Abstract
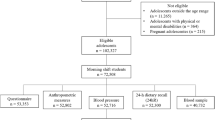
To investigate the influence of ultra-processed food (UPF) consumption on systolic (SBP) and diastolic (DBP) blood pressure in children with obesity, using dietary and urinary markers. We conducted a secondary analysis of a randomized clinical trial involving children with obesity, aged 7 to 12 years. Over a period of six months, the children and their guardians attended monthly individual consultations and educational activities aimed at promoting a reduction in UPF consumption. During each visit, measurements of blood pressure, body weight, height, and 24-h dietary recall were recorded. Additionally, spot urine samples were collected at baseline, and at the second and fifth-month follow-ups. A total of 96 children were included in the analysis. Energy intake, UPF intake and blood pressure showed a quadratic pattern of change, with a decrease in the first two months and an increase thereafter. There was an association between UPF consumption and DBP. The intake of UPF was correlated with the urinary sodium-to-potassium (Na/K) ratio (r = 0.29; p = 0.008) and the dietary Na/K ratio (r = 0.40; p < 0.001). For every 100 g increase in UPF, DBP increased by 0.28 mmHg (p-value = 0.01). After further adjustment for changes in body mass index (BMI), and physical activity, the increase in DBP was 0.22 mmHg.
Conclusion: Our findings indicate that reducing UPF consumption may have an impact on blood pressure in children with obesity. Additional adjustment for BMI and physical activity did not influence the results. Therefore, reducing UPF consumption can be considered as a strategy against hypertension.
What is Known: • Ultra-processed food consumption is associated with an increased risk of cardiovascular disease; however, this evidence is still limited in children. • Intake of calories from ultra-processed food in relation to the total calories is increasing worldwide. | |
What is New: • Ultra-processed food consumption has an effect on the diastolic blood pressure, independent of changes in weight. • The intake of ultra-processed food was correlated to the dietary sodium-to-potassium ratio (r = 0.40; p < 0.001). |

Similar content being viewed by others
Data availability
The data supporting the results of this study are available from the corresponding author upon reasonable request.
Abbreviations
- 24hDR:
-
24-hour dietary recall
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CVD:
-
Cardiovascular disease
- DBP:
-
Diastolic blood pressure
- IPAQ:
-
International physical activity questionnaire
- kcal:
-
Kilocalories
- kg:
-
Kilograms
- mEq/L:
-
Milliequivalents per liter
- mg:
-
Milligrams
- mmHg:
-
Millimeters of mercury
- Na/K:
-
Sodium-to-potassium
- SBP:
-
Systolic blood pressure
- UPF:
-
Ultra-processed food
- WHO:
-
World Health Organization
References
Juul F, Vaidean G, Lin Y et al (2021) Ultra-Processed Foods and Incident Cardiovascular Disease in the Framingham Offspring Study. J Am Coll Cardiol 77:1520–1531. https://doi.org/10.1016/j.jacc.2021.01.047
Srour B, Fezeu LK, Kesse-Guyot E et al (2019) Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé). BMJ 365:l1451. https://doi.org/10.1136/bmj.l1451
Micha R, Shulkin ML, Peñalvo JL et al (2017) Etiologic effects and optimal intakes of foods and nutrients for risk of cardiovascular diseases and diabetes: Systematic reviews and meta-analyses from the Nutrition and Chronic Diseases Expert Group (NutriCoDE). PLoS One 12:e0175149. https://doi.org/10.1371/journal.pone.0175149
Monteiro CA, Cannon G, Levy RB et al (2019) Ultra-processed foods: what they are and how to identify them. Public Health Nutr 22:936–941. https://doi.org/10.1017/S1368980018003762
de Oliveira Otto MC, Afshin A, Micha R et al (2016) The Impact of Dietary and Metabolic Risk Factors on Cardiovascular Diseases and Type 2 Diabetes Mortality in Brazil. PLoS One 11:e0151503. https://doi.org/10.1371/journal.pone.0151503
Instituto Brasileiro de Geografia e Estatística - IBGE (2020) Pesquisa nacional de saúde : 2019 : percepção do estado de saúde, estilos de vida, doenças crônicas e saúde bucal: Brasil e grandes regiões / IBGE, Coordenação de Trabalho e Rendimento - Rio de Janeiro: IBGE, 2020. 113p
Instituto Brasileiro de Geografia e Estatística, Diretoria de Pesquisa, Coordenação de Trabalho e Rendimento (2020) Pesquisa de orçamentos familiares 2017–2018: avaliação nutricional da disponibilidade domiciliar de alimentos no Brasil
