Abstract
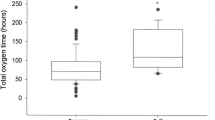
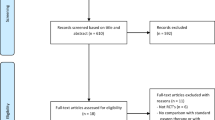
To study association of enteral feeds in bronchiolitis patients supported by different levels of high flow nasal cannula (HFNC) with adverse events, nutritional goals, and clinical outcomes. Bronchiolitis patients ≤ 24 months of age treated with < 1 L/kg/min, 1–2 L/kg/min and > 2 L/kg/min of HFNC between January 2014 and December 2021 were studied retrospectively at a tertiary care children’s hospital. Adverse events (aspiration pneumonia, emesis, and respiratory support escalation), nutritional goals (initiation of enteral feeds, achievement of nutritional goal volume and goal calories, percentage weight change during hospital stay) and clinical outcomes (HFNC duration, oxygen supplementation duration after HFNC, length of hospital stay following HFNC support, total length of hospital stay and follow-up for 1 month after hospital discharge) were compared between fed and non-fed patients on HFNC. Six hundred thirty-six (489 fed and 147 not-fed) bronchiolitis patients on HFNC studied. 260 patients, 317 patients and 59 patients were supported by < 1 L/kg/min, 1–2 L/kg/min and > 2 L/kg/min of HFNC, respectively. Enterally fed patients had significantly less adverse events (OR = 0.14, 95% CI 0.083 – 0.23, p < 0.001), significantly better nutritional goals: earlier initiation of enteral feeds by 65% in time (mean ratio = 0.35, 95% CI 0.28 – 0.43, p < 0.001), earlier achievement of goal volume and goal calorie needs by 14% in time (mean ratio = 0.86, 95% CI 0.78 to 0.96, p = 0.005) and significantly better clinical outcomes: shorter HFNC duration by 29.75 h (95% CI 20.19 -39.31, p < 0.001), shorter oxygen supplementation duration after HFNC by 12.14 h (95% CI 6.70 -17.59, p < 0.001), shorter length of hospital stay after HFNC support by 21.35 h (95% CI 14.71–27.98, p < 0.001) and shorter total length of hospital stay by 51.10 h (95% CI 38.65 -63.55, p < 0.001), as compared to non-fed patients, after adjusting for age, weight, prematurity, comorbidities, admission time, admission bronchiolitis score, admission respiratory rate, and HFNC levels. The number of revisits and readmissions at 7 and 30 days after hospital discharge were not significantly different (p > 0.05) between the fed and non-fed groups.
Conclusion: Enteral feeding of bronchiolitis patients supported by different levels of HFNC is associated with less adverse events and better nutrition goals and clinical outcomes.
What is Known: •There is general apprehension to feed critically ill bronchiolitis patients supported by high flow nasal cannula. | |
What is New: •Our study reveals that enteral feeding of critically ill bronchiolitis patients supported by different levels of high flow nasal cannula is associated with minimal adverse events, better nutritional goals and improved clinical outcomes as compared to non-fed patients. |


Similar content being viewed by others
Data availability
Data availability will be provided at request to the corresponding author.
