practicing statistician. Biom J 60:431–449
Heymans M (2021) PSFMI: Prediction model selection and performance evaluation in multiple imputed datasets. R Package Version 1.0.0
Wong JJM, Liu S, Dang H, Anantasit N, Phan PH, Phumeetham S et al (2020) The impact of high frequency oscillatory ventilation on mortality in paediatric acute respiratory distress syndrome. Crit Care 24:31
Dowell JC, Thomas NJ, Yehya N et al (2017) Association of response to inhaled nitric oxide and duration of mechanical ventilation in pediatric acute respiratory distress syndrome. Pediatr Crit Care Med 18:1019–1026
van Schelven P, Koopman AA, Burgerhof JGM, Markhorst DG, Blokpoel RGT, Kneyber MCJ et al (2005) Driving pressure is associated with outcome in pediatric acute respiratory failure. Pediatr Crit Care Med 23:e136-144
Curley MAQ, Hibberd PL, Fineman LD, Wypij D, Shih MC, Thompson JE et al (2005) Effect of prone positioning on clinical outcomes in children with acute lung injury: a randomized controlled trial. JAMA 294:229–237
Curley MA, Thompson JE, Arnold JH et al (2000) The effects of early and repeated prone positioning in pediatric patients with acute lung injury. Chest 118:156–163
Rudolph MW, Kneyber MCJ, Asaro LA, Cheifetz IM, Wypij D, Curley MAQ et al (2022) Early neuromuscular blockade in moderate-to-severe pediatric acute respiratory distress syndrome. Crit Care Med 50:e445–e457
Jegard J, Levy Y, Guellec I, Guilbert J, Soreze Y, Piloquet JE et al (2022) Usefulness of implementation of a protective mechanical ventilation bundle during extracorporeal membrane oxygenation for pediatric acute respiratory distress syndrome. Minerva Pediatr. https://doi.org/10.23736/S2724-5276.22.06391-1
Araos J, Alegria L, Garcia P, Cruces P, Soto D, Erranz B et al (2019) Near-apneic ventilation decreases lung injury and fibroproliferation in an acute respiratory distress syndrome model with extracorporeal membrane oxygenation. Am J Respir Crit Care Med 199:603–612
Graf PT, Boesing C, Brumm I, Biehler J, Müller KW, Thiel M et al (2022) Ultra protective versus apneic ventilation in acute respiratory distress syndrome patients with extracorporeal membrane oxygenation: a physiological study. J Intensive Care 10:12
Author information
Authors and Affiliations
Contributions
JR and MD defined the project and write the main manuscript FV, PLL, LB, JEP collected data and help preparing all the table SC et YG performed the statistics All authors review the manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional) and with the Helsinki Declaration of 1975.
Conflict of interest
Dr. Matteo Di Nardo is an Advisory Board Member of Eurosets (Eurosets srl: Medolla, Modena, Italy). Dr. Broman is an Advisory Board Member of Eurosets (Eurosets srl: Medolla, Modena, Italy) and Xenios AG, Heilbronn, Germany. All other authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rambaud, J., Broman, L.M., Chevret, S. et al. Association between pediatric intensive care mortality and mechanical ventilation settings during extracorporeal membrane oxygenation for pediatric acute respiratory distress syndrome. Eur J Pediatr 182, 4487–4497 (2023). https://doi.org/10.1007/s00431-023-05119-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05119-5