Abstract
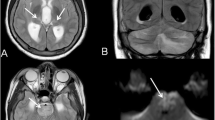
Influenza virus is generally characterized by fever, myalgia, and respiratory symptoms. Neurological entities have already been described, such as acute necrotizing encephalitis (ANE). We aimed to highlight the non-exceptional nature and explore the clinical spectrum and evolution of neurological features related to influenza virus in children. This monocentric observational study included patients under 18 years old, positive for influenza virus, between January 2017 and April 2019 in a pediatric university hospital. Patients were classified into two groups: those with or without a previous significant neurological or metabolic disorder. Two hundred eighty-nine children were identified with influenza infection. Thirty seven had a neurological manifestation: 14 patients who had previous significant neurological or metabolic disorder and 23 patients with no medical history. We identified several clinical patterns: 22 patients had seizures, 7 behavior disorders, 5 disturbances of consciousness, and 3 motor deficits. Four were diagnosed with a known influenza-associated neurological syndrome: 1 ANE, 1 cytotoxic lesion of the corpus callosum, 1 hemiconvulsion-hemiplegia-epilepsia syndrome, and 1 recurrent encephalitis in the context of a RANBP2 mutation. The neurological outcome was favorable in most cases. None of the patients with previous significant disorder retained sequalae or had a recurrence. Two patients had a fatal outcome, and both had a predisposing disorder.
Conclusion: Various neurological manifestations can be associated with influenza virus. Certain entities led to a poor prognosis, but in most cases, symptoms improved within a few days. The severity of the neurological manifestations correlated with previous neurological or metabolic disorders.
What is Known: • Influenza viruses are well known pathogens with a seasonal epidemic evolution, particularly affecting children. These viruses cause acute fever with respiratory symptoms, associated with myalgia and headaches. Neurological presentation in influenza‐virus infection is a well‐established possibility as influenza virus is considered to be responsible for 27 to 36% of childhood encephalitis. Some specific and severe entity as acute necrotizing encephalitis, cytotoxic lesion of the corpus callosum, or Hemiconvulsion‐hemiplegia‐epilepsy syndrome are well described. | |
What is New: • In a French monocentric cohort of 37 children with influenza‐related neurologic manifestations, the majority of these manifestations, including seizure, drowsiness, motor deficiency, hallucination… are self limiting and do not lead to after‐effects. In rare cases (4/37), they may reveal severe encephalitis requiring rapid and appropriate treatment. Otherwise, comparison of a group of 14 children with underlying neurological or metabolic disorder with a group of 23 children free of any significant disorder show that the severity of the neurological manifestations was largely related to previous neurological or metabolic disorders highlighting the importance of vaccination in this population. |



Similar content being viewed by others
Data availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Abbreviations
- ANE:
-
Acute necrotizing encephalitis
- CLOCCs:
-
Cytotoxic lesion of the corpus callosum
- HHE:
-
Hemiconvulsion-hemiplegia-epilepsy syndrome
- IAE:
-
Influenza-associated encephalopathy/encephalitis
References s
Labella AM, Merel SE (2013) Influenza. Med Clin North Am 97(4):621–45. https://pubmed.ncbi.nlm.nih.gov/23809717/
InVs bulletin hebdomadaire 17/04/2019. https://www.santepubliquefrance.fr/revues/beh/bulletin-epidemiologique-hebdomadaire
Kuiken T, Taubenberger JK (2008) Pathology of human influenza revisited. Vaccine 26:D59–66. https://pubmed.ncbi.nlm.nih.gov/19230162/
Mamas MA, Fraser D, Neyses L (2008) Cardiovascular manifestations associated with influenza virus infection. Int J Cardiol 130(3):304–9. https://pubmed.ncbi.nlm.nih.gov/18625525/
Jeliffe S (1918) Nervous and mental disturbances of influenza. N Y Med J 108:725–8.
Okabe N, Yamashita K, Inouye KT (2000) Influenza surveillance system of Japan and acute encephalitis and encephalopathy in the influenza season. Pediatr Int 42(2):187–91. https://pubmed.ncbi.nlm.nih.gov/10804740/
Hoshino A, Saitoh M, Oka A, Okumura A, Kubota M, Saito Y et al (2012) Epidemiology of acute encephalopathy in Japan, with emphasis on the association of viruses and syndromes. Brain Dev 34(5):337–43. https://pubmed.ncbi.nlm.nih.gov/21924570/
Britton PN, Dale RC, Blyth CC, Macartney K, Crawford NW, Marshall H et al (2017) Influenza-associated encephalitis/encephalopathy identified by the Australian childhood encephalitis study 2013–2015. Pediatr Infect Dis J 36(11):1021–6. https://pubmed.ncbi.nlm.nih.gov/28654561/
Maricich SM, Neul JL, Lotze TE, Cazacu AC, Uyeki TM, Demmler GJ et al (2004) Neurologic complications associated with influenza A in children during the 2003–2004 influenza season in Houston, Texas. Pediatrics 114(5):e626–33. https://reference.medscape.com/medline/abstract/15520093
Goenka A, Michael BD, Ledger E, Hart IJ, Absoud M, Chow G et al (2014) Neurological manifestations of influenza infection in children and adults: results of a National British Surveillance Study. Clinical Infectious Diseases: An Official Publication Of The Infectious Diseases Society Of America 58(6):775–84. https://pubmed.ncbi.nlm.nih.gov/24352349/
Wang K, Carver T, Tonner S, Semple MG, Hay AD, Moore M et al (2018) Early use of antibiotics for at risk children with influenza (ARCHIE): protocol for a double-blind, randomised, placebo-controlled trial. BMJ Open 8(5):e021144. https://pubmed.ncbi.nlm.nih.gov/29769256/
Mizuguchi M, Abe J, Mikkaichi K, Noma S, Yoshida K, Yamanaka T et al (1995) Acute necrotising encephalopathy of childhood: a new syndrome presenting with multifocal, symmetric brain lesions. J Neurol Neurosurg Psychiatr 58(5):555–61. https://pubmed.ncbi.nlm.nih.gov/7745402/
Mizuguchi M (1997) Acute necrotizing encephalopathy of childhood: a novel form of acute encephalopathy prevalent in Japan and Taiwan. Brain Dev 19(2):81–92. https://pubmed.ncbi.nlm.nih.gov/9105653/
Mizuguchi M, Yamanouchi H, Ichiyama T, Shiomi M (2007) Acute encephalopathy associated with influenza and other viral infections. Acta Neurologica Scandinavica Supplementum 115:45–56. https://pubmed.ncbi.nlm.nih.gov/17784537/
Protheroe SM, Mellor DH (1991) Imaging in influenza A encephalitis. Arch Dis Child 66(6):702–5. https://pubmed.ncbi.nlm.nih.gov/2053792/
Ka A, Britton P, Troedson C, Webster R, Procopis P, Ging J et al (2015) Mild encephalopathy with reversible splenial lesion: an important differential of encephalitis. Eur J Paediatr Neurol 19(3):377–82. https://pubmed.ncbi.nlm.nih.gov/25707871/
Gastaut H, Poirier F, Payan H, Salamon G, Toga M, Vigouroux M (1959) HHE syndrome hemiconvulsions, hemiplegia, epilepsy. Epilepsia 1(1–5):418–47. https://pubmed.ncbi.nlm.nih.gov/13826801/
Auvin S, Bellavoine V, Merdariu D, Delanoë C, Elmaleh-Bergés M, Gressens P et al (2012) Hemiconvulsion–hemiplegia–epilepsy syndrome: current understandings. Eur J Paediatr Neurol 16(5):413–21. https://pubmed.ncbi.nlm.nih.gov/22341151/
Toovey S (2008) Influenza-associated central nervous system dysfunction: a literature review. Travel Med Infect Dis 6(3):114–24. https://pubmed.ncbi.nlm.nih.gov/18486065/