Abbreviations
- BiPAP:
-
Bilevel positive airway pressure support
- CPAP:
-
Continuous positive airway pressure support
- HFNC:
-
High Flow Nasal Cannula
- IQR:
-
Interquartile range
- PICU:
-
Pediatric Intensive Care Unit
- RSE:
-
Respiratory support escalation
References
Ralston SL, Lieberthal AS, Meissner HC et al (2014) American Academy of Pediatrics: Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics 134:e1474–e1502. https://doi.org/10.1542/peds.2014-2742
Gupta P, Beam BW, Rettiganti M (2016) Temporal trends of respiratory syncytial virus–associated hospital and ICU admissions across the United States. Pediatr Crit Care Med 17:e343–e351. https://doi.org/10.1097/PCC.0000000000000850
Pelletier JH, Au AK, Fuhrman D, Clark RSB, Hovat C (2021) Trends in bronchiolitis ICU admissions and ventilation practices: 2010–2019. Pediatrics 147:e2020039115. https://doi.org/10.1542/peds.2020-039115
Mecklin M, Heikkila P, Korppi M (2018) The change in management of bronchiolitis in the intensive care unit between 2000 and 2015. Eur J Pediatr 177:1131–1137. https://doi.org/10.1007/s00431-018-3156-4
O’Brien S, Borland ML, Cotterell E et al (2019) Australasian bronchiolitis guideline. J Paediatr Child Health 55:42–53. https://doi.org/10.1111/jpc.14104
Milesi C, Baudin F, Durand P et al (2023) Clinical practice guidelines: management of severe bronchiolitis in infants under 12 months old admitted to a pediatric critical care unit. Intensive Care Med 49:5–25. https://doi.org/10.1007/s00134-022-06918-4
Valla FV, Baudin F, Demaret P et al (2019) Nutritional management of young infants presenting with acute bronchiolitis in Belgium, France, and Switzerland: survey of current practices and documentary search of national guidelines worldwide. Eur J Pediatr 178:331–340. https://doi.org/10.1007/s00431-018-3300-1
Walter S, DeLeon S, Walther JP, Sifers F, Garbe MC, Allen C (2022) The nutritional impact of a feeding protocol for infants on high flow nasal cannula therapy. Nutr Clin Pract 37:935–944. https://doi.org/10.1002/ncp.10817
Shadman KA, Kelly MM, Edmonson MB, Sklansky DJ, Nackers K, Allen A, Barreda CB, Thurber AS, Coller RJ (2019) Feeding during high-flow nasal cannula for bronchiolitis: associations with time to discharge. J Hosp Med 14:E43‐E48. https://doi.org/10.12788/jhm.3306
Sochet AA, McGee JA, October TW (2017) Oral nutrition in children with bronchiolitis on high-flow nasal cannula is well tolerated. Hosp Pediatr 7:249–255. https://doi.org/10.1542/hpeds.2016-0131
Slain KN, Martinez-Schlurmann N, Shein SL, Stormorken A (2017) Nutrition and high-flow nasal cannula respiratory support in children with bronchiolitis. Hosp Pediatr 7:256–262. https://doi.org/10.1542/hpeds.2016-0194
Courtney A, Bernard A, Burgess S, Davies K, Foster K, Kapor V, Levitt D, Sly PD (2022) Bolus versus continuous nasogastric feeds for infants with bronchiolitis: a randomized trial. Hosp Pediatrics 12:1–10. https://doi.org/10.1542/hpeds.2020-005702
Conway TP, Halaby C, Akerman M, Asuncion A (2021) The use of high-flow nasal cannula and the timing of safe feeding in children with bronchiolitis. Cureus 13:e15665. https://doi.org/10.7759/cureus.15665
Dadlez NM, Esteban-Cruciani N, Khan A, Shi Y, McKenna KJ, Azzarone G, Southern WN (2019) Safety of high-flow nasal cannula outside the ICU for previously healthy children with bronchiolitis. Respir Care 64:1410–1415. https://doi.org/10.4187/respcare.06352
Yurtseven A, Turan C, Erseven E, Saz EU (2019) Comparison of heated humidified high-flow nasal cannula flow rates (1-L/kg/min vs 2-L/kg/min) in the management of acute bronchiolitis. Pediatr Pulmonol 54:894–900. https://doi.org/10.1002/ppul.24318
