Abstract
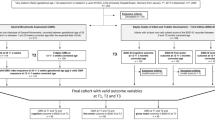
This study aimed to analyze spatiotemporal gait characteristics of preterm children from 3 to 4 years of age according to different gestational age groups and to examine the relationship between the detailed general movements assessment and spatiotemporal gait characteristics. A total of 74 preterm children, 32 extremely preterm and very preterm (EP-VP, < 32 weeks gestational age) and 42 moderate to late preterm (MLP, 32 to < 37 weeks gestational age), were included in this prospective study, along with 38 term children. Early spontaneous movements of preterm children were assessed from videos at 9–20 weeks post-term according to the general movements assessment, which determines the Motor Optimality Score-Revised (MOS-R). The spatiotemporal gait characteristics of all children were evaluated using the GAITRite®electronic walkway at self-selected walking speeds. EP-VP children walked with shorter step lengths (p = 0.039), and MLP children walked with greater step length variability (p = 0.003) than their term peers. The MOS-R results were related to step length (r = 0.36, p = 0.042), step length variability (r = −0.56, p = 0.001), and base of support (r = −0.37, p = 0.038) in EP-VP children. The MOS-R subcategories, age-adequate movement repertoire, and postural patterns were related to some of the spatiotemporal gait characteristics, including step length, step length variability, and base of support (p < 0.05).
Conclusion: EP-VP and MLP children might catch up to their term peers at 3 to 4 years of age in terms of most gait parameters. In addition to the MOS-R, age-adequate movement repertoire and postural patterns of preterm children without cerebral palsy in early life may be a marker of later neurodevelopmental dysfunction.
What is Known: |
• Preterm children walk with a wider step width, a greater step length asymmetry and step time, and a shorter stride length at 18 to 22 months of age compared with term children at a self-selected speed, while these differences disappear in children 4.5–5 years old and older. |
What is New: |
• Early spontaneous movements were related to some spatiotemporal gait characteristics. |
• Preterm children might catch up to term children at 3–4 years of age in spatiotemporal gait characteristics while walking at a self-selected speed. |


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request. The data are not publicly available due to privacy or ethical restrictions.
Abbreviations
- CP:
-
Cerebral palsy
- EP-VP:
-
Extremely preterm and very preterm
- GMA:
-
General movements assessment
- MLP:
-
Moderate to late preterm
- MOS:
-
Motor optimality score
- MOS-R:
-
Motor optimality score – revised
- VP:
-
Very preterm
References
Spittle AJ, Orton J (2014) Cerebral palsy and developmental coordination disorder in children born preterm. Semin Fetal Neonatal Med 19(2):84–9. https://doi.org/10.1016/j.siny.2013.11.005
Wood NS, Marlow N, Costeloe K, Gibson AT, Wilkinson AR (2000) Neurologic and developmental disability after extremely preterm birth. EPICure Study Group. N Engl J Med 343(6):378–84. https://doi.org/10.1056/NEJM200008103430601
Cheong JL, Doyle LW (2012) Increasing rates of prematurity and epidemiology of late preterm birth. J Paediatr Child Health 48(9):784–8. https://doi.org/10.1111/j.1440-1754.2012.02536.x
Blencowe H, Lee AC, Cousens S, Bahalim A, Narwal R, Zhong N, Chou D, Say L, Modi N, Katz J et al (2013) Preterm birth-associated neurodevelopmental impairment estimates at regional and global levels for 2010. Pediatr Res 74 Suppl 1(Suppl 1):17–34. https://doi.org/10.1038/pr.2013.204
Kerstjens JM, de Winter AF, Bocca-Tjeertes IF, Bos AF, Reijneveld SA (2012) Risk of developmental delay increases exponentially as gestational age of preterm infants decreases: a cohort study at age 4 years. Dev Med Child Neurol 54(12):1096–101. https://doi.org/10.1111/j.1469-8749.2012.04423.x
