Abstract
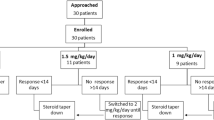
Nephrotic syndrome is the commonest glomerular disease in childhood. It usually follows a relapsing and remitting course. Corticosteroids are the mainstay of treatment for both the first episode and subsequent relapses. This study was conducted at a single centre to compare the clinical response to a single dose vs. split dose of prednisolone in the treatment of relapses of childhood nephrotic syndrome. Children between the ages of 1 and 14 years admitted with a relapse of idiopathic steroid sensitive nephrotic syndrome from August 2019 to February 2020 were considered for recruitment. A block randomization method based on age was used for allocation. Patients randomised to group A received oral prednisolone at 60 mg/m2 as a single morning dose, while those randomised to group B received the same total dose as two divided doses, of which 2/3 was given in the morning and the rest in the evening. Treatment was continued until remission was achieved following which all patients were switched to alternate day prednisolone. An independent sample t test was used to compare the two groups. One hundred and four episodes of relapse occurring in 96 children were included of which 49 were treated with prednisolone as a split dose and 55 were treated with a single dose of prednisolone. The mean duration to achieve remission for the split-dose group was 8.02 days (SD 1.58) while it was 9.74 days (SD 3.72) for the single-dose group. This difference was statistically highly significant (t(102) = 3.004; p = 0.001; CI 0.58 to 2.86). There was no difference in the adverse events profile of the two groups.
Conclusion: The use of prednisolone as a split dose results in a shorter duration to achieve remission when compared to a single morning dose, resulting in a lower cumulative dose of prednisolone to achieve remission.
What is Known: • Corticosteroids are the mainstay of treatment for childhood nephrotic syndrome. • Corticosteroids are given as a single dose in the morning to minimise adrenocortical suppression. | |
What is New: • A more rapid attainment of remission can be achieved with a split dose of corticosteroids. |



Similar content being viewed by others
Data availability
The data is available on request. However as patient confidentiality issues may arise prior approval from the Scientific and Ethics Committee, Faculty of Medicine, University of Peradeniya, Sri Lanka will need to be obtained before release.
References
Schnaper HW (1989) The immune system in minimal change nephrotic syndrome. Pediatr Nephrol 3(1):101–110. https://doi.org/10.1007/BF00859637
Shalhoub R (1974) Pathogenesis of lipoid nephrosis: a disorder of T-cell function. The Lancet 304(7880):556–560. https://doi.org/10.1016/S0140-6736(74)91880-7
Czock D, Keller F, Rasche FM, Häussler U (2005) Pharmacokinetics and pharmacodynamics of systemically administered glucocorticoids. Clin Pharmacokinet 44(1):61–98. https://doi.org/10.2165/00003088-200544010-00003
Ekka BK, Bagga A, Srivastava RN (1997) Single-versus divided-dose prednisolone therapy for relapses of nephrotic syndrome. Pediatr Nephrol 11(5):597–599. https://doi.org/10.1007/s004670050344
Brodehl J (1981) Alternate-day prednisone is more effective than intermittent prednisone in frequently relapsing nephrotic syndrome. Eur J Pediatr 135(3):229–237. https://doi.org/10.1007/BF00442096
Coleman J, Hopkins A, Houston IB, Joseph A, Watson AR, Jones KV Consensus statement on management and audit potential for steroid responsive nephrotic syndrome. https://doi.org/10.1136/adc.70.2.151
Ackerman GL, Nolan CM (1968) Adrenocortical responsiveness after alternate-day corticosteroid therapy. N Engl J Med 278(8):405–409. https://doi.org/10.1056/NEJM196802222780801
Leonard MB, Feldman HI, Shults J, Zemel BS, Foster BJ, Stallings VA (2004) Long-term, high-dose glucocorticoids and bone mineral content in childhood glucocorticoid-sensitive nephrotic syndrome. N Engl J Med 351(9):868–875. https://doi.org/10.1056/NEJMoa040367
Warshaw BL, Hymes LC (1989) Daily single-dose and daily reduced-dose prednisone therapy for children with the nephrotic syndrome. Pediatrics 83(5):694–699. https://doi.org/10.1542/peds.83.5.694
Choonara IA, Heney D, Meadow SR (1989) Low dose prednisolone in nephrotic syndrome. Arch Dis Child 64(4):610–611. https://doi.org/10.1136/adc.64.4.610
Park SJ, Shin JI (2011) Complications of nephrotic syndrome. Korean J Ped 54(8):322. https://doi.org/10.3345/kjp.2011.54.8.322
Yates CJ, Fourlanos S, Colman PG, Cohney SJ (2014) Divided dosing reduces prednisolone-induced hyperglycaemia and glycaemic variability: a randomized trial after kidney transplantation. Nephrol Dial Transplant 29(3):698–705. https://doi.org/10.1093/ndt/gft377
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Dr. W A L K Weerasooriya, Prof. R S Thalgahagoda and Prof. A S Abeyagunawardana. The first draft of the manuscript was written by Dr. W A L K Weerasooriya, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of University Peradeniya, Sri Lanka (date 10/05/20019/NO-2018/EC/26).
Consent to participate
Informed consent was obtained from parents or guardians of all individual participants included in the study.
Consent for publication
Not relevant.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Weerasooriya, W.A.L.K., Abeyagunawardena, A.S. & Thalgahagoda, R.S. Single vs split dose of prednisolone in the treatment of relapses of childhood nephrotic syndrome. Eur J Pediatr 182, 1741–1747 (2023). https://doi.org/10.1007/s00431-023-04804-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04804-9