Leffa PS, Hoffman DJ, Rauber F et al (2020) Longitudinal associations between ultra-processed foods and blood lipids in childhood. Br J Nutr 124:341–348. https://doi.org/10.1017/S0007114520001233
Rodrigues RM, de Souza AM, Bezerra IN et al (2021) Most consumed foods in Brazil: evolution between 2008–2009 and 2017–2018. Rev Saúde Pública 55. https://doi.org/10.11606/s1518-8787.2021055003406
Buckley JP, Kim H, Wong E, Rebholz CM (2019) Ultra-processed food consumption and exposure to phthalates and bisphenols in the US National Health and Nutrition Examination Survey, 2013–2014. Environ Int 131:105057. https://doi.org/10.1016/j.envint.2019.105057
da Lopes AE, SC, Araújo LF, Levy RB et al (2019) Association between consumption of ultra-processed foods and serum C-reactive protein levels: cross-sectional results from the ELSA-Brasil study. Sao Paulo Med J 137:169–176. https://doi.org/10.1590/1516-3180.2018.0363070219
de Mendonça R, D, Lopes ACS, Pimenta AM et al (2017) Ultra-Processed Food Consumption and the Incidence of Hypertension in a Mediterranean Cohort: The Seguimiento Universidad de Navarra Project. Am J Hypertens 30:358–366. https://doi.org/10.1093/ajh/hpw137
Brandao JM, Sichieri R, Ribas SA et al (2020) Treatment of Childhood Obesity Based on Brazilian Dietary Guidelines Plus Energy Restriction (PAPPAS HUPE Study): Protocol for a Randomized Clinical Trial. JMIR Res Protoc 9:e16170. https://doi.org/10.2196/16170
Monteiro CA, Cannon G, Moubarac J-C et al (2015) Dietary guidelines to nourish humanity and the planet in the twenty-first century. A blueprint from Brazil. Public Health Nutr 18:2311–2322. https://doi.org/10.1017/S1368980015002165
Christofaro DGD, Fernandes RA, Gerage AM et al (2009) Validação do monitor de medida de pressão arterial Omron HEM 742 em adolescentes. Arq Bras Cardiol 92:10–15. https://doi.org/10.1590/S0066-782X2009000100003
Pickering TG, Hall JE, Appel LJ et al (2005) Recommendations for Blood Pressure Measurement in Humans and Experimental Animals. Circulation 111:697–716. https://doi.org/10.1161/01.CIR.0000154900.76284.F6
Flynn JT, Falkner BE (2017) New Clinical Practice Guideline for the Management of High Blood Pressure in Children and Adolescents. Hypertension 70:683–686. https://doi.org/10.1161/HYPERTENSIONAHA.117.10050
Barufaldi LA, de Abreu G, A, Veiga GV da et al (2016) Software to record 24-hour food recall: application in the Study of Cardiovascular Risks in Adolescents. Rev bras epidemiol 19:464–468. https://doi.org/10.1590/1980-5497201600020020
Food Research Center (FoRC) (2022) Tabela Brasileira de Composição de Alimentos (TBCA). Universidade de São Paulo (USP). Versão 7.2. São Paulo
Mill JG, Rodrigues SL, Baldo MP et al (2015) Validation study of the Tanaka and Kawasaki equations to estimate the daily sodium excretion by a spot urine sample. Rev Bras Epidemiol 18:224–237. https://doi.org/10.1590/1980-5497201500060020
Gordon C, Chumlea W, Roche A (1988) Stature, recumbent length and weight. In: Lohman TG, Roche AF, Martorel R (eds) Anthropometric Standardization Reference Manual, 1st edn. Human Kinetics Books, Champaign, pp 3–8
de Onis M, Onyango AW, Borghi E et al (2007) Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 85:660–667. https://doi.org/10.2471/BLT.07.043497
Matsudo S, Araújo T, Matsudo V et al (2001) Questionário Internacional de Atividade Física (IPAQ): Estudo de Validade e Reprodutibilidade no Brasil. Revista Brasileira de Atividade Física & Saúde 6:5–18. https://doi.org/10.12820/rbafs.v.6n2p5-18
Kuller LH (2009) Weight Loss and Reduction of Blood Pressure and Hypertension. Hypertension 54:700–701. https://doi.org/10.1161/HYPERTENSIONAHA.109.138891
He FJ, Li J, MacGregor GA (2013) Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 346. https://doi.org/10.1136/bmj.f1325
Gowrishankar M, Blair B, Rieder MJ (2020) Dietary intake of sodium by children: Why it matters. Paediatr Child Health 25:47–61. https://doi.org/10.1093/pch/pxz153
Rezende-Alves K, Hermsdorff HHM, da Miranda AE, S et al (2021) Food processing and risk of hypertension: Cohort of Universities of Minas Gerais, Brazil (CUME Project). Public Health Nutr 24:4071–4079. https://doi.org/10.1017/S1368980020002074
Monteiro CA, Cannon G, Moubarac J-C et al (2018) The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr 21:5–17. https://doi.org/10.1017/S1368980017000234
Crovetto MM, Uauy R, Martins AP et al (2014) Household availability of ready-to-consume food and drink products in Chile: impact on nutritional quality of the diet. Rev Med Chil 142:850–858. https://doi.org/10.4067/S0034-98872014000700005
