Abstract
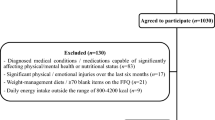
The aim of this cross-sectional study was to analyze the association between adherence to the Mediterranean diet (MedDiet) and its dietary components and health-related quality of life (HRQoL) in a sample of Spanish adolescents. A total sample of 634 adolescents was included (mean age: 13.96 ± 1.54 years; 56.9% girls). The Mediterranean Diet Quality Index in children and adolescents (KIDMED) and the KIDSCREEN-10 were used to assess adherence to the MedDiet and its components and HRQoL, respectively. Linear regression was applied to estimate the association between overall adherence to the MedDiet and HRQoL. Cluster analysis was used to establish subgroups according to different patterns of MedDiet component consumption. Higher overall adherence to the MedDiet was significantly associated with greater HRQoL (unstandardized beta coefficient [β] = 0.329; 95% CI: 0.108, 0.550; p = 0.004), even after adjustment for sociodemographic, physical and lifestyle covariates (β = 0.228; 95% CI: 0.007, 0.449; p = 0.043). When different clusters were established according to similar features of MedDiet component consumption, the cluster with a higher percentage of individuals who skipped breakfast had significantly lower scores on the HRQoL scale (p < 0.05)
Conclusions: Our findings highlight the relevance of considering the specific patterns of food group consumption and MedDiet-related behaviors and not just the overall measure of MedDiet adherence for promoting HRQoL in adolescents.
What is Known: |
• Previous studies have shown that some lifestyle behaviors, such as dietary habits, could be associated with health-related quality of life. |
• According to our results, higher adherence to the Mediterranean diet pattern was associated with greater health-related quality of life in adolescents. |
What is New: |
• Skipping breakfast seems to have a crucial role in health-related quality of life among adolescents. |
• These results could lead to the development of more specific dietary strategies for increasing health-related quality of life in adolescents. |


Similar content being viewed by others
Abbreviations
- β:
-
Unstandardized beta coefficient
- CI:
-
Confidence interval
- FAS-III:
-
Family Affluence Scale
- FFQ:
-
Food frequency questionnaire
- HRQoL:
-
Health-related quality of life
- KIDMED:
-
Mediterranean Diet Quality Index in children and adolescents
- MedDiet:
-
Mediterranean diet
- YAP-S:
-
Spanish version of the Youth Activity Profile
References
Patton GC, Viner R (2007) Pubertal transitions in health. Lancet 369:1130–1139. https://doi.org/10.1016/S0140-6736(07)60366-3
World Health Organization (2020) Adolescent mental health. https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health. Accessed 14 Jan 2023
Frisén A (2007) Measuring health-related quality of life in adolescence. Acta Paediatr Int J Paediatr 96:963–968. https://doi.org/10.1111/J.1651-2227.2007.00333.X
Solans M, Pane S, Estrada MD et al (2008) Health-related quality of life measurement in children and adolescents: A systematic review of generic and disease-specific instruments. Value Heal 11:742–764. https://doi.org/10.1111/J.1524-4733.2007.00293.X
Testa MA, Simonson DC (1996) Assessment of quality-of-life outcomes. N Engl J Med 334:835–840. https://doi.org/10.1056/NEJM199603283341306
Kaplan RM, Hays RD (2022) Health-Related Quality of Life Measurement in Public Health. Annu Rev Public Health 43:355–373. https://doi.org/10.1146/ANNUREV-PUBLHEALTH-052120-012811
Matza LS, Swensen AR, Flood EM et al (2004) Assessment of health-related quality of life in children: a review of conceptual, methodological, and regulatory issues. Value Health 7:79–92. https://doi.org/10.1111/J.1524-4733.2004.71273.X
Zullig KJ, Valois RF, Huebner ES, Drane JW (2005) Adolescent health-related quality of life and perceived satisfaction with life. Qual Life Res 14:1573–1584. https://doi.org/10.1007/S11136-004-7707-Y
