Abstract
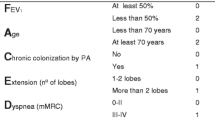
Several clinical scales have been developed to assess the severity of bronchiolitis as well as the probability of needing in-hospital care. A recent systematic review of 32 validated clinical scores for bronchiolitis concluded that 6 of them (Wood-Downes, M-WCAS, Respiratory Severity Score, Respiratory Clinical Score, Respiratory Score and Bronchiolitis risk of admission score) were the best ones regarding reliability, sensitivity, validity, and usability. However, to the best of our knowledge, no study has compared all of them in a clinical scenario. Also, after this review, three more scales were published: BROSJOD, Tal modified, and one score developed by PERN. Our main aim was to compare the ability of different clinical scales for bronchiolitis to predict any relevant outcome. A prospective observational study was conducted that included patients of up to 12 months old attended to, due to bronchiolitis, in the paediatric Emergency Department of a secondary university hospital from October 2019 to January 2022. For each patient, the attending clinician filled in a form with the items of the scales, decomposed, in order to prevent the clinician from knowing the score of each scale. Then, the patient was managed according to the protocol of our Emergency Department. A phone call was made to each patient in order to check whether the patient ended up being admitted in the next 48 h. In the case of those that were impossible to contact by phone, the clinical history was reviewed. For the purpose of the study, any of the following were considered to be a relevant outcome: admission to ward and need for supplementary oxygen, non-invasive ventilation (NIV) or intravenous fluids, and admission to the paediatric intensive care unit (PICU) within the next 48 h or death. For the aim of the study, the area under the curve (AUC) and the odds ratio (OR) for a relevant outcome were calculated in each scale. Also, the best cut-off point was estimated according to the Youden index, and its sensitivity (Sn) and specificity (Sp) for a relevant outcome were calculated. We included 265 patients (52.1% male) with a median age of 5.3 months (P25-P75 2.6–7.4). Among them, 46 (17.4%) had some kind of relevant outcome. AUC for prediction of a relevant outcome ranged from 0.705 (Respiratory Score) to 0.786 (BRAS), although no scale performed significantly better than others. A score ≤ 2 in the PERN scale showed a sensitivity of 91.3% (CI95% 79.7–96.6) for a relevant outcome, with only 4 misdiagnosed patients (only 2 of them needed NIV).
Conclusions: There were no differences in the performance of the nine scales to predict relevant outcomes in patients with bronchiolitis. However, the PERN scale might be more useful to select patients at low risk of a severe outcome.
What is Known: • Several clinical scales are used to assess the severity of bronchiolitis. Nevertheless, none of them seems to be better than others. | |
What is New: • This is the first study comparing different bronchiolitis scales in a real clinical scenario. None of the nine scales compared performed better than the other. However, the PERN scale might be more useful to select patients at low risk of relevant outcomes. |
Similar content being viewed by others
Availability of data and material
All data of the study are at disposal of the editor if needed.