Garcelon N, Neuraz A, Salomon R, Faour H, Benoit V, Delapalme A et al (2018) A clinician friendly data warehouse oriented toward narrative reports: Dr. Warehouse. J Biomed Inform 80:52–63. https://pubmed.ncbi.nlm.nih.gov/29501921/
Gu Y, Shimada T, Yasui Y, Tada Y, Kaku M, Okabe N (2013) National surveillance of influenza-associated encephalopathy in Japan over six years, before and during the 2009–2010 influenza pandemic. PLoS ONE 8(1):e54786. https://pubmed.ncbi.nlm.nih.gov/23355899/
Ekstrand JJ, Herbener A, Rawlings J, Turney B, Ampofo K, Korgenski EK et al (2010) Heightened neurologic complications in children with pandemic H1N1 influenza. Ann Neurol 68(5):762. https://pubmed.ncbi.nlm.nih.gov/20865762/
Khandaker G, Zurynski Y, Buttery J, Marshall H, Richmond PC, Dale RC et al (2012) Neurologic complications of influenza A(H1N1)pdm09: surveillance in 6 pediatric hospitals. Neurology 79(14):1474–81. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4098823/
Cárdenas G, Soto‐Hernández JL, Díaz‐Alba A, Ugalde Y, Mérida‐Puga J, Rosetti M et al (2014) Neurological events related to influenza A ( H1 N1) pdm09. Influenza Other Respir Virus 8(3):339. https://pubmed.ncbi.nlm.nih.gov/24895698/
Morishima T, Togashi T, Yokota S, Okuno Y, Miyazaki C, Tashiro M et al (2002) Encephalitis and encephalopathy associated with an influenza epidemic in Japan. Clin Infect Dis 35(5):512–7. https://pubmed.ncbi.nlm.nih.gov/12173123/
Popescu CP, Florescu SA, Lupulescu E, Zaharia M, Tardei G, Lazar M et al (2017) Neurologic complications of influenza B virus infection in adults, Romania. Emerg Infect Dis 23(4):574–81. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5367398/
McCullers JA, Facchini S, Chesney PJ, Webster RG (1999) Influenza B virus encephalitis. Clin Infect Dis 28(4):898–900. https://pubmed.ncbi.nlm.nih.gov/10825057/
Sazgar M, Robinson JL, Chan AKJ, Sinclair DB (2003) Influenza B acute necrotizing encephalopathy: a case report and literature review. Pediatr Neurol 28(5):396–9. https://pubmed.ncbi.nlm.nih.gov/12878304/
Togashi T, Matsuzono Y, Narita M, Morishima T (2004) Influenza-associated acute encephalopathy in Japanese children in 1994–2002. Virus Res 103(1):75–8. https://pubmed.ncbi.nlm.nih.gov/15163492/
Chen LW, Teng CK, Tsai YS, Wang JN, Tu YF, Shen CF et al (2018) Influenza-associated neurological complications during 2014–2017 in Taiwan. Brain Dev 40(9):799–806. https://pubmed.ncbi.nlm.nih.gov/29891404/
Freeman JL, Coleman LT, Smith LJ, Shield LK (2002) Hemiconvulsion-hemiplegia-epilepsy syndrome: characteristic early magnetic resonance imaging findings. J Child Neurol 17(1):10–6. https://pubmed.ncbi.nlm.nih.gov/11913562/
Takanashi J ichi, Tsuji M, Amemiya K, Tada H, Barkovich AJ (2007) Mild influenza encephalopathy with biphasic seizures and late reduced diffusion. J Neurol Sci 256(1):86–9. https://pubmed.ncbi.nlm.nih.gov/17367813/
Tada H, Takanashi J, Barkovich AJ, Oba H, Maeda M, Tsukahara H et al (2004) Clinically mild encephalitis/encephalopathy with a reversible splenial lesion. Neurology 63(10):1854–8. https://pubmed.ncbi.nlm.nih.gov/15557501/