Faure MI, Urquidi C, Bustamante F et al (2018) Association of health-related quality of life and suicidal risk in adolescents: A cross-sectional study. Rev Chil Pediatr 89:318–324. https://doi.org/10.4067/S0370-41062018005000103
Vajdi M, Farhangi MA (2020) A systematic review of the association between dietary patterns and health-related quality of life. Health Qual Life Outcomes 18. https://doi.org/10.1186/s12955-020-01581-z
Wu XY, Zhuang LH, Li W et al (2019) The influence of diet quality and dietary behavior on health-related quality of life in the general population of children and adolescents: a systematic review and meta-analysis. Qual Life Res 28:1989–2015. https://doi.org/10.1007/S11136-019-02162-4
Bach-Faig A, Berry EM, Lairon D et al (2011) Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr 14:2274–2284. https://doi.org/10.1017/S1368980011002515
Bizzozero-Peroni B, Brazo-Sayavera J, Martínez-Vizcaíno V et al (2022) High Adherence to the Mediterranean Diet is Associated with Higher Physical Fitness in Adults: a Systematic Review and Meta-Analysis. Adv Nutr 13. https://doi.org/10.1093/ADVANCES/NMAC104
Lassale C, Batty GD, Baghdadli A et al (2019) Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol Psychiatry 24:965–986. https://doi.org/10.1038/s41380-018-0237-8
Sofi F, Macchi C, Abbate R et al (2014) Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr 17:2769–2782. https://doi.org/10.1017/S1368980013003169
Romero-Robles MA, Ccami-Bernal F, Ortiz-Benique ZN et al (2022) Adherence to Mediterranean diet associated with health-related quality of life in children and adolescents: a systematic review. BMC Nutr 8:57. https://doi.org/10.1186/s40795-022-00549-0
López-Gil JF, García-Hermoso A (2022) Adherence to the Mediterranean diet and subjective well-being among Chilean children. Appetite 172. https://doi.org/10.1016/J.APPET.2022.105974
Nabbosa S, Lee S (2022) Associations between Food Groups and Health-Related Quality of Life in Korean Adults. Nutrients 14. https://doi.org/10.3390/nu14173643
Silvers KM, Scott KM (2002) Fish consumption and self-reported physical and mental health status. Public Health Nutr 5:427–431. https://doi.org/10.1079/PHN2001308
Lopez-Garcia E, Leon-Muñoz L, Guallar-Castillon P, Rodríguez-Artalejo F (2015) Habitual yogurt consumption and health-related quality of life: A prospective cohort study. J Acad Nutr Diet 115:31–39. https://doi.org/10.1016/j.jand.2014.05.013
Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13:3–9. https://doi.org/10.1097/00041433-200202000-00002
Wirfält E, Mattisson I, Gullberg B, Berglund G (2000) Food patterns defined by cluster analysis and their utility as dietary exposure variables: a report from the Malmö Diet and Cancer Study. Public Health Nutr 3:159–173. https://doi.org/10.1017/S1368980000000197
Hulshof KFAM, Wedel M, Lowik MRH et al (1992) Clustering of dietary variables and other lifestyle factors (Dutch Nutritional Surveillance System). J Epidemiol Community Health 46:417–424. https://doi.org/10.1136/JECH.46.4.417
López-Gil JF (2022) The Eating Healthy and Daily Life Activities (EHDLA) Study. Child (Basel, Switzerland) 9. https://doi.org/10.3390/CHILDREN9030370
Aymerich M, Berra S, Guillamón I et al (2005) Development of the Spanish version of the KIDSCREEN, a health-related quality of life instrument for children and adolescents. Gac Sanit 19:93–102. https://doi.org/10.1157/13074363
Serra-Majem L, Ribas L, Ngo J et al (2004) Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr 7:931–935. https://doi.org/10.1079/PHN2004556
Rollo S, Antsygina O, Tremblay MS (2020) The whole day matters: Understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J Sport Heal Sci 9:493–510. https://doi.org/10.1016/J.JSHS.2020.07.004
Iaccarino Idelson P, Scalfi L, Valerio G (2017) Adherence to the Mediterranean Diet in children and adolescents: A systematic review. Nutr Metab Cardiovasc Dis 27:283–299. https://doi.org/10.1016/J.NUMECD.2017.01.002
Currie C, Molcho M, Boyce W et al (2008) Researching health inequalities in adolescents: the development of the Health Behaviour in School-Aged Children (HBSC) family affluence scale. Soc Sci Med 66:1429–1436. https://doi.org/10.1016/J.SOCSCIMED.2007.11.024