Abbreviations
- AUC:
-
Area under the curve
- BRAS:
-
Bronchiolitis Risk of Admission Score
- ED :
-
Emergency department
- P25-p75:
-
First and third quartiles
- M-WCAS:
-
Modified Wood’s Clinical Asthma Score
- NIV:
-
Non-invasive ventilation
- PEM:
-
Paediatric Emergency Medicine
- PERN:
-
Pediatric Emergency Research Network
- PICU:
-
Paediatric intensive care unit
- RCS:
-
Respiratory Clinical Score
- RSS:
-
Respiratory Severity Score
- Sn:
-
Sensitivity
- Sp:
-
Specificity
References
Fujiogi M, Goto T, Yasunaga H, Fujishiro J, Mansbach JM, Camargo CA et al (2019) Trends in bronchiolitis hospitalizations in the United States: 2000–2016. Pediatrics 144(6):e20192614
Cano-Garcinuño A, Praena-Crespo M, Mora-Gandarillas I, Carvajal-Urueña I, Callén-Blecua MT, García-Merino Á et al (2019) Heterogeneidad de criterios en el diagnóstico de bronquiolitis aguda en España. An Pediatría 90(2):109–117
Meissner HC (2016) Viral bronchiolitis in children. Ingelfinger JR, editor. N Engl J Med 374(1):62–72
Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM et al (2014) Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics 134(5):e1474–e1502
Bronchiolitis in children (2021) diagnosis and management. National Institute for Health and Care Excellence (NICE), London
O’Brien S, Borland ML, Cotterell E, Armstrong D, Babl F, Bauert P et al (2019) Australasian bronchiolitis guideline: Australasian bronchiolitis guideline. J Paediatr Child Health 55(1):42–53
Bekhof J, Reimink R, Brand PL (2014) Systematic review: insufficient validation of clinical scores for the assessment of acute dyspnoea in wheezing children. Paediatr Respir Rev 15(1):98–112. https://doi.org/10.1016/j.prrv.2013.08.004. (Epub 2013 Oct 11 PMID: 24120749)
Davies CJ, Waters D, Marshall A (2017) A systematic review of the psychometric properties of bronchiolitis assessment tools. J Adv Nurs 73(2):286–301. https://doi.org/10.1111/jan.13098. (Epub 2016 Sep 21 PMID: 27509019)
Rodriguez-Martinez CE, Sossa-Briceño MP, Nino G (2018) Systematic review of instruments aimed at evaluating the severity of bronchiolitis. Paediatr Respir Rev 25:43–57
Rodriguez H, Hartert TV, Gebretsadik T, Carroll KN, Larkin EK (2016) A simple respiratory severity score that may be used in evaluation of acute respiratory infection. BMC Res Notes 9(1):85
Ferres J (1992) Inhalation therapy in the newborn. An Esp Pediatr 36(Suppl 49):160–163
Duarte-Dorado DM, Madero-Orostegui DS, Rodriguez-Martinez CE, Nino G (2013) Validation of a scale to assess the severity of bronchiolitis in a population of hospitalized infants. J Asthma 50(10):1056–1061
Liu LL, Gallaher MM, Davis RL, Rutter CM, Lewis TC, Marcuse EK (2004) Use of a respiratory clinical score among different providers. Pediatr Pulmonol 37(3):243–248
Gajdos V, Beydon N, Bommenel L, Pellegrino B, de Pontual L, Bailleux S et al (2009) Inter-observer agreement between physicians, nurses, and respiratory therapists for respiratory clinical evaluation in bronchiolitis. Pediatr Pulmonol 44(8):754–762
Marlais M, Evans J, Abrahamson E (2011) Clinical predictors of admission in infants with acute bronchiolitis. Arch Dis Child 96(7):648–652
Balaguer M, Alejandre C, Vila D, Esteban E, Carrasco JL, Cambra FJ et al (2017) Bronchiolitis score of Sant Joan de Déu: BROSJOD Score, validation and usefulness. Pediatr Pulmonol 52(4):533–539
Golan-Tripto I, Goldbart A, Akel K, Dizitzer Y, Novack V, Tal A (2018) Modified Tal Score: Validated score for prediction of bronchiolitis severity. Pediatr Pulmonol 53(6):796–801
Freire G, Kuppermann N, Zemek R, Plint AC, Babl FE, Dalziel SR et al (2018) Predicting escalated care in infants with bronchiolitis. Pediatrics 142(3):e20174253
Modesto i Alapont V, Garcia Cuscó M, Medina A (2018) High-flow oxygen therapy in infants with bronchiolitis. N Engl J Med 378(25):2444
Del Villar-Guerra P, Medina A, Gutiérrez M, Modesto I, Alapont V (2020) High-flow therapy for bronchiolitis. J Paediatr Child Health 56(1):182–185. https://doi.org/10.1111/jpc.14761. PMID: 31943471
