Abstract
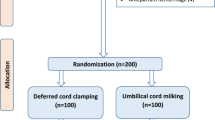
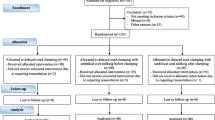
Routine practice of delayed cord clamping (DCC) is the standard of care in vigorous neonates. However there is no consensus on the recommended approach to placental transfusion in non-vigorous neonates. In this trial, we tried to examine the effect of cut umbilical cord milking (C-UCM) as compared to early cord clamping (ECC) on hematological and clinical hemodynamic parameters in non-vigorous preterm neonates of 30–35 weeks gestation. The primary outcome assessed was venous hematocrit (Hct) at 48 (± 4) hours of postnatal age. The important secondary outcomes assessed were serum ferritin at 6 weeks of age, mean blood pressure in the initial transitional phase along with important neonatal morbidities and potential complications. In this single centre randomized controlled trial, 134 non vigorous neonates of 30–35 weeks gestation were allocated in a 1:1 ratio to either C-UCM (n = 67) or ECC (n = 67). For statistical analysis, unpaired Student t and Chi square or Fisher’s exact test were used. The mean Hct at 48 h was higher in the C-UCM group as compared to the control group, 50.24(4.200) vs 46.16(2.957), p < .0001. Also significantly higher was the mean Hct at 12 h, 6 weeks and mean serum ferritin at 6 weeks of age in the milked group (p < .0001). Mean blood pressure at 1 h and 6 h was also significantly higher in the milked arm. Need for transfusion and inotropes was less in the milked group but not statistically significant. No significant difference in potential complications was observed between the groups.
Conclusion: C-UCM stabilizes initial blood pressure and results in higher hematocrit and improved iron stores. It can be an alternative to DCC in non-vigorous preterm neonates of 30–35 weeks’ gestation. Further large multicentric studies are needed to fully establish its efficacy and safety.
Trial registration: CTRI/2021/12/038606; registration date December 14, 2021.
What is Known: • DCC is the routinely recommended method of placental transfusion for vigorous neonates but no consensus exist for neonates requiring resuscitation at birth. • C-UCM is easier to perform in non-vigorous neonates but there is paucity of studies in the preterm population. | |
What is New: • C-UCM is effective as well as safe in non-vigorous preterm neonates of 30–35 weeks gestational age. • C-UCM holds promise as an alternative to DCC, especially in resource limited settings and in situations where the later is not feasible. |


Similar content being viewed by others
Data Availability
Abbreviations
- C-UCM:
-
Cut umbilical cord milking
- DCC:
-
Delayed cord clamping
- ECC:
-
Early/immediate cord clamping
- Hb:
-
Hemoglobin
- Hct:
-
Hematocrit
- ILCOR:
-
International Liaison Committee on Resuscitation
- I-UCM:
-
Intact umbilical cord milking
- IVH:
-
Intraventricular hemorrhage
- MINVI:
-
Milking in non-vigorous infants
- NRP:
-
Neonatal resuscitation program
- PRBC:
-
Packed red blood cell
- SD:
-
Standard deviation
References
WHO Guidelines Approved by the Guidelines Review Committee (2012) Guidelines on Basic Newborn Resuscitation. World Health Organization, Geneva
Perlman JM, Wyllie J, Kattwinkel J, Wyckoff MH, Aziz K, Guinsburg R et al (2015) Part 7: neonatal resuscitation: 2015 International consensus on cardiopulmonaryresuscitation and emergency cardiovascular care science with treatment recommendations (Reprint). Pediatrics 136(Suppl. 2):S120–S166. https://doi.org/10.1542/peds.2015-3373D
Committee opinion no (2017) 684: delayed umbilical cord clamping after birth. Obstet Gynecol 129:e5-10. https://doi.org/10.1097/AOG.0000000000001860