Segura-Díaz JM, Barranco-Ruiz Y, Saucedo-Araujo RG et al (2021) Feasibility and reliability of the Spanish version of the Youth Activity Profile questionnaire (YAP-Spain) in children and adolescents. J Sports Sci 39:801–807. https://doi.org/10.1080/02640414.2020.1847488
Favier J, Ireland-Ripert J, Feinberg M TC (1995) Répertoire Général Des Aliments: Tables de Composition. Technique & Documentation: INRA: Ciqual-Regal, Paris
Benjamini Y, Hochberg Y (1995) Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J R Stat Soc Ser B 57:289–300. https://doi.org/10.1111/J.2517-6161.1995.TB02031.X
Ferrer-Cascales R, Sánchez-Sansegundo M, Ruiz-Robledillo N et al (2018) Eat or Skip Breakfast? The Important Role of Breakfast Quality for Health-Related Quality of Life, Stress and Depression in Spanish Adolescents. Int J Environ Res Public Health 15. https://doi.org/10.3390/IJERPH15081781
Huang CJ, Hu HT, Fan YC et al (2010) Associations of breakfast skipping with obesity and health-related quality of life: evidence from a national survey in Taiwan 34:720–725
Coulthard JD, Palla L, Pot GK (2017) Breakfast consumption and nutrient intakes in 4–18-year-olds: UK National Diet and Nutrition Survey Rolling Programme (2008–2012). https://doi.org/10.1017/S0007114517001714
Monzani A, Ricotti R, Caputo M et al (2019) A Systematic Review of the Association of Skipping Breakfast with Weight and Cardiometabolic Risk Factors in Children and Adolescents. What Should We Better Investigate in the Future? Nutrients 11. https://doi.org/10.3390/NU11020387
Zahedi H, Djalalinia S, Sadeghi O et al (2022) Breakfast consumption and mental health: a systematic review and meta-analysis of observational studies. Nutr Neurosci 25:1250–1264. https://doi.org/10.1080/1028415X.2020.1853411
Adolphus K, Lawton CL, Champ CL, Dye L (2016) The Effects of Breakfast and Breakfast Composition on Cognition in Children and Adolescents: A Systematic Review. Adv Nutr 7:590S-612S. https://doi.org/10.3945/AN.115.010256
Rampersaud GC, Pereira MA, Girard BL et al (2005) Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc 105:743–760. https://doi.org/10.1016/j.jada.2005.02.007
Sánchez-Villegas A, Henríquez-Sánchez P, Ruiz-Canela M et al (2015) A longitudinal analysis of diet quality scores and the risk of incident depression in the SUN Project. BMC Med 13. https://doi.org/10.1186/S12916-015-0428-Y
Gómez-Pinilla F (2008) Brain foods: The effects of nutrients on brain function. Nat Rev Neurosci 9:568–578. https://doi.org/10.1038/nrn2421
Serra-Majem L, Román-Viñas B, Sanchez-Villegas A et al (2019) Benefits of the Mediterranean diet: Epidemiological and molecular aspects. Mol Aspects Med 67:1–55. https://doi.org/10.1016/j.mam.2019.06.001
Henríquez Sánchez P, Ruano C, De Irala J et al (2012) Adherence to the Mediterranean diet and quality of life in the SUN Project. Eur J Clin Nutr 66:360–368. https://doi.org/10.1038/ejcn.2011.146
Ferrer-Cascales R, Albaladejo-Blázquez N, Ruiz-Robledillo N et al (2019) Higher Adherence to the Mediterranean Diet is Related to More Subjective Happiness in Adolescents: The Role of Health-Related Quality of Life. Nutrients 11. https://doi.org/10.3390/NU11030698
Conner TS, Brookie KL, Carr AC et al (2017) Let them eat fruit! The effect of fruit and vegetable consumption on psychological well-being in young adults: A randomized controlled trial. PLoS One 12. https://doi.org/10.1371/JOURNAL.PONE.0171206
Gantenbein K V., Kanaka-Gantenbein C (2021) Mediterranean Diet as an Antioxidant: The Impact on Metabolic Health and Overall Wellbeing. Nutrients 13. https://doi.org/10.3390/NU13061951
Bourre JM (2006) Effects of nutrients (in food) on the structure and function of the nervous system: Update on dietary requirements for brain. Part 2: Macronutrients. J Nutr Heal Aging 10:386–399
Fulton SL, McKinley MC, Neville CE et al (2017) The effect of increased fruit and vegetable consumption on selected macronutrient and micronutrient intakes in four randomised-controlled trials. Br J Nutr 117:1270–1278. https://doi.org/10.1017/S0007114517001088