O’Brien S, Craig S, Babl FE, Borland ML, Oakley E, Dalziel SR et al (2019) Rational use of high-flow therapy in infants with bronchiolitis. What do the latest trials tell us? A Paediatric Research in Emergency Departments International Collaborative perspective: Use of high flow for bronchiolitis. J Paediatr Child Health 55(7):746–52
van Koningsveld R, Steyerberg EW, Hughes RA, Swan AV, van Doorn PA, Jacobs BC (2007) A clinical prognostic scoring system for Guillain-Barré syndrome. Lancet Neurol 6(7):589–594
Gudjonsdottir J, Marklund E, Hagander L, Salö M (2021) Clinical prediction scores for pediatric appendicitis. Eur J Pediatr Surg 31(03):252–260
Schonfeld D, Bressan S, Da Dalt L, Henien MN, Winnett JA, Nigrovic LE (2014) Pediatric Emergency Care Applied Research Network head injury clinical prediction rules are reliable in practice. Arch Dis Child 99(5):427–431
Smith SR, Baty JD, Hodge D (2002) Validation of the pulmonary score: an asthma severity score for children. Acad Emerg Med 9(2):7
Alnaji F, Zemek R, Barrowman N, Plint A (2014) PRAM score as predictor of pediatric asthma hospitalization. Walthall J, editor. Acad Emerg Med 21(8):872–8
Rivas-Juesas C, Rius Peris JM, García AL, Madramany AA, Peris MG, Álvarez LV, Primo J (2018) A comparison of two clinical scores for bronchiolitis. A multicentre and prospective study conducted in hospitalised infants. Allergol Immunopathol (Madr) 46(1):15–23. https://doi.org/10.1016/j.aller.2017.01.012. Epub 2017 Jun 16. PMID: 28629673
Faber TE, Kamps AW, Sjoerdsma MH, Vermeulen S, Veeger NJ, Bont LJ (2015) Computerized assessment of wheezing in children with respiratory syncytial virus bronchiolitis before and after hypertonic saline nebulization. Respir Care 60(9):1252–1256
Kuppermann N, Holmes JF, Dayan PS, Hoyle JD, Atabaki SM, Holubkov R et al (2009) Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet 374(9696):1160–1170
Holmes JF, Wisner DH, McGahan JP, Mower WR, Kuppermann N (2009) Clinical prediction rules for identifying adults at very low risk for intra-abdominal injuries after blunt trauma. Ann Emerg Med 54(4):575–584
Torres-Fernandez D, Casellas A, Mellado MJ, Calvo C, Bassat Q (2021) Acute bronchiolitis and respiratory syncytial virus seasonal transmission during the COVID-19 pandemic in Spain: a national perspective from the pediatric Spanish Society (AEP). J Clin Virol 145:105027
Curatola A, Lazzareschi I, Bersani G, Covino M, Gatto A, Chiaretti A (2021) Impact of COVID-19 outbreak in acute bronchiolitis: lesson from a tertiary Italian Emergency Department. Pediatr Pulmonol 56(8):2484–2488
Acknowledgements
We acknowledge all the members of the paediatric emergency department for their substantial contribution to the development of the study.
Author information
Authors and Affiliations
Contributions
Elena Granda conceptualized and designed the study, collaborated in data collection, revised multiple drafts of the manuscript, and critically revised the final submitted manuscript. Roberto Velasco designed the study, analysed the data, wrote the initial draft of the manuscript, and approved the final manuscript as submitted. Mario Urbano, Pilar Andrés, Marina Corchete, and Alfredo Cano collaborated in the design of the study and in data collection, revised multiple manuscript drafts, and critically revised the final submitted manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Ethics Committee of Valladolid Oeste.
Consent to participate
Written consent from the parents or caregivers was obtained prior to the participation of every included patient.
Consent for publication
Informed consent was obtained prior to the publication of every included patient.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Piet Leroy.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Granda, E., Urbano, M., Andrés, P. et al. Comparison of severity scales for acute bronchiolitis in real clinical practice. Eur J Pediatr 182, 1619–1626 (2023). https://doi.org/10.1007/s00431-023-04840-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04840-5