Katheria AC, Lakshminrusimha S, Rabe H, McAdams R, Mercer JS (2017) Placental transfusion: a review. J Perinatol 37(2):105–111. https://doi.org/10.1038/jp.2016.151
Mangla MK, Thukral A, Sankar MJ, Agarwal R, Deorari AK, Paul VK (2020) Effect of Umbilical Cord Milking vs Delayed Cord Clamping on Venous Hematocrit at 48 Hours in Late Preterm and Term Neonates: A Randomized Controlled Trial. Indian Pediatr 57(12):1119–1123. PMID: 33034301
Katheria AC, Truong G, Cousins L, Oshiro B, Finer NN (2015) Umbilical Cord Milking Versus Delayed Cord Clamping in Preterm Infants. Pediatrics 136(1):61–69. https://doi.org/10.1542/peds.2015-0368
Orpak ÜS, Ergin H, Çıralı C, Özdemir ÖMA, Koşar Can Ö, Çelik Ü (2021) Comparison of cut and intact cord milking regarding cerebral oxygenation, hemodynamic and hematological adaptation of term infants. J Matern Fetal Neonatal Med 34(14):2259–2266. https://doi.org/10.1080/14767058.2019.1662781
Upadhyay A, Gothwal S, Parihar R, Garg A, Gupta A, Chawla D et al (2013) Effect of umbilical cord milking in term and near term infants: randomized control trial. Am J Obstet Gynecol 208(2):120.e1-120.e6. https://doi.org/10.1016/j.ajog.2012.10.884
Simnin A, Safarulla A, Farmer Z, Coleman J, Sutton D, Wheeler K et al (2020) Cut umbilical cord milking: an ineffective method of placental transfusion in preterm infants? J Matern Fetal Neonatal Med 33(18):3132–3135. https://doi.org/10.1080/14767058.2019.1569616
Ram Mohan G, Shashidhar A, Chandrakala BS, Nesargi S, Suman Rao PN (2018) Umbilical cord milking in preterm neonates requiring resuscitation: A randomized controlled trial. Resuscitation 130:88–91. https://doi.org/10.1016/j.resuscitation.2018.07.003
McAdams RM, Fay E, Delaney S (2018) Whole blood volumes associated with milking intact and cut umbilical cords in term newborns. J Perinatol 38(3):245–250. https://doi.org/10.1038/s41372-017-0002-x
Kliegman R, Walsh M (1987) Neonatal necrotizing enterocolitis: Pathogenesis, classification, and spectrum of illness. Curr Probl Pediatr 17(4):219–288. https://doi.org/10.1016/0045-9380(87)90031-4
Inder TE, Perlman JM, Volpe JJ (2017) Preterm Intraventricular Hemorrhage/ Posthemorrhagic Hydrocephalus. In: Inder TE, Volpe JJ, du Plessis AJ, de Vries LS, Perlman JM, Darras BT et al (eds) Volpe’s neurology of the newborn, 6th edn. Elsevier - Health Sciences Division, Philadelphia, PA, p 637
Chiang MF, Quinn GE, Fielder AR, Ostmo SR, Paul Chan R, Berrocal A et al (2021) International Classification of Retinopathy of Prematurity. Third Edition. Ophthalmology 128(10):e51–e68. https://doi.org/10.1016/j.ophtha.2021.05.031
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA et al (2005) Validation of the National Institutes of Health Consensus Definition of Bronchopulmonary Dysplasia. Pediatrics 116(6):1353–1360. https://doi.org/10.1542/peds.2005-0249
Hosono S, Hine K, Nagano N, Taguchi Y, Yoshikawa K, Okada T et al (2015) Residual blood volume in the umbilical cord of extremely premature infants. Pediatr Int 57(1):68–71. https://doi.org/10.1111/ped.12464
Jaiswal P, Upadhyay A, Gothwal S, Singh D, Dubey K, Garg A et al (2015) Comparison of two types of intervention to enhance placental redistribution in term infants: randomized control trial. Eur J Pediatr 174(9):1159–1167
Katheria AC, Clark E, Yoder B, Schmölzer GM, Yan Law BH, El-Naggar W et al (2023) Umbilical cord milking in nonvigorous infants: a cluster-randomized crossover trial. Am J Obstet Gynecol 228(2):217.e1-217.e14. https://doi.org/10.1016/j.ajog.2022.08.015
Kumar B, Upadhyay A, Gothwal S, Jaiswal V, Joshi P, Dubey K (2015) Umbilical cord milking and hematological parameters in moderate to late preterm neonates: A randomized controlled trial. Indian Pediatr 52(9):753–757. https://doi.org/10.1007/s13312-015-0711-1