Schofield WN (1985) Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr 39:5–41. PMID: 4044297
WHO. World Health Organization (1985) Energy and protein requirements, Report of a joint FAO/WHO/UNU expert consultation. World Health Organ Tech Rep Ser 724:1–206. PMID: 3937340
Sala KA, Moore A, Desai S, Welch K, Bhandari S, Carroll CL (2015) Factors associated with disease severity in children with bronchiolitis. J Asthma 52:268–272. https://doi.org/10.3109/02770903.2014.956893
Duarte-Dorado DM, Madero-Orostegui DS, Rodriguez-Martinez CE, Nino G (2013) Validation of a scale to assess the severity of bronchiolitis in a population of hospitalized infants. J Asthma 50:1056–1106. https://doi.org/10.3109/02770903.2013.834504
Ng GYH, Ong C, Wong JJM, Teoh OH, Sultana R, Mok YH, Lee JH (2020) Nutritional status, intake and outcomes in critically ill children with bronchiolitis. Pediatr Pulmonol 55:1199–1206. https://doi.org/10.1002/ppul.24701
Kalburgi S. Halley T (2020) High-flow nasal cannula outside of the ICU setting. Pediatrics 146:e20190483. https://doi.org/10.1542/peds.2019-4083
Tume LN, Eveleens RD, Mayordomo-Colunga J, Lopez J, Verbruggen SCAT, Fricaudet M, Smith C, Cusco MCC, Latten L, Valla FV (2021) Enteral feeding of children on noninvasive respiratory support: A four-center European study. Pediatr Crit Care Med 22:e192–e202. https://doi.org/10.1097/PCC.0000000000002602
Maloney JP, Ryan TA (2002) Detection of aspiration in enterally fed patients: a requiem for bedside monitors of aspiration. JPEN J Parenter Enteral Nutr 26:S34–S41. https://doi.org/10.1177/014860710202600606
Velayutham P, Irace AL, Kawai K, Dodrill P, Perez J, Londahl M, Mundy L, Dombrowski ND, Rahbar R (2018) Silent aspiration: Who is at risk? Laryngoscope 128:1952–1957. https://doi.org/10.1002/lary.27070
Franklin D, Babl FE, Schlapbach LJ et al (2018) A randomized trial of high-flow oxygen therapy in infants with bronchiolitis. N Engl J Med 378:1121–1131. https://doi.org/10.1056/NEJMoa1714855
Kepreotes E, Whitehead B, Attia J, Oldmeadow C, Collison A, Searles A, Goddard B, Hilton J, Lee M, Mattes J (2017) High-flow warm humidified oxygen versus standard low-flow nasal cannula oxygen for moderate bronchiolitis (HFWHO RCT): an open, phase 4, randomized controlled trial. Lancet 389:930–939. https://doi.org/10.1016/S0140-6736(17)30061-2
Leboucher J, Milesi C, Fumagalli A, Wroblewski I, Debillon T, Mortamet G (2022) Prevalence and risk factors of discomfort in infants with severe bronchiolitis. Acta Paediatr 111:1238–1244. https://doi.org/10.1111/apa.16305
Sochet AA, Nunez M, Wilsey MJ, Morrison JM, Bessone SK, Nakagawa TA (2021) Enteral nutrition improves vital signs in children with bronchiolitis on noninvasive ventilation. Hosp Pediatr 11:135–143. https://doi.org/10.1542/hpeds.2020-001180
Lenihan A, Ramos V, Nemec N, Lukowski J, Lee J, Kendall KM, Mahapatra S (2021) A retrospective analysis of feeding practices and complications in patients with critical bronchiolitis on non-invasive respiratory support. Children (Basel) 8:410. https://doi.org/10.3390/children8050410
Oakley E, Borland M, Neutze J et al (2013) Nasogastric hydration versus intravenous hydration for infants with bronchiolitis: a randomized trial. Lancet Respir Med 1:113–120. https://doi.org/10.1016/S2213-600(12)70053-X
Stocks J (1980) Effect of nasogastric tubes on nasal resistance during infancy. Arch Dis Child 55:17–21. https://doi.org/10.1136/adc.55.1.17
Srinivasan V, Hasbani NR, Mehta NM et al (2020) Early enteral nutrition is associated with improved clinical outcomes in critically ill children: a secondary analysis of nutrition support in the heart and lung failure-pediatric insulin titration trial. Pediatr Crit Care Med 21:213–221. https://doi.org/10.1097/PCC.0000000000002135