Chaves-Carballo E, Montes JE, Nelson WB, Chrenka BA (1990) Hemorrhagic shock and encephalopathy. Clinical definition of a catastrophic syndrome in infants. Am J Dis Child 144(10):1079–82. https://pubmed.ncbi.nlm.nih.gov/2403087/
Levin M, Hjelm M, Kay JD, Pincott JR, Gould JD, Dinwiddie R et al (1983) Haemorrhagic shock and encephalopathy: a new syndrome with a high mortality in young children. Lancet 2(8341):64–7. https://pubmed.ncbi.nlm.nih.gov/6134958/
Laino D, Mencaroni E, Esposito S. Management of pediatric febrile seizures. Int J Environ Res Public Health. https://pubmed.ncbi.nlm.nih.gov/30321985/
Kwong KL, Lam SY, Que TL, Wong SN (2006) Influenza A and febrile seizures in childhood. Pediatr Neurol 35(6):395–9. https://pubmed.ncbi.nlm.nih.gov/17138008/
Chiu SS, Tse CY, Lau YL, Peiris M (2001) Influenza A infection is an important cause of febrile seizures. Pediatrics 108(4):E63–E63. https://pubmed.ncbi.nlm.nih.gov/11581471/
Chung B, Wong V (2007) Relationship between five common viruses and febrile seizure in children. Arch Dis Childhood 92(7):589. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2083759/
Hara K, Tanabe T, Aomatsu T, Inoue N, Tamaki H, Okamoto N et al (2007) Febrile seizures associated with influenza A. Brain Dev 29(1):30–8. https://pubmed.ncbi.nlm.nih.gov/16859852/
Huang YC, Lin TY, Wu SL, Tsao KC (2003) Influenza A-associated central nervous system dysfunction in children presenting as transient visual hallucination. Pediatr Infect Dis J 22(4):366–8. https://pubmed.ncbi.nlm.nih.gov/12690279/
Okumura A, Nakano T, Fukumoto Y, Higuchi K, Kamiya H, Watanabe K et al (2005) Delirious behavior in children with influenza: its clinical features and EEG findings. Brain Dev 27(4):271–4. https://pubmed.ncbi.nlm.nih.gov/15862189/
Kashiwagi M, Tanabe T, Ooba C, Masuda M, Shigehara S, Murata S et al (2015) Differential diagnosis of delirious behavior in children with influenza. Brain Dev 37(6):618–24. https://pubmed.ncbi.nlm.nih.gov/25277296/
Bertrand A, Janbon F, Clot J, Milane J, Bosc E (1971) [Guillain-Barre polyradiculoneuritis and influenza virus]. Presse Med 79(51):2328. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1828628/
Burwen DR, Ball R, Bryan WW, Izurieta HS, Voie LL, Gibbs NA et al (2010) Evaluation of Guillain-Barré syndrome among recipients of influenza vaccine in 2000 and 2001. Am J Prevent Med 39(4):296–304. https://pubmed.ncbi.nlm.nih.gov/20837279/
Chaari A, Bahloul M, Dammak H, Nourhene G, Rekik N, Hedi C et al (2010) Guillain–Barré syndrome related to pandemic influenza A (H1N1) infection. Intensive Care Med 36(7):1275. https://pubmed.ncbi.nlm.nih.gov/20428843/
Clarence C. Tam, Sarah J. O’Brien, Rodrigues LC (2006) Influenza, campylobacter and mycoplasma infections, and hospital admissions for Guillain-Barré syndrome, England. Emerg Infect Dis (12):1880. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3291336/
Giambrone GP, Zansky SM, Eidson M, Duncan PG, McNutt LA, Birkhead GS (2013) Guillain-Barré syndrome surveillance during national influenza vaccination campaign, New York, USA, 2009. Emerg Infect Dis 19(12):1956–62. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3840872/
Haber P, DeStefano F, Angulo FJ, Iskander J, Shadomy SV, Weintraub E et al (2004) Guillain-Barré syndrome following influenza vaccination. JAMA 292(20):2478–81. https://pubmed.ncbi.nlm.nih.gov/15562126/