Rabe H, Jewison A, Fernandez Alvarez R, Crook D, Stilton D, Bradley R et al (2011) Milking Compared With Delayed Cord Clamping to Increase Placental Transfusion in Preterm Neonates. Obstet Gynecol 117(2):205–211. https://doi.org/10.1097/AOG.0b013e3181fe46ff
Mercer JS, Erickson-Owens DA, Deoni SC, Dean DC, Collins J, Parker AB et al (2018) Effects of Delayed Cord Clamping on 4-Month Ferritin Levels, Brain Myelin Content, and Neurodevelopment: A Randomized Controlled Trial. J Pediatr 203:266-272.e2. https://doi.org/10.1016/j.jpeds.2018.06.006
Al-Wassia H, Shah PS (2015) Efficacy and safety of umbilical cord milking at birth: a systematic review and meta-analysis. JAMA Pediatr 169(1):18–25. https://doi.org/10.1001/jamapediatrics.2014.1906
Katheria A, Reister F, Essers J, Mendler M, Hummler H, Subramaniam A et al (2019) Association of Umbilical Cord Milking vs Delayed Umbilical Cord Clamping With Death or Severe Intraventricular Hemorrhage Among Preterm Infants. JAMA 322(19):1877. https://doi.org/10.1001/jama.2019.16004
Balasubramanian H, Ananthan A, Jain V, Rao SC, Kabra N (2020) Umbilical cord milking in preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 105(6):572–580. https://doi.org/10.1136/archdischild-2019-318627
Barboza JJ, Albitres-Flores L, Rivera-Meza M, Rodriguez-Huapaya J, Caballero-Alvarado J, Pasupuleti V et al (2021) Short-term efficacy of umbilical cord milking in preterm infants: systematic review and meta-analysis. Pediatr Res 89(1):22–30. https://doi.org/10.1038/s41390-020-0902-x
Acknowledgements
We thank the babies and their parents, nurses and residents of the unit. We offer our sincere gratitude to the laboratory technicians for their help and support.
Author information
Authors and Affiliations
Contributions
The study was conceptualized, designed and first protocol was developed by Rajib Losan Bora. Bijan Saha and Sambhunath Bandyopadhyay contributed significantly in each stage and improved the content. Bijan Saha and Suchandra Mukherjee reviewed and finalised the protocol. Rajib Losan Bora did the data collection supervised by Bijan Saha and Sambhunath Bandyopadhyay. Abhijit Hazra did the data analysis. Rajib Losan Bora prepared the first draft. Suchandra Mukherjee and Sambhunath Bandyopadhyay critically reviewed the manuscript. Rajib Losan Bora and Bijan Saha revised and finalised the manuscript. All the authors approved the final manuscript as submitted and agree to be accountable for all aspect of the work.
Corresponding author
Ethics declarations
Ethics approval
The study was conducted in conformity with the Declaration of Helsinki's ethical standards and in a manner that was consistent with good clinical practice. Approval of the trial was obtained from institutional ethics committee of the Institute of Post Graduate Medical Education and Research, Kolkata, India (IPGME&R/IEC/2021/490). The study's registration number with the Clinical Trial Registry of India (CTRI) was CTRI/2021/12/038606.
Consent to participate
Informed written consent was obtained from all legal guardians before participating in the study.
Consent for publication
Informed written consent was obtained from parents or authorized legal guardian of all included participants for publication of anonymous patients’ data.
Conflict of interest
The authors declare no potential conflict of interest.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bora, R.L., Bandyopadhyay, S., Saha, B. et al. Cut umbilical cord milking (C-UCM) as a mode of placental transfusion in non-vigorous preterm neonates: a randomized controlled trial. Eur J Pediatr 182, 3883–3891 (2023). https://doi.org/10.1007/s00431-023-05063-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05063-4