Williams J, Lee KJ, Anderson PJ (2010) Prevalence of motor-skill impairment in preterm children who do not develop cerebral palsy: a systematic review. Dev Med Child Neurol 52(3):232–7. https://doi.org/10.1111/j.1469-8749.2009.03544.x
Ferrari F, Gallo C, Pugliese M, Guidotti I, Gavioli S, Coccolini E, Zagni P, Della Casa E, Rossi C, Lugli L et al (2012) Preterm birth and developmental problems in the preschool age. Part I: minor motor problems. J Matern Fetal Neonatal Med 25(11):2154–9. https://doi.org/10.3109/14767058.2012.696164
Goyen TA, Lui K (2002) Longitudinal motor development of “apparently normal” high-risk infants at 18 months, 3 and 5 years. Early Hum Dev 70(1–2):103–15. https://doi.org/10.1016/s0378-3782(02)00094-4
Novak I, Morgan C, Adde L, Blackman J, Boyd RN, Brunstrom-Hernandez J, Cioni G, Damiano D, Darrah J, Eliasson AC et al (2017) Early, accurate diagnosis and early intervention in cerebral palsy: advances in diagnosis and treatment. JAMA Pediatr 171(9):897–907. https://doi.org/10.1001/jamapediatrics.2017.1689
Einspieler C, Prechtl HF, Bos AF, Ferrari F, Cioni G (2004) Prechtl’s method on the qualitative assessment of general movements in preterm, term and young infants, 1st edn. Mac Keith Press, London
Prechtl HF (1990) Qualitative changes of spontaneous movements in fetus and preterm infant are a marker of neurological dysfunction. Early Hum Dev 23(3):151–8. https://doi.org/10.1016/0378-3782(90)90011-7
Einspieler C, Prechtl HF (2005) Prechtl’s assessment of general movements: a diagnostic tool for the functional assessment of the young nervous system. Ment Retard Dev Disabil Res Rev 11(1):61–7. https://doi.org/10.1002/mrdd.20051
Einspieler C, Bos AF, Krieber-Tomantschger M, Alvarado E, Barbosa VM, Bertoncelli N, Burger M, Chorna O, Del Secco S, DeRegnier RA et al (2019) Cerebral palsy: early markers of clinical phenotype and functional outcome. J Clin Med 4;8(10):1616. https://doi.org/10.3390/jcm8101616
Kwong AK, Boyd RN, Chatfield MD, Ware RS, Colditz PB, George JM (2022) Early motor repertoire of very preterm infants and relationships with 2-year neurodevelopment. J Clin Med 11(7):1833. https://doi.org/10.3390/jcm11071833
Salavati S, Bos AF, Doyle LW, Anderson PJ, Spittle AJ (2021) Very preterm early motor repertoire and neurodevelopmental outcomes at 8 years. Pediatrics 148(3):e2020049572. https://doi.org/10.1542/peds.2020-049572
Bruggink JL, Einspieler C, Butcher PR, Stremmelaar EF, Prechtl HF, Bos AF (2009) Quantitative aspects of the early motor repertoire in preterm infants: do they predict minor neurological dysfunction at school age? Early Hum Dev 85(1):25–36. https://doi.org/10.1016/j.earlhumdev.2008.05.010
Dzeladini F, van den Kieboom J, Ijspeert A (2014) The contribution of a central pattern generator in a reflex-based neuromuscular model. Front Hum Neurosci 8:371. https://doi.org/10.3389/fnhum.2014.00371
Kraan CM, Tan AHJ, Cornish KM (2017) The developmental dynamics of gait maturation with a focus on spatiotemporal measures. Gait Posture 51:208–217. https://doi.org/10.1016/j.gaitpost.2016.10.021
WHO Multicentre Growth Reference Study Group (2006) WHO Motor Development Study: windows of achievement for six gross motor development milestones. Acta Paediatr Suppl 450:86–95. https://doi.org/10.1111/j.1651-2227.2006.tb02379.x
Sutherland DH, Olshen R, Cooper L, Woo SL (1980) The development of mature gait. J Bone Joint Surg Am 62(3):336–353. PMID: 7364807
Jeng SF, Liao HF, Lai JS, Hou JW (1997) Optimization of walking in children. Med Sci Sports Exerc 29(3):370–6. https://doi.org/10.1097/00005768-199703000-00012
Jeng SF, Lau TW, Hsieh WS, Luo HJ, Chen PS, Lin KH, Shieh JY (2008) Development of walking in preterm and term infants: age of onset, qualitative features and sensitivity to resonance. Gait Posture 27(2):340–6. https://doi.org/10.1016/j.gaitpost.2007.04.012