Juurlink DN, Stukel TA, Kwong J, Kopp A, McGeer A, Upshur RE et al (2006) Guillain-Barré syndrome after influenza vaccination in adults: a population-based study. Arch Intern Med 166(20):2217–21. https://pubmed.ncbi.nlm.nih.gov/17101939/
Lehmann HC, Hartung HP, Kieseier BC, Hughes RA (2010) Guillain-Barré syndrome after exposure to influenza virus. Lancet Infect Dis 10(9):643–51. https://pubmed.ncbi.nlm.nih.gov/20797646/
Kumar P, Panigrahi I, Sankhyan N, Ahuja C, Goyadi PK (2018) Down syndrome with moyamoya disease: a case series. J Pediatr Neurosci 13(2):201. https://pubmed.ncbi.nlm.nih.gov/30090136/
Tavares Bello C, Barreiros C, Gil I, Vasconcelos C (2017) Down syndrome and Moyamoya disease: unusual cause of stroke. BMJ Case Rep 2017. https://pubmed.ncbi.nlm.nih.gov/28647711/
Dildar N, Bangash A, Nadeem F, Gul P, Rauf S (2017) Recurrent strokes secondary to moyamoya phenomenon in a child with down’s syndrome. Pakistan Armed Forces Med J 67(1):182
Amlie-Lefond C, Gilden D (2016) Varicella zoster virus: a common cause of stroke in children and adults. J Stroke Cerebrovasc Dis 25(7):1561–9. https://pubmed.ncbi.nlm.nih.gov/27138380/
Lanthier S, Armstrong D, Domi T, deVeber G (2005) Post-varicella arteriopathy of childhood: natural history of vascular stenosis. Neurology 64(4):660–3. https://pubmed.ncbi.nlm.nih.gov/15728288/
Losurdo G, Giacchino R, Castagnola E, Gattorno M, Costabel S, Rossi A et al (2006) Cerebrovascular disease and varicella in children. Brain Dev 28(6):366–70. https://pubmed.ncbi.nlm.nih.gov/16376509/
Yen YF, Jen I, Chen M, Chuang PH, Liu YL, Sharp GB et al (2016) Association of cytomegalovirus end-organ disease with stroke in people living with HIV/AIDS: a nationwide population-based cohort study. PLoS ONE 11(3):1–13. https://pubmed.ncbi.nlm.nih.gov/26986005/
Fullerton HJ, Luna JM, Wintermark M, Hills NK, Tokarz R, Li Y et al (2017) Parvovirus B19 infection in children with arterial ischemic stroke. Stroke 48(10):2875–7. https://pubmed.ncbi.nlm.nih.gov/28864597/
Forbes HJ, Williamson E, Benjamin L, Breuer J, Brown MM, Langan SM et al (2018) Association of herpesviruses and stroke: systematic review and meta-analysis. PLoS ONE 13(11):1–33. https://pubmed.ncbi.nlm.nih.gov/30462656/
Anand G, Visagan R, Chandratre S, Segal S, Nemeth AH, Squier W et al (2015) H1N1 triggered recurrent acute necrotizing encephalopathy in a family with a T653I mutation in the RANBP2 gene. Pediatr Infect Dis J 34(3):318–20. https://pubmed.ncbi.nlm.nih.gov/25170550/
Howard A, Uyeki TM, Fergie J (2018) Influenza-associated acute necrotizing encephalopathy in siblings. J Pediatric Infect Dis Soc 7(3):e172–7. https://pubmed.ncbi.nlm.nih.gov/29741717/
Bloch C, Suter B, Fischmann A, Gensicke H, Rüegg S, Weisser M (2015) Only a touch of the flu? The simultaneous manifestation of acute necrotizing encephalopathy in two consanguineous patients. Open Forum Infect Dis 2(2):ofv013. https://pubmed.ncbi.nlm.nih.gov/26110162/
Gika AD, Rich P, Gupta S, Neilson DE, Clarke A (2010) Recurrent acute necrotizing encephalopathy following influenza A in a genetically predisposed family. Dev Med Child Neurol 52(1):99–102. https://pubmed.ncbi.nlm.nih.gov/19811512/