da Louzada ML, C, Ricardo CZ, Steele EM et al (2018) The share of ultra-processed foods determines the overall nutritional quality of diets in Brazil. Public Health Nutr 21:94–102. https://doi.org/10.1017/S1368980017001434
Zinöcker MK, Lindseth IA (2018) The Western Diet–Microbiome-Host Interaction and Its Role in Metabolic Disease. Nutrients 10:365. https://doi.org/10.3390/nu10030365
Flint HJ, Scott KP, Louis P, Duncan SH (2012) The role of the gut microbiota in nutrition and health. Nat Rev Gastroenterol Hepatol 9:577–589. https://doi.org/10.1038/nrgastro.2012.156
Laster J, Bonnes SL, Rocha J (2019) Increased Use of Emulsifiers in Processed Foods and the Links to Obesity. Curr Gastroenterol Rep 21:61. https://doi.org/10.1007/s11894-019-0723-4
Xu H, Li Y, Shang X et al (2020) Effect of Comprehensive Interventions Including Nutrition Education and Physical Activity on High Blood Pressure among Children: Evidence from School-Based Cluster Randomized Control Trial in China. Int J Environ Res Public Health 17. https://doi.org/10.3390/ijerph17238944
Ortiz-Marrón H, Cabañas Pujadas G, Ortiz-Pinto MA et al (2023) Changes in general and abdominal obesity in children at 4, 6 and 9 years of age and their association with other cardiometabolic risk factors. Eur J Pediatr. https://doi.org/10.1007/s00431-022-04802-3
Oliveira T, Ribeiro I, Jurema-Santos G et al (2020) Can the Consumption of Ultra-Processed Food Be Associated with Anthropometric Indicators of Obesity and Blood Pressure in Children 7 to 10 Years Old? Foods 9:1567. https://doi.org/10.3390/foods9111567
Du S, Neiman A, Batis C et al (2014) Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China123. Am J Clin Nutr 99:334–343. https://doi.org/10.3945/ajcn.113.059121
Perez V, Chang ET (2014) Sodium-to-Potassium Ratio and Blood Pressure, Hypertension, and Related Factors12. Adv Nutr 5:712–741. https://doi.org/10.3945/an.114.006783
Pereira TSS, Mill JG, Griep RH et al (2019) Effect of urinary sodium-to-potassium ratio change on blood pressure in participants of the longitudinal health of adults study - ELSA-Brasil. Medicine (Baltimore) 98. https://doi.org/10.1097/MD.0000000000016278
Iwahori T, Miura K, Ueshima H (2017) Time to Consider Use of the Sodium-to-Potassium Ratio for Practical Sodium Reduction and Potassium Increase. Nutrients 9. https://doi.org/10.3390/nu9070700
Vadiveloo M, Sacks FM, Champagne CM et al (2016) Greater Healthful Dietary Variety Is Associated with Greater 2-Year Changes in Weight and Adiposity in the Preventing Overweight Using Novel Dietary Strategies (POUNDS Lost) Trial. J Nutr 146:1552–1559. https://doi.org/10.3945/jn.115.224683
Willett WC, Howe GR, Kushi LH (1997) Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr 65:1220S–1228S; discussion 1229S–1231S. https://doi.org/10.1093/ajcn/65.4.1220S
Acknowledgements
The investigators would like to thank all patients and parents for their participation in this study.
Funding
This study was supported by the National Council for Scientific and Technological Development (CNPq) and from Carlos Chagas Filho Foundation for Research Support in the State of Rio de Janeiro (FAPERJ).
Author information
Authors and Affiliations
Contributions
Designed the experiments: Diana Barbosa Cunha and Rosely Sichieri. Conceived the experiments: Caroline Cortes and Joana Maia Brandão. Analyzed the data: Caroline Cortes, Vitor Barreto Paravidino and Rosely Sichieri. Wrote and approved the final version of the paper: Caroline Cortes, Joana Maia Brandão, Diana Barbosa Cunha, Vitor Barreto Paravidino and Rosely Sichieri.
Corresponding author
Ethics declarations
Ethical approval
This study was conducted following the guidelines of the Consolidated Standards of Reporting Trials (CONSORT 2010). Approval was granted by the Research Ethics Committee of Pedro Ernesto University Hospital (CAAE: 87593118000005259).
Consent to participate
The Informed Consent Form was signed by the child's parents or legal guardians and the children signed the Informed Assent Form.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Communicated by Gregorio Milani
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cortes, C., Brandão, J.M., Cunha, D.B. et al. Blood pressure variation and ultra-processed food consumption in children with obesity. Eur J Pediatr 182, 4077–4085 (2023). https://doi.org/10.1007/s00431-023-05076-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05076-z