Hubert A, Ford-Chessel C, Berthiller J, Peretti N, Javouhey E, Valla FV (2016) Nutritional status in pediatric intermediate care: assessment at admission, progression during the stay and after discharge. Arch Pediatr 23:333–339. https://doi.org/10.1016/j.arcped.2015.12.014
Soshnick SH, Mark GS, Weingarten-Arams J, Chuu Y, Chandhoke S, Medar SS, Philips K, Cassel-Choudhry GN (2022) Feeding pathway for children on high flow nasal cannula decreases time to enteral nutrition. Pediatr Qual Saf 7:e608. https://doi.org/10.1097/pq9.0000000000000608
Halvorson EE, Chandler N, Neiberg R, Ervin SE (2013) Association of NPO status and type of nutritional support on weight and length of stay in infants hospitalized with bronchiolitis. Hosp Pediatr 3:366–370. https://doi.org/10.1542/hpeds.2013-0011
De Cosmi V, Mehta NM, Boccazzi A, Milani GP, Esposito S, Bedogni G, Agostoni C (2017) Nutritional status, metabolic state and nutrient intake in children with bronchiolitis. Int J Food Sci Nutr 68:378–383. https://doi.org/10.1080/09637486.2016.1245714
Weisgerber MC, Lye PS, Nugent M, Li SH, Fouw KD, Gedeit R, Simpson P, Gorelick MH (2013) Relationship between caloric intake and length of hospital stay for infants with bronchiolitis. Hosp Pediatr 3:24–30. https://doi.org/10.1542/hpeds.2012-0032
Kugelman A, Raibin K, Dabbah H, Chistyakov I, Srugo I, Even L, Bzezinsky N, Riskin A (2013) Intravenous fluids versus gastric tube feeding in hospitalized infants with viral bronchiolitis: a randomized, prospective pilot study. J Pediatr 162:640–642. https://doi.org/10.1016/j.jpeds.2012.10.057
Oakley E, Bata S, Rengasamy S, Kriser D, Cheek J, Jachno K, Babl FE (2016) Nasogastric hydration in infants with bronchiolitis less than 2 months of age. J Pediatr 178:241–245. https://doi.org/10.1016/j.jpeds.2016.07.012
Mehta NM, Skillman HE, Irving SY, Coss-Bu JA, Vermilyea S, Farrington EA, McKeever L, Hall AM, Goday PS, Braunschweig C (2017) Guidelines for the provision and assessment of nutrition support therapy in the pediatric critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition. JPEN J Parenter Enteral Nutr 41:706–742. https://doi.org/10.1177/0148607117711387
Tume LN, Valla FV, Joosten K et al (2020) Nutritional support for children during critical illness: European Society of Pediatric and Neonatal Intensive Care (ESPNIC) metabolism, endocrine and nutrition section position statement and clinical recommendations. Intensive Care Med 46:411–425. https://doi.org/10.1007/s00134-019-05922-5
Canarie MF, Barry S, Carroll CL, Hassinger A, Kandil S, Li S, Pinto M, Valentine SL, Faustino EVS, Northeast Pediatric Critical Care Research Consortium (2015) Risk factors for delayed enteral nutrition in critically ill children. Pediatr Crit Care Med 16:e283–e289. https://doi.org/10.1097/PCC.0000000000000527
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Reem Sarkis, Wei Liu, and Hemant Agarwal. The first draft of the manuscript was written by Reem Sarkis, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of The Cleveland Clinic Foundation (CCF) Institutional Review Board (IRB) (Date 3/17/2022 /No # 21-303).
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sarkis, R., Liu, W., DeTallo, C. et al. Association of enteral feeds in critically ill bronchiolitis patients supported by high-flow nasal cannula with adverse events and outcomes. Eur J Pediatr 182, 4015–4025 (2023). https://doi.org/10.1007/s00431-023-05085-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05085-y