Neilson DE, Adams MD, Orr CMD, Schelling DK, Eiben RM, Kerr DS et al (2009) Infection-triggered familial or recurrent cases of acute necrotizing encephalopathy caused by mutations in a component of the nuclear pore, RANBP2. Am J Hum Genet 84(1):44–51. https://pubmed.ncbi.nlm.nih.gov/19811512/
Yao D, Mizuguchi H, Yamaguchi M, Yamada H, Chida J, Shikata K et al (2008) Thermal instability of compound variants of carnitine palmitoyltransferase II and impaired mitochondrial fuel utilization in influenza-associated encephalopathy. Hum Mutat 29(5):718–27. https://pubmed.ncbi.nlm.nih.gov/18306170/
Chen Y, Mizuguchi H, Yao D, Ide M, Kuroda Y, Shigematsu Y et al (2005) Thermolabile phenotype of carnitine palmitoyltransferase II variations as a predisposing factor for influenza-associated encephalopathy. FEBS Lett 579(10):2040–4. https://pubmed.ncbi.nlm.nih.gov/15811315/
Kobayashi Y, Kanazawa H, Hoshino A, Takamatsu R, Watanabe R, Hoshi K et al (2019) Acute necrotizing encephalopathy and a carnitine palmitoyltransferase 2 variant in an adult. J Clin Neurosci 61:264–6. https://pubmed.ncbi.nlm.nih.gov/30470651/
Akins PT, Belko J, Uyeki TM, Axelrod Y, Lee KK, Silverthorn J (2010) H1N1 encephalitis with malignant edema and review of neurologic complications from influenza. Neurocrit Care 13(3):396–406. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7222163/
Ito Y, Ichiyama T, Kimura H, Shibata M, Ishiwada N, Kuroki H et al (1999) Detection of influenza virus RNA by reverse transcription-PCR and proinflammatory cytokines in influenza-virus-associated encephalopathy. J Med Virol 58(4):420–5. https://pubmed.ncbi.nlm.nih.gov/10421411/
Koh JC, Murugasu A, Krishnappa J, Thomas T (2019) Favorable outcomes with early interleukin-6 receptor blockade in severe acute necrotizing encephalopathy of childhood. Pediatr Neurol. https://pubmed.ncbi.nlm.nih.gov/31201070/
Author information
Authors and Affiliations
Contributions
Violette Goetz, Mélodie Aubart, François Angoulvant, and Isabelle Desguerres contributed to the conception and design of the study. Hanene Abid provided the list of children having influenza virus PCR. Violette Goetz collected and assembled data. Violette Goetz, François Angoulvant, and David-Dawei Yang performed the analysis. Charles-Joris Roux and Raphael Levy selected MRI and CTM iconography. All authors contributed to manuscript revision and read and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics approval
No animal studies are presented in this manuscript. The study was performed using a data warehouse (DrWH®) that has received ethical approval by the French IRB CPP Ile-de-France II (IRB registration number 00001072), registered under reference 2016–06-01. No potentially identifiable human images or data is presented in this study.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Tobias Tenenbaum.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Goetz, V., Yang, DD., Abid, H. et al. Neurological features related to influenza virus in the pediatric population: a 3-year monocentric retrospective study. Eur J Pediatr 182, 2615–2624 (2023). https://doi.org/10.1007/s00431-023-04901-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04901-9