Campos JJ, Anderson DI, Barbu-Roth MA, Hubbard EM, Hertenstein MJ, Witherington D (2000) Travel broadens the mind. Infancy 1(2):149–219. https://doi.org/10.1207/S15327078IN0102_1
Albesher RA, Spittle AJ, McGinley JL, Dobson FL (2019) Gait characteristics of children born preterm. Neoreviews 20(7):e397-e408. https://doi.org/10.1542/neo.20-7-e397
Cahill-Rowley K, Rose J (2016) Temporal-spatial gait parameters and neurodevelopment in very-low-birth-weight preterm toddlers at 18–22 months. Gait Posture 45:83–9. https://doi.org/10.1016/j.gaitpost.2016.01.002
Albesher RA, Spittle AJ, Dobson FL, Mentiplay BF, FitzGerald TL, Cameron KL, Zannino D, Josev EK, Doyle LW, Cheong JLY et al (2022) Spatiotemporal gait variables and step-to-step variability in preschool-aged children born < 30 weeks’ gestation and at term in preferred speed, dual-task paradigm, and tandem walking. Gait Posture 92:236–242. https://doi.org/10.1016/j.gaitpost.2021.11.027
Kluenter H, Roedder D, Kribs A, Fricke O, Roth B, Guntinas-Lichius O (2008) Postural control at 7 years of age after preterm birth with very low birth weight. Otol Neurotol 29(8):1171–5. https://doi.org/10.1097/MAO.0b013e31818a0f5c
Hagmann-von Arx P, Manicolo O, Perkinson-Gloor N, Weber P, Grob A, Lemola S (2015) Gait in very preterm school-aged children in dual-task paradigms. PLoS One 10(12):e0144363. https://doi.org/10.1371/journal.pone.0144363
Örtqvist M, Einspieler C, Marschik PB, Ådén U (2021) Movements and posture in infants born extremely preterm in comparison to term-born controls. Early Hum Dev 154:105304. https://doi.org/10.1016/j.earlhumdev.2020.105304
Zang FF, Yang H, Han Q, Cao JY, Tomantschger I, Krieber M, Shi W, Luo DD, Zhu M, Einspieler C (2016) Very low birth weight infants in China: the predictive value of the motor repertoire at 3 to 5months for the motor performance at 12months. Early Hum Dev 100:27–32. https://doi.org/10.1016/j.earlhumdev.2016.03.010
Fjørtoft T, Einspieler C, Adde L, Strand LI (2009) Inter-observer reliability of the “Assessment of Motor Repertoire--3 to 5 Months” based on video recordings of infants. Early Hum Dev 85(5):297–302. https://doi.org/10.1016/j.earlhumdev.2008.12.001
Webster KE, Wittwer JE, Feller JA (2005) Validity of the GAITRite walkway system for the measurement of averaged and individual step parameters of gait. Gait Posture 22(4):317–21. https://doi.org/10.1016/j.gaitpost.2004.10.005
Thorpe DE, Dusing SC, Moore CG (2005) Repeatability of temporospatial gait measures in children using the GAITRite electronic walkway. Arch Phys Med Rehabi 86(12):2342–6. https://doi.org/10.1016/j.apmr.2005.07.301
Wondra VC, Pitetti KH, Beets MW (2007) Gait parameters in children with motor disabilities using an electronic walkway system: assessment of reliability. Pediatr Phys Ther 19(4):326–31. https://doi.org/10.1097/PEP.0b013e3181577d6d
Sutherland D (1997) The development of mature gait. Gait Posture 6(2):163–170. https://doi.org/10.1016/S0966-6362(97)00029-5
Holm S (1979) A simple sequentially rejective multiple test procedure. Scand J Stat 6(2):65–70
Asuero AG, Sayago A, González A (2006) The correlation coefficient: an overview. Crit Rev Anal Chem 36(1):41–59. https://doi.org/10.1080/10408340500526766
Ito Y, Ito T, Sugiura H, Kidokoro H, Sugiyama Y, Mizusawa J, Natsume J, Noritake K, Kato Y, Ochi N (2021) Physical functions and gait performance in school-aged children born late preterm. Early Hum Dev 163:105478. https://doi.org/10.1016/j.earlhumdev.2021.105478
Brown L, Burns YR, Watter P, Gibbons KS, Gray PH (2015) Motor performance, postural stability and behaviour of non-disabled extremely preterm or extremely low birth weight children at four to five years of age. Early Hum Dev 91(5):309–15. https://doi.org/10.1016/j.earlhumdev.2015.03.003
Ivanenko YP, Poppele RE, Lacquaniti F (2006) Motor control programs and walking. Neuroscientist12(4):339–48. https://doi.org/10.1177/1073858406287987.
