Abstract
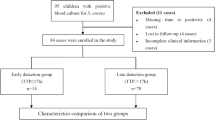
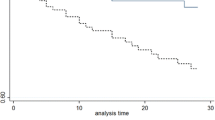
Persistent S. aureus bloodstream infection (PSBSI) increased the incidence of metastatic infection and mortality. We aimed to clarify its risk factors and correlation with metastatic infection and septic shock in children. This retrospective and observational study enrolled children with S. aureus bloodstream infection who admitted to Children’s Hospital of Chongqing Medical University between January 2016 and December 2021. The logistic regression model was used for multivariable analyses to determine independent factors associated with PSBSI and clarify the effect of persistent S. aureus bloodstream infection and other factors on metastatic infection and septic shock. One hundred and twenty-seven children were included in this study retrospectively. There were thirty-two cases in the persistent S. aureus bloodstream infection group and ninety-five children in the non-persistent infection group. Multivariate logistic regression analysis indicated that inappropriate empirical antibiotic therapy (OR, 7.26; 95%CI, 2.48–21.30; P<0.01) was an independent risk factor of persistent S. aureus bloodstream infection. Persistent S. aureus bloodstream infection (OR, 6.40; 95%CI, 2.08–19.70; P<0.01) and community-acquired S. aureus bloodstream infection (OR, 4.75; 95%CI, 1.34–16.89; P=0.02) were independent predictors of metastatic infection. Pittsburgh bacteremia scores ≥ 2 (OR, 28.81; 95%CI, 5.26–157.99; P<0.01), hypoalbuminemia (OR, 13.34; 95%CI, 2.43–73.28; P<0.01) and persistent S. aureus bloodstream infection (OR, 5.48; 95%CI, 1.13–26.54; P=0.04) were independent risk factors of septic shock.
Conclusion: Inappropriate empirical antibiotic therapy was an independent risk factor of pediatric persistent S. aureus bloodstream infection. Pediatric persistent S. aureus bloodstream infection was associated with metastatic infection and septic shock.
What is Known: • Pathogenic features such as Methicillin-resistant S. aureus and sources of infection such as central venous catheter related infection were risk factors of PSBSI in adults. • PSBSI increased the incidence of metastatic infection and mortality in adults. | |
What is New: • Inappropriate empirical antibiotic therapy was an independent risk factor of pediatric persistent S. aureus bloodstream infection. • Pediatric persistent S. aureus bloodstream infection was associated with metastatic infection and septic shock. |





Similar content being viewed by others
Data Availability
The data-sets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CI :
-
Confidence interval
- S. aureus :
-
Staphylococcus aureus
- MRSA :
-
Methicillin-resistant S. aureus
- MSSA :
-
Methicillin-sensitive S. aureus
- PICU:
-
Pediatric Intensive Care Unit
- PSBSI:
-
Persistent S. aureus bloodstream infection
- OR :
-
Odds ratio
- ROC :
-
Receiver operating characteristic
- TTP:
-
Time to positive
- IQR:
-
Inter-quartile ranges
- *:
-
P<0.05
References
Ferreira M, Santos M, Rodrigues J, Diogo C, Resende C, Baptista C, Faria C (2021) Epidemiology of bacteremia in a pediatric population-a 10-year study. Enferm Infecc Microbiol Clin. https://doi.org/10.1016/j.eimc.2021.06.011
Luthander J, Bennet R, Giske CG, Eriksson M, Nilsson A (2020) Trends of pediatric bloodstream infections in Stockholm, Sweden: a 20-year retrospective study. Pediatr Infect Dis J. https://doi.org/10.1097/INF.0000000000002850
Wang X, Zhao C, Li H, Chen H, Jin L, Wang Z, Liao K, Zeng J, Xu X, Jin Y, Su D, Liu W, Hu Z, Cao B, Chu Y, Zhang R, Luo Y, Hu B, Wang H (2018) Microbiological profiles of pathogens causing nosocomial bacteremia in 2011, 2013 and 2016. Sheng Wu Gong Cheng Xue Bao. https://doi.org/10.13345/j.cjb.180192
Qiu Y, Yang J, Chen Y, Yang J, Zhu Q, Zhu C, Li S, Liu J, Wan C, Zhu Y, Chen M, Xu Y, Tong J, Li R, Shan Q, Lin D, Wu S, Zhuo Z, Wang C, Zhao S, Qi Z, Sun X, Maihebuba B, Jia C, Gao H, Cheng Y, Zeng M (2021) Microbiological profiles and antimicrobial resistance patterns of pediatric bloodstream pathogens in China, 2016–2018. Eur J Clin Microbiol Infect Dis. https://doi.org/10.1007/s10096-020-04069-2
Ok HS, Lee HS, Park MJ, Kim KH, Kim BK, Wi YM, Kim JM (2013) Predictors and clinical outcomes of persistent methicillin-resistant Staphylococcus aureus bacteremia: a prospective observational study. Korean J Intern Med. https://doi.org/10.3904/kjim.2013.28.6.678
Minejima E, Bensman J, She RC, Mack WJ, Tran MT, Ny P, Lou M, Yamaki J, Nieberg P, Ho J, Wong-Beringer A (2016) A dysregulated balance of proinflammatory and anti-inflammatory host cytokine response early during therapy predicts persistence and mortality in Staphylococcus aureus bacteremia. Crit Care Med. https://doi.org/10.1097/CCM.0000000000001465
Tan K, Minejima E, Lou M, Mack WJ, Nieberg P, Wong-Beringer A (2021) Cytokine measurements add value to clinical variables in predicting outcomes for Staphylococcus aureus bacteremia. BMC Infect Dis. https://doi.org/10.1186/s12879-021-06010-0
Alonso GA, Loarte MDC, Ramos RN, Jiménez MC, Ruiz-Capillas JJJ (2018) Staphylococcus aureus bacteremia in a secondary level Spanish hospital: clinical implications of high vancomycin MIC. Rev Esp Quimioter 31:353–362
Khatib R, Johnson LB, Fakih MG, Riederer K, Khosrovaneh A, Shamse Tabriz M, Sharma M, Saeed S (2006) Persistence in staphylococcus aureus bacteremia: incidence, characteristics of patients and outcome. Scand J Infect Dis. https://doi.org/10.1080/00365540500372846
Park KH, Lee YM, Hong HL, Kim T, Park HJ, Park SY, Moon SM, Chong YP, Kim SH, Lee SO, Choi SH, Jeong JY, Kim MN, Woo JH, Kim YS (2012) Persistent catheter-related Staphylococcus aureus bacteremia after catheter removal and initiation of antimicrobial therapy. PLoS ONE. https://doi.org/10.1371/journal.pone.0046389
Chong YP, Park KH, Kim ES, Kim MN, Kim SH, Lee SO, Choi SH, Jeong JY, Woo JH, Kim YS (2014) Association of mannose-binding lectin 2 gene polymorphisms with persistent Staphylococcus aureus bacteremia. PLoS ONE. https://doi.org/10.1371/journal.pone.0089139
Lee YM, Chong YP, Kim M, Eom Y, Kim ES, Kim M, Park KH, Kim SH, Lee SO, Choi SH, Woo JH, Kim YS (2020) Long-term methicillin-resistant Staphylococcus aureus bacteremia persisting for more than 2 weeks: risk factors and outcomes. Eur J Clin Microbiol Infect Dis. https://doi.org/10.1007/s10096-019-03795-6
Park SY, Chong YP, Park HJ, Park KH, Moon SM, Jeong JY, Kim MN, Kim SH, Lee SO, Choi SH, Woo JH, Kim YS (2013) Agr dysfunction and persistent methicillin-resistant Staphylococcus aureus bacteremia in patients with removed eradicable foci. Infection. https://doi.org/10.1007/s15010-012-0348-0
Kuehl R, Morata L, Boeing C, Subirana I, Seifert H, Rieg S, Kern WV, Kim HB, Kim ES, Liao CH, Tilley R, Lopez-Cortés LE, Llewelyn MJ, Fowler VG, Thwaites G, Cisneros JM, Scarborough M, Nsutebu E, Gurgui Ferrer M, Pérez JL, Barlow G, Hopkins S, Ternavasio-de la Vega HG, Török ME, Wilson P, Kaasch AJ, Soriano A; International Staphylococcus aureus collaboration study group and the ESCMID Study Group for Bloodstream Infections, Endocarditis and Sepsis (2020) Defining persistent Staphylococcus aureus bacteraemia: secondary analysis of a prospective cohort study. Lancet Infect Dis. https://doi.org/10.1016/S1473-3099(20)30447-3
Minejima E, Mai N, Bui N, Mert M, Mack WJ, She RC, Nieberg P, Spellberg B, Wong-Beringer A (2020) Defining the breakpoint duration of Staphylococcus aureus bacteremia predictive of poor outcomes. Clin Infect Dis. https://doi.org/10.1093/cid/ciz257
Neuner EA, Casabar E, Reichley R, McKinnon PS (2010) Clinical, microbiologic, and genetic determinants of persistent methicillin-resistant Staphylococcus aureus bacteremia. Diagn Microbiol Infect Dis. https://doi.org/10.1016/j.diagmicrobio.2010.02.026
Yoon YK, Kim JY, Park DW, Sohn JW, Kim MJ (2010) Predictors of persistent methicillin-resistant Staphylococcus aureus bacteraemia in patients treated with vancomycin. J Antimicrob Chemother. https://doi.org/10.1093/jac/dkq050
Hawkins C, Huang J, Jin N, Noskin GA, Zembower TR, Bolon M (2007) Persistent Staphylococcus aureus bacteremia: an analysis of risk factors and outcomes. Arch Intern Med. https://doi.org/10.1001/archinte.167.17.1861
Khatib R, Johnson LB, Sharma M, Fakih MG, Ganga R, Riederer K (2009) Persistent Staphylococcus aureus bacteremia: incidence and outcome trends over time. Scand J Infect Dis. https://doi.org/10.1080/00365540802441711
Chong YP, Park SJ, Kim HS, Kim ES, Kim MN, Park KH, Kim SH, Lee SO, Choi SH, Jeong JY, Woo JH, Kim YS (2013) Persistent Staphylococcus aureus bacteremia: a prospective analysis of risk factors, outcomes, and microbiologic and genotypic characteristics of isolates. Medicine. https://doi.org/10.1097/MD.0b013e318289ff1e
Li L, Yeaman MR, Bayer AS, Xiong YQ (2019) Phenotypic and genotypic characteristics of methicillin-resistant Staphylococcus aureus (MRSA) related to persistent endovascular infection. Antibiotics. https://doi.org/10.3390/antibiotics8020071
Asgeirsson H, Kristjansson M, Kristinsson KG, Gudlaugsson O (2011) Staphylococcus aureus bacteