Abstract
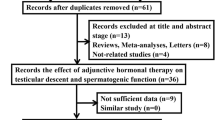
Congenital cryptorchidism is a well-established risk factor of testicular malignancies. However, there is still remarkable variability in the measures of associations between of these two clinical entities. The current meta-analysis investigates the up-to-date risk of testicular cancer in adults with a history of surgically corrected congenital cryptorchidism until adolescence. The meta-analysis was conducted with strict criteria for the identification of the congenital cryptorchidism cases that underwent surgery before adulthood. The study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A search of the PubMed and the Scopus databases was conducted, using a defined strategy, from inception to February 2023. Two independent authors screened the literature and extracted the data, using inclusion and exclusion criteria. Of the 2176 articles identified, 93 articles were fully retrieved, and 6 articles met all the inclusion criteria. The Newcastle–Ottawa scale was applied for the studies’ quality assessment. The random-effects model in RevMan 5.4 program was used for the meta-analysis. Three case–control studies and three cohort studies were selected. They included 371,681 patients and 1786 incidents of testicular cancer. The pooled odds ratio (OR) was 3.99 (95% confidence intervals (CI): 2.80–5.71). The heterogeneity was moderate and estimated at 51% with the I-squared statistic. A forest plot and a funnel plot were produced to evaluate the ORs and the probable publication bias, respectively. The mean Newcastle–Ottawa score was 8/9 for all the included reports.
Conclusion: This systematic review and meta-analysis verifies, with an updated estimate, the increased risk of testicular cancer in adults with an orchidopexy history. New evidence on the maldescent laterality supports that the cancer risk remains increased and for the contralateral, unaffected testicle, although to a lesser extent. The orchidopexy in the first year of life prevents the testicular damage and decreases the overall cancer risk.
What is Known: |
• Congenital cryptorchidism is the commonest genitourinary abnormality and a risk factor for testicular cancer. |
• The most recent meta-analysis reporting this association was in 2013. |
What is New: |
• After reviewing literature until February 2023, the association of congenital cryptorchidism with testicular cancer risk in adulthood was verified: odds ratio=3.99 [2.80–5.71], 95% CI. |
• The meta-analysis highlights the protective role of early orchidopexy and the controversial data about maldescent and testicular cancer laterality. |


Similar content being viewed by others
Data availability
Data available upon request.
Abbreviations
- CI:
-
Confidence intervals
- hCG:
-
Human chorionic gonadotropin
- HIV:
-
Human immunodeficiency virus
- ICD:
-
International Classification of Diseases
- MeSH:
-
Medical Subject Headings
- NOS:
-
Newcastle Ottawa Scale
- OR:
-
Odds ratio
- RR:
-
Risk ratio
- SD:
-
Standard deviation
References
Kim SO, Hwang EC, Hwang IS, Oh KJ, Jung SI, Kang TW, Kwon D, Park K, Bang-Ryu S (2011) Testicular catch-up growth: the impact of orchiopexy age. Urology 78(4):886–889. https://doi.org/10.1016/j.urology.2011.04.057
Lip SZ, Murchison LE, Cullis PS, Govan L, Carachi R (2013) A meta-analysis of the risk of boys with isolated cryptorchidism developing testicular cancer in later life. Arch Dis Child 98(1):20–26. https://doi.org/10.1136/archdischild-2012-302051
Kolon TF, Herndon CD, Baker LA, Baskin LS, Baxter CG, Cheng EY, Diaz M, Lee PA, Seashore CJ, Tasian GE, Barthold JS (2014) American Urological Association. (2014) Evaluation and treatment of cryptorchidism: AUA guideline. J Urol 192(2):337–45. https://doi.org/10.1016/j.juro.2014.05.005
