Abstract
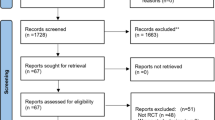
We conducted a systematic review and meta-analysis to examine the efficacy profiles of metronidazole (MNZ) and vancomycin (VCM) in pediatric and adolescent patients with Clostridioides difficile infection (CDI). A systematic review and meta-analysis was conducted using four electronic databases (PubMed, Cochrane Library, Web of Science, and Clinicaltrials.gov) through July 6, 2022. We analyzed the clinical cure and recurrence rates to determine the efficacy of MNZ and VCM. The clinical cure rates in all included studies were not significantly different between MNZ and VCM (OR = 0.63; 95% CI = 0.36–1.10; I2 = 0%; P = 0.10). Subgroup analyses were performed separately for each region to account for regional differences in the CDI. MNZ treatment achieved significantly lower clinical cure rates than did VCM in the United States of America (USA) and Europe (OR = 0.42, 95% CI = 0.19–0.93, I2 = 0%, P = 0.03). Recurrence rates were not significantly different between MNZ and VCM (OR = 1.48, 95% CI = 0.62–3.53, I2 = 28%, P = 0.38).
Conclusion: MNZ exhibited significantly lower clinical cure rates than did VCM in the US and Europe; therefore, it is not recommended for the management of CDI in pediatric and adolescent populations.
What is Known: • The unavailability of robust data on recommendations of therapeutic agents for the management of Clostridioides difficile infections in children precludes effective antibiotic choice. | |
What is New: • Metronidazole exhibited significantly lower clinical cure rates than did vancomycin in the United States of America and Europe and recurrence rate was not significantly different between metronidazole and vancomycin; therefore, it is not recommended for the management of Clostridioides difficile infection in children. |


Similar content being viewed by others
Data availability
The datasets generated or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CDI:
-
Clostridioides difficile Infection
- CIs:
-
Confidence intervals
- FDX:
-
Fidaxomicin
- MNZ:
-
Metronidazole
- ORs:
-
Odd ratios
- RCTs:
-
Randomized controlled trials
- VCM:
-
Vancomycin
References
Johnson S, Lavergne V, Skinner AM, Gonzales-Luna AJ, Garey KW, Kelly CP et al (2021) Clinical practice guideline by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA): 2021 focused update guidelines on management of Clostridioides difficile infection in adults. Clin Infect Dis 73:e1029–e1044. https://doi.org/10.1093/cid/ciab549
van Prehn J, Reigadas E, Vogelzang EH, Bouza E, Hristea A, Guery B et al (2021) European Society of Clinical Microbiology and Infectious Diseases: 2021 update on the treatment guidance document for Clostridioides difficile infection in adults. Clin Microbiol Infect 27:S1–S21. https://doi.org/10.1016/j.cmi.2021.09.038
Johnson S, Louie TJ, Gerding DN, Cornely OA, Chasan-Taber S, Fitts D et al (2014) Vancomycin, metronidazole, or tolevamer for Clostridium difficile infection: Results from two multinational, randomized, controlled trials. Clin Infect Dis 59:345–354. https://doi.org/10.1093/cid/ciu313
Krutova M, de Meij TGJ, Fitzpatrick F, Drew RJ, Wilcox MH, Kuijper EJ (2022) How to: Clostridioides difficile infection in children. Clin Microbiol Infect 28:1085–1090. https://doi.org/10.1016/j.cmi.2022.03.001
McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE et al (2018) Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis 66:987–994. https://doi.org/10.1093/cid/ciy149
Wolf J, Kalocsai K, Fortuny C, Lazar S, Bosis S, Korczowski B et al (2020) Safety and efficacy of fidaxomicin and vancomycin in children and adolescents with Clostridioides (Clostridium) difficile infection: A phase 3, multicenter, randomized, single-blind clinical trial (SUNSHINE). Clin Infect Dis 71:2581–2588. https://doi.org/10.1093/cid/ciz1149
Louie TJ, Miller MA, Mullane KM, Weiss K, Lentnek A, Golan Y et al (2011) Fidaxomicin versus vancomycin for Clostridium difficile infection. N Engl J Med 364:422–431. https://doi.org/10.1056/NEJMoa0910812
Cornely OA, Crook DW, Esposito R, Poirier A, Somero MS, Weiss K et al (2012) Fidaxomicin versus vancomycin for infection with Clostridium difficile in Europe, Canada, and the USA: A double-blind, non-inferiority, randomised controlled trial. Lancet Infect Dis 12:281–289. https://doi.org/10.1016/S1473-3099(11)70374-7
Kunishima H, Ohge H, Suzuki H, Nakamura A, Matsumoto K, Mikamo H et al (2021) Japanese Clinical practice guidelines for management of Clostridioides (Clostridium) difficile infection. J Infect Chemother 28:1045–1083. https://doi.org/10.1016/j.jiac.2021.12.011
