Abstract
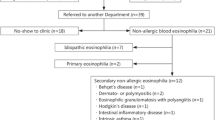
Eosinophilia is common in children and may be caused by various disorders. Large-cohort studies, including mild cases, are limited in children. This study aimed to reveal underlying etiologies of childhood eosinophilia and to create a diagnostic algorithm. Children (< 18 years) with absolute eosinophil counts (AECs) ≥ 0.5 × 109/L were reviewed from medical files. Clinical characteristics and laboratory values were recorded. Patients were grouped based on the severity of eosinophilia as mild (0.5–1.5 × 109/L), moderate (≥ 1.5 × 109/L) and severe (≥ 5.0 × 109/L). An algorithm was formed to evaluate these patients. We included 1178 children with mild (80.8%), moderate (17.8%) and severe eosinophilia (1.4%). The most common reasons of eosinophilia were allergic diseases (80%), primary immunodeficiency (PID) (8.5%), infectious diseases (5.8%), malignancies (0.8%) and rheumatic diseases (0.7%). Only 0.3% of children presented with idiopatic hypereosinophilic syndrome. Allergic diseases and PIDs were the most common etiologies in mild/moderate and severe groups, respectively. The median duration of eosinophilia was 7.0 (3.0–17.0) months in the study population and was the shortest in severe cases (2.0 (2.0–5.0) months). Multiple logistic regression analysis demonstrated food allergy [OR:1.866, 95%CI:1.225–2.842, p = 0.004] and PIDs [OR:2.200, 95%CI:1.213–3.992, p = 0.009] as independent factors for childhood eosinophilia. A diagnostic algorithm including mild form was presented for childhood eosinophilia.
Conclusion: Eosinophilia was frequently determined due to secondary causes; allergic diseases in mild/moderate eosinophilia, PIDs in severe group. Etiology of eosinophilia was diverse, and an algorithm concerning the severity of eosinophilia would be practical and rational.
What is Known: • In children, eosinophilia is common, and mild eosinophilia occurs frequently. • Malignancies presents frequently with severe eosinophilia. | |
What is New: • Primary immunodeficiencies were not a rare cause of eosinophilia, especially in countries such as the Middle East and eastern Mediterranean countries, where the countries consanguineous marriages are common, and should be investigated in children with eosinophilia who do not have allergic or infectious diseases. • In literature, there are many algorithms about childhood hypereosinophilia. However, mild eosinophilia is extremely important in children. Because all patients with malignancy and most of the patients with rheumatic diseases presented with mild eosinophilia. Therefore, we proposed an algorithm for childhood eosinophilia that includes mild eosinophilia besides moderate and severe cases. |



Similar content being viewed by others
References
Curtis C, Ogbogu PU (2015) Evaluation and differential diagnosis of persistent marked eosinophilia. Immunol Allergy Clin North Am 35:387–402
Valent P, Klion AD, Horny H-P et al (2012) Contemporary consensus proposal on criteria and classification of eosinophilic disorders and related syndromes. J Allergy Clin Immunol 130:607–612
Burris D, Rosenberg CE, Schwartz JT et al (2019) Pediatric hypereosinophilia: characteristics, clinical manifestations, and diagnoses. J Allergy Clin Immunol Pract 7:2750–2758
Williams KW, Ware J, Abiodun A, Holland-Thomas NC, Khoury P, Klion AD (2016) Hypereosinophilia in children and adults: a retrospective comparison. J Allergy Clin Immunol Pract 4:941–947
Kim K-M, Bae M-H, Kim Y-M et al (2014) Cause and incidence of eosinophilia in children: a single center study in one year. Allergy Asthma Respir Dis 2:358–361
Chipps BE, Murphy KR, Oppenheimer J (2022) 2020 NAEPP Guidelines Update and GINA 2021—Asthma Care Differences, Overlap, and Challenges. J Allerg Clin Immunol Pract 10(1S):S19–S30
Bousquet J, Anto JM, Bachert C et al (2019) From ARIA guidelines to the digital transformation of health in rhinitis and asthma multimorbidity. Eur RespirJ 54:1901023
Eichenfield LF, Tom WL, Berger TG et al (2014) Guidelines of care for the management of atopic dermatitis: section 2. Management and treatment of atopic dermatitis with topical therapies. J Am Acad Dermatol 71:116–132
Halken S, Muraro A, de Silva D et al (2021) EAACI guideline: Preventing the development of food allergy in infants and young children (2020 update). Pediatr Allergy Immunol 32:843–858
Broyles AD, Banerji A, Barmettler S et al (2020) Practical guidance for the evaluation and management of drug hypersensitivity: specific drugs. J Allergy Clin Immunol Pract 8:S16–S116
Tangye SG, Al-Herz W, Bousfiha A et al (2022) Human inborn errors of immunity: 2022 update on the classification from the International Union of Immunological Societies Expert Committee. J Clin Immunol 42:1473–1507
Eades-Perner AM, Gathmann B, Knerr V et al (2007) The European internet-based patient and research database for primary immunodeficiencies: results 2004–06. Clin Exp Immunol 147:306–312
Picard C, Gaspar HB, Al-Herz W et al (2018) International union of immunological societies: 2017 primary immunodeficiency diseases committee report on inborn errors of immunity. J Clin Immunol 38:96–128