Sánchez-Villegas A, Galbete C, Martinez-González MA et al (2011) The effect of the Mediterranean diet on plasma brain-derived neurotrophic factor (BDNF) levels: the PREDIMED-NAVARRA randomized trial. Nutr Neurosci 14:195–201. https://doi.org/10.1179/1476830511Y.0000000011
Beam A, Clinger E, Hao L (2021) Effect of Diet and Dietary Components on the Composition of the Gut Microbiota. Nutrients 13. https://doi.org/10.3390/NU13082795
Osadchiy V, Martin CR, Mayer EA (2019) The Gut-Brain Axis and the Microbiome: Mechanisms and Clinical Implications. Clin Gastroenterol Hepatol 17:322–332. https://doi.org/10.1016/J.CGH.2018.10.002
Fung TC, Olson CA, Hsiao EY (2017) Interactions between the microbiota, immune and nervous systems in health and disease. Nat Neurosci 20:145–155. https://doi.org/10.1038/NN.4476
Valles-Colomer M, Falony G, Darzi Y et al (2019) (2019) The neuroactive potential of the human gut microbiota in quality of life and depression. Nat Microbiol 44(4):623–632. https://doi.org/10.1038/S41564-018-0337-X
Berding K, Vlckova K, Marx W et al (2021) Diet and the Microbiota-Gut-Brain Axis: Sowing the Seeds of Good Mental Health. Adv Nutr 12:1239–1285
Mujcic R, Oswald AJ (2016) Evolution of well-being and happiness after increases in consumption of fruit and vegetables. Am J Public Health 106:1504–1510. https://doi.org/10.2105/AJPH.2016.303260
Costarelli V, Koretsi E, Georgitsogianni E (2013) Health-related quality of life of Greek adolescents: The role of the Mediterranean diet. Qual Life Res 22:951–956
López-Gil JF, Smith L, López-Bueno R, Tárraga-López PJ (2022) Breakfast and psychosocial behavioural problems in young population: The role of status, place, and habits. Front Nutr 9. https://doi.org/10.3389/FNUT.2022.871238
Acknowledgments
JFL-G is a Margarita Salas Fellow (Universidad Pública de Navarra—1225/2022). AEM is a Beatriz Galindo Fellow (Spanish Ministry of Education, Culture and Sport – BEAGAL 18/00093). The authors would like to express their gratitude to Ayuntamiento de Archena, as well as the participation of all the adolescents, parents/legal guardians, physical education teachers, schools, and staff implicated, and wish to thank them for the information provided. BB‐P is a Beatriz Galindo Fellow (University of Castilla-La Mancha co-financed by the European Social Fund – 2020‐ PREDUCLM-16746). RF‐R was supported by a grant from the Spanish Ministry of Education, Culture and Sport (FPU 19/00167).
Author information
Authors and Affiliations
Contributions
EJ-L and JFL-G developed the methodological approach. EJ-L and JFL-G performed the data analyses and prepared the tables and figures, with inputs from AEM. BB-P, RF-R, DV-M, RL-B, and MG-M provided further data interpretation. EJ-L wrote the first draft of the manuscript with further input from all coauthors. All authors contributed to drafting the work or reviewing it critically and made substantial contributions. EJ-L had final responsibility for the decision to submit for publication. All authors had full access to all the data in the study and accept responsibility to submit for publication.
Corresponding author
Ethics declarations
Competing interests and funding
The authors have declared that they have no competing or potential conflicts of interest. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical statement
This study was performed in line with the principles of the Declaration of Helsinki. This obtained ethics approval from the Bioethics Committee of the University of Murcia (ID 2218/2018) and the Ethics Committee of the Albacete University Hospital Complex and the Albacete Integrated Care Management (ID 2021–85).
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiménez-López, E., Mesas, A.E., Bizzozero-Peroni, B. et al. Clustering of Mediterranean dietary patterns linked with health-related quality of life in adolescents: the EHDLA study. Eur J Pediatr 182, 4113–4121 (2023). https://doi.org/10.1007/s00431-023-05069-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05069-y