Fjørtoft T, Grunewaldt KH, Løhaugen GC, Mørkved S, Skranes J, Evensen KA (2013) Assessment of motor behaviour in high-risk-infants at 3 months predicts motor and cognitive outcomes in 10 years old children. Early Hum Dev 89(10):787–93. https://doi.org/10.1016/j.earlhumdev.2013.06.007
Kwong AKL, Doyle LW, Olsen JE, Eeles AL, Lee KJ, Cheong JLY, Spittle AJ (2022) Early motor repertoire and neurodevelopment at 2 years in infants born extremely preterm or extremely-low-birthweight. Dev Med Child Neurol 64(7):855–862. https://doi.org/10.1111/dmcn.15167
Peyton C, Einspieler C, Fjørtoft T, Adde L, Schreiber MD, Drobyshevsky A, Marks JD (2020) Correlates of normal and abnormal general movements in infancy and long-term neurodevelopment of preterm infants: insights from functional connectivity studies at term equivalence. J Clin Med 9(3):834. https://doi.org/10.3390/jcm9030834
Pollock AS, Durward BR, Rowe PJ, Paul JP (2000) What is balance? Clin Rehabil 14(4):402–6. https://doi.org/10.1191/0269215500cr342oa
Hallemans A, De Clercq D, Aerts P (2006) Changes in 3D joint dynamics during the first 5 months after the onset of independent walking: a longitudinal follow-up study. Gait Posture 24(3):270–9. https://doi.org/10.1016/j.gaitpost.2005.10.003
Sato H, Nomura Y, Kamide K (2022) Relationship between static balance and gait parameters in preschool children. Gait Posture 96:143–148. https://doi.org/10.1016/j.gaitpost.2022.05.029
Fallang B, Saugstad OD, Hadders-Algra M (2003) Postural adjustments in preterm infants at 4 and 6 months post-term during voluntary reaching in supine position. Pediatr Res 54(6):826–33. https://doi.org/10.1203/01.PDR.0000088072.64794.F3
Fallang B, Øien I, Hellem E, Saugstad OD, Hadders-Algra M (2005) Quality of reaching and postural control in young preterm infants is related to neuromotor outcome at 6 years. Pediatr Res 58(2):347–53. https://doi.org/10.1203/01.PDR.0000170898.60160.09
Fallang B, Hadders-Algra M (2005) Postural behavior in children born preterm. Neural Plast 12(2–3):175–82; discussion 263–72. https://doi.org/10.1155/np.2005.175
Bucci MP, Tringali M, Trousson C, Husson I, Baud O, Biran V (2017) Spatial and temporal postural analysis in children born prematurely. Gait Posture 57:230–235. https://doi.org/10.1016/j.gaitpost.2017.06.023
Acknowledgements
The authors would like to thank the children and parents who participated in the study.
Author information
Authors and Affiliations
Contributions
Yusuf Topal and Bilge Nur Yardımcı-Lokmanoğlu conceived and designed the study, analyzed and interpreted the data, and drafted and revised the manuscript; Semra Topuz and Akmer Mutlu assisted with the overall study design and implementation, interpreted the results, and reviewed and revised the manuscript; all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Non-Interventional Clinical Research Ethics Board, Hacettepe University (GO 21/1006). The study protocol was in accordance with the Declaration of Helsinki. All parents gave written informed consent before the study.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Gregorio Milani.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Topal, Y., Yardımcı-Lokmanoğlu, B.N., Topuz, S. et al. Early spontaneous movements and spatiotemporal gait characteristics in preterm children. Eur J Pediatr 182, 2913–2923 (2023). https://doi.org/10.1007/s00431-023-04949-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04949-7