Niggemann B, Lange L, Finger A, Ziegert M, Müller V, Beyer K (2012) Accurate oral food challenge requires a cumulative dose on a subsequent day. J Allergy Clin Immunol 130:261–263
Valent P, Klion AD, Horny HP et al (2012) Contemporary consensus proposal on criteria and classification of eosinophilic disorders and related syndromes. J Allergy Clin Immunol 130:607–612
Shomali W, Gotlib J (2022) World Health Organization-defined eosinophilic disorders: 2022 update on diagnosis, risk stratification, and management. Am J Hematol 97(1):129–148
Butt NM, Lambert J, Ali S et al (2017) Guideline for the investigation and management ofeosinophilia. Br J Haematol 176:553–572
Leru PM (2019) Eosinophilic disorders: evaluation of current classifcation and diagnostic criteria, proposal of a practical diagnostic algorithm. Clin Transl Allergy 9:36–45
Gotlib J (2017) World Health Organization-defined eosinophilic disorders: 2017 update on diagnosis, risk stratification, and management. Am J Hematol 92:1243–1259
Xiaohong C, Yiping XU, Meiping LU (2016) Clinical characteristics and etiology of children with hypereosinophilia. Zhejiang Da Xue Xue Bao Yi Xue Ban J Zhejiang Univ Sci 45:292–296
Çelik İK, Büyüktiryaki B, Açıkgöz FG et al (2021) Evaluation of Etiological Factors Causing Hypereosinophilia in Children. Turk J Pediatr Dis 15:373–378
Schwartz JT, Fulkerson PC (2018) An approach to the evaluation of persistent hypereosinophilia in pediatric patients. Front Immunol 9:1944
Brigden ML (1999) A practical workup for eosinophilia: you can investigate the most likely causes right in your office. Postgrad Med 105:193–210
Kovalszki A, Weller PF (2016) Eosinophilia. Prim Care 43:607–617
Kasap N, Celik V, Isik S et al (2021) A set of clinical and laboratory markers differentiates hyper-IgE syndrome from severe atopic dermatitis. Clin Immunol 223:108645
Navabi B, Upton JEM (2016) Primary immunodeficiencies associated with eosinophilia. Allergy Asthma Clin Immunol 12:1–12
Bergmann MM, Caubet J-C, Boguniewicz M, Eigenmann PA (2013) Evaluation of food allergy in patients with atopic dermatitis. J Allergy Clin Immunol Pract 1:22–28
Pilania RK, Chaudhary H, Jindal AK, Rawat A, Singh S (2020) Current status and prospects of primary immunodeficiency diseases in Asia. Genes Dis 7:3–11
Williams KW, Milner JD, Freeman AF (2015) Eosinophilia associated with disorders of immune deficiency or immune dysregulation. Immunol Allergy Clin North Am 35:523–544
Halken S, Muraro A, de Silva D et al (2021) EAACI guideline: Preventing the development of food allergy in infants and young children (2020 update). Pediatr Allergy Immunol 32:843–858
Davido B, de Truchis P, Dinh A (2019) Interest of Eosinophil Count in Bacterial Infections to Predict Antimicrobial Therapy Efficacy. JAMA Surg 154:464–464
Chusid MJ (1999) Eosinophilia in childhood. Immunol Allergy Clin North Am 19:327–346
Patel L, Garvey B, Arnon S, Roberts IA (1994) Eosinophilia in newborn infants Acta Pædiatr 83:797–801
López-Hurtado M, Arteaga-Troncoso G, Sosa-González IE, Haro-Cruz MJ, Flores-Salazar VR, Guerra-Infante FM (2016) Eosinophilia in Preterm Born Infants Infected with Chlamydia trachomatis. Fetal Pediatr Pathol 35:149–158
Da-Woon K, Myung-Geun S, Hyeong-Kee Y et al (2009) Incidence and causes of hypereosinophilia in the patients of a university hospital. Korean J Leg Med 29(3):185–193
Mehraj V, Hatcher J, Akhtar S, Rafique G, Beg MA (2008) Prevalence and factors associated with intestinal parasitic infection among children in an urban slum of Karachi. PLoS ONE 3:e3680
Bailey C, Lopez S, Camero A, Taiquiri C, Arhuay Y, Moore DAJ (2013) Factors associated with parasitic infection amongst street children in orphanages across Lima. Peru Pathog Glob Health 107:52–57
Acar M, Sutcu M, Umur O et al (2017) Acquired immune deficiency syndrome in differential diagnosis of hyper-ige-immunoglobulinemia: pediatric case report. J Trop Pediatr 63:82–84
Rezamand A, Ghorashi Z, Ghorashi S, Nezami N (2013) Eosinophilic presentation of acute lymphoblastic leukemia. Am J Case Rep 14:143–146
Wang SA (2019) The diagnostic work-up of hypereosinophilia. Pathobiology 86:39–52
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Pınar Gür Çetinkaya, Saliha Esenboga and Elif Soyak Aytekin. Data analysis was performed by Pınar Gür Çetinkaya and Ozge Soyer. The first draft of the manuscript was written by Pınar Gür Çetinkaya and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Hacettepe University School of Medicine (Date: 2021/Approval No: 2021/06-46).
Informed consent
Written informed consent was obtained from the parents of the children included in the study.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Communicated by Peter de Winter.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cetinkaya, P.G., Aytekin, E.S., Esenboga, S. et al. Eosinophilia in children: characteristics, etiology and diagnostic algorithm. Eur J Pediatr 182, 2833–2842 (2023). https://doi.org/10.1007/s00431-023-04961-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04961-x