Hutson JM, Thorup J (2015) Evaluation and management of the infant with cryptorchidism. Curr Opin Pediatr 27(4):520–524. https://doi.org/10.1097/MOP.0000000000000237
Loebenstein M, Thorup J, Cortes D, Clasen-Linde E, Hutson JM, Li R (2020) Cryptorchidism, gonocyte development, and the risks of germ cell malignancy and infertility: a systematic review. J Pediatr Surg 55(7):1201–1210. https://doi.org/10.1016/j.jpedsurg.2019.06.023
Feyles F, Peiretti V, Mussa A, Manenti M, Canavese F, Cortese MG, Lala R (2014) (2014) Improved sperm count and motility in young men surgically treated for cryptorchidism in the first year of life. Eur J Pediatr Surg 24(5):376–380. https://doi.org/10.1055/s-0033-1349715
Hensel KO, Caspers T, Jenke AC, Schuler E, Wirth S (2015) Operative management of cryptorchidism: guidelines and reality--a 10-year observational analysis of 3587 cases. BMC Pediatr 15:116. https://doi.org/10.1186/s12887-015-0429-1
Hack WW, Meijer RW, Van Der Voort-Doedens LM, Bos SD, De Kok ME (2003) (2003) Previous testicular position in boys referred for an undescended testis: further explanation of the late orchidopexy enigma? BJU Int 92(3):293–296. https://doi.org/10.1046/j.1464-410x.2003.04317.x
Wei Y, Wu SD, Wang YC, Lin T, He DW, Li XL, Liu JH, Liu X, Hua Y, Lu P, Zhang DY, Wen S, Wei GH (2016) A 22-year retrospective study: educational update and new referral pattern of age at orchidopexy. BJUInt 118(6):987–993. https://doi.org/10.1111/bju.13588
Dieckmann KP, Pichlmeier U (2004) Clinical epidemiology of testicular germ cell tumors. World J Urol 22:2–14. https://doi.org/10.1007/s00345-004-0398-8
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100. https://doi.org/10.1371/journal.pmed.1000100
Higgins JPT, Green S (editors) (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Cochrane Collab
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605. https://doi.org/10.1007/s10654-010-9491-z
Review Manager (RevMan) [Computer program] (2020) Version 5.4. Cochrane Collab
Schneuer FJ, Milne E, Jamieson SE, Pereira G, Hansen M, Barker A, Holland AJA, Bower C, Nassar N (2018) Association between male genital anomalies and adult male reproductive disorders: a population-based data linkage study spanning more than 40 years. Lancet Child Adolesc Health 2(10):736–743. https://doi.org/10.1016/S2352-4642(18)30254-2
Pettersson A, Richiardi L, Nordenskjold A, Kaijser M, Akre O (2007) Age at surgery for undescended testis and risk of testicular cancer. N Engl J Med 356(18):1835–1841. https://doi.org/10.1056/NEJMoa067588
Prener A, Engholm G, Jensen OM (1996) Genital anomalies and risk for testicular cancer in Danish men. Epidemiology 7(1):14–9. https://doi.org/10.1097/00001648-199601000-00004
Forman D, Pike MC, Davey G, Dawson S, Baker K, Chilvers CE et al (1994) Aetiology of testicular cancer: association with congenital abnormalities, age at puberty, infertility, and exercise BMJ 308:1393. https://doi.org/10.1136/bmj.308.6941.1393
Strader CH, Weiss NS, Daling JR, Karagas MR, McKnight B (1988) Cryptorchism, orchiopexy, and the risk of testicular cancer. Am J Epidemiol 127(5):1013–1018. https://doi.org/10.1093/oxfordjournals.aje.a114877
Swerdlow AJ, Huttly SR, Smith PG (1987) Testicular cancer and antecedent diseases. Br J Cancer 55(1):97–103. https://doi.org/10.1038/bjc.1987.20
Cook MB, Akre O, Forman D, Madigan MP, Richiardi L, McGlynn KA (2010) A systematic review and meta-analysis of perinatal variables in relation to the risk of testicular cancer–experiences of the son. Int J Epidemiol 39(6):1605–1618. https://doi.org/10.1093/ije/dyq120
Walsh TJ, Dall'Era MA, Croughan MS, Carroll PR, Turek PJ (2007) Prepubertal orchiopexy for cryptorchidism may be associated with lower risk of testicular cancer. J Urol 178(4 Pt 1):1440–6; discussion 1446. https://doi.org/10.1016/j.juro.2007.05.166
Baird DC, Meyers GJ, Hu JS (2018) Testicular cancer: diagnosis and treatment. Am Fam Physician 97(4):261–268
Skakkebaek NE, Rajpert-De Meyts E, Main KM (2001) Testicular dysgenesis syndrome: an increasingly common develop- mental disorder with environmental aspects. Hum Reprod 16:972. https://doi.org/10.1093/humrep/16.5.972
Akre O, Pettersson A, Richiardi L (2009) Risk of contralateral testicular cancer among men with unilaterally undescended testis: a meta analysis. Int J Cancer 124(3):687–689. https://doi.org/10.1002/ijc.23936
Wood HM, Elder JS (2009) Cryptorchidism and testicular cancer: separating fact from fiction. J Urol 181(2):452–461. https://doi.org/10.1016/j.juro.2008.10.074
Banks K, Tuazon E, Berhane K, Koh CJ, De Filippo RE, Chang A, Kim SS, Daneshmand S, Davis-Dao C, Lewinger JP, Bernstein L, Cortessis VK (2013) Cryptorchidism and testicular germ cell tumors: comprehensive meta-analysis reveals that association between these conditions diminished over time and is modified by clinical characteristics. Front Endocrinol (Lausanne) 18(3):182. https://doi.org/10.3389/fendo.2012.00182
Ritzén EM, Bergh A, Bjerknes R, Christiansen P, Cortes D, Haugen SE, Jörgensen N, Kollin C, Lindahl S, Läckgren G, Main KM, Nordenskjöld A, Rajpert-De Meyts E, Söder O, Taskinen S, Thorsson A, Thorup J, Toppari J, Virtanen H (2007) Nordic consensus on treatment of undescended testes. Acta Paediatr 96(5):638–643. https://doi.org/10.1111/j.1651-2227.2006.00159.x
Radmayr C, Dogan HS, Hoebeke P, Kocvara R, Nijman R, Silay S, Stein R, Undre S, Tekgul S (2016) Management of undescended testes: European Association of Urology/European Society for Paediatric Urology Guidelines. J Pediatr Urol 12(6):335–343. https://doi.org/10.1016/j.jpurol.2016.07.014
Allin BSR, Dumann E, Fawkner-Corbett D, Kwok C, Skerritt C (2018) Paediatric Surgery Trainees Research Network. Systematic review and meta-analysis comparing outcomes following orchidopexy for cryptorchidism before or after 1 year of age. BJS Open 2(1):1–12. https://doi.org/10.1002/bjs5.36
Dawson DV, Pihlstrom BL, Blanchette DR (2016) Understanding and evaluating meta-analysis. J Am Dent Assoc 147(4):264–270. https://doi.org/10.1016/j.adaj.2015.10.023
Khan S, Memon B, Memon MA (2019) Meta-analysis: a critical appraisal of the methodology, benefits and drawbacks. Br J Hosp Med (Lond) 80(11):636–641. https://doi.org/10.12968/hmed.2019.80.11.636
Author information
Authors and Affiliations
Contributions
Study concept and design: Maria Florou, Evangelia Ntzani, Christos Kaselas. Acquisition of data: Maria Florou, Christos Kaselas. Analysis and interpretation of data: Maria Florou, Evangelia Ntzani, Ekaterini Siomou, Triantafyllia Koletsa. Drafting of the manuscript: Maria Florou. Statistical analysis: Maria Florou, Konstantinos Tsilidis, Evangelia Ntzani. Prepared figures and tables: Ekaterini Siomou, Ioannis Spyridakis, Antonia Syrnioti. All authors reviewed the manuscript. Supervision: Christos Kaselas, Evangelia Ntzani.
Corresponding author
Ethics declarations
Ethics approval
This is a systematic review and meta-analysis of observational studies. No ethics approval is required.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Gregorio Milani.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Florou, M., Tsilidis, K.K., Siomou, E. et al. Orchidopexy for congenital cryptorchidism in childhood and adolescence and testicular cancer in adults: an updated systematic review and meta-analysis of observational studies. Eur J Pediatr 182, 2499–2507 (2023). https://doi.org/10.1007/s00431-023-04947-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04947-9