Baker SS, Faden H, Sayej W, Patel R, Baker RD (2010) Increasing incidence of community-associated atypical Clostridium difficile disease in children. Clin Pediatr (Phila) 49:644–647. https://doi.org/10.1177/0009922809360927
Khanna S, Baddour LM, Huskins WC, Kammer PP, Faubion WA, Zinsmeister AR et al (2013) The epidemiology of Clostridium difficile infection in children: A population-based study. Clin Infect Dis 56:1401–1406. https://doi.org/10.1093/cid/cit075
Lo Vecchio A, Lancella L, Tagliabue C, De Giacomo C, Garazzino S, Mainetti M et al (2017) Clostridium difficile infection in children: Epidemiology and risk of recurrence in a low-prevalence country. Eur J Clin Microbiol Infect Dis 36:177–185. https://doi.org/10.1007/s10096-016-2793-7
Parmar D, Dang R, Miranda-Katz M, Alabaster A, Greenhow TL (2019) Risk factors for recurrent community-associated Clostridiodes difficile infection in children. Pediatr Infect Dis J 38:1073–1078. https://doi.org/10.1097/INF.0000000000002439
Yin J, Kociolek LK, Same RG, Hsu AJ, Amoah J, Tamma PD. (2019) Oral vancomycin may be associated with earlier symptom resolution than metronidazole for hospitalized children with nonsevere Clostridiodes difficile infections. Open Forum Infect Dis 6:ofz492. https://doi.org/10.1093/ofid/ofz492
Duclaux-Loras R, Berthiller J, Ferroni A, Chardot C, Goulet O, Lacaille F et al (2020) Clostridium difficile: A frequent infection in children after intestinal transplantation. Transplantation 104:197–200. https://doi.org/10.1097/TP.0000000000002795
Li X, Xiao F, Li Y, Hu H, Xiao Y, Xu Q et al. (2022) Characteristics and management of children with Clostridiodes difficile infection at a tertiary pediatric hospital in China. Brazilian J Infect Dis 26:102380. https://doi.org/10.1016/j.bjid.2022.102380
Gonzales M, Pepin J, Frost EH, Carrier JC, Sirard S, Fortier LC et al (2010) Faecal pharmacokinetics of orally administered vancomycin in patients with suspected Clostridium difficile infection. BMC Infect Dis 10:363. https://doi.org/10.1186/1471-2334-10-363
Pepin J (2008) Vancomycin for the treatment of Clostridium difficile infection: For whom is this expensive bullet really magic? Clin Infect Dis 46:1493–1498. https://doi.org/10.1086/587656
Bolton RP, Culshaw MA (1986) Faecal metronidazole concentrations during oral and intravenous therapy for antibiotic associated colitis due to Clostridium difficile. Gut 27:1169–1172. https://doi.org/10.1136/gut.27.10.1169
Czepiel J, Pituch H, Kuijper EJ, Perucki W, Mielimonka A (2019) Clostridium difficile infection: Review. Eur J Clin Microbiol Infect Dis 38:1211–1221. https://doi.org/10.1007/s10096-019-03539-6
Eglow R, Pothoulakis C, Itzkowitz S, Israel EJ, O’Keane CJ, Gong O et al (1992) Diminished Clostridium difficile toxin a sensitivity in newborn rabbit ileum is associated with decreased toxin a receptor. J Clin Invest 90:822–829. https://doi.org/10.1172/JCI115957
Van Dorp SM, Smajlovic E, Knetsch CW, Notermans DW, De Greeff SC, Kuijper EJ (2017) Clinical and microbiological characteristics of Clostridium difficile infection among hospitalized children in the Netherlands. Clin Infect Dis 64:192–198. https://doi.org/10.1093/cid/ciw699
Acknowledgements
Sho Tashiro wishes to thank the Nagai Memorial Research Scholarship of the Pharmaceutical Society of Japan and JST SPRING (Grant Number JPMJSP2123). The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of this study. Material preparation, data collection, and analyses were performed by Sho Tashiro, Takayuki Mihara, Rikiya Okawa, Yoko Tanaka, and Yuki Enoki. The first draft of the manuscript was written by Sho Tashiro and Yuki Enoki, and all authors commented on previous versions of the manuscript. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Kazuaki Matsumoto received grant support funding from Meiji Seika Pharma Co., Ltd., Sumitomo Pharma Co., Ltd., and Shionogi & Co., Ltd., and speaker honoraria from Meiji Seika Pharma Co., Ltd. Yuka Yamagishi received speaker honoraria from MSD K.K. The authors declare no conflicts of interest.
Additional information
Communicated by Tobias Tenenbaum.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tashiro, S., Mihara, T., Okawa, R. et al. Optimal therapeutic recommendation for Clostridioides difficile infection in pediatric and adolescent populations: a systematic review and meta-analysis. Eur J Pediatr 182, 2673–2681 (2023). https://doi.org/10.1007/s00431-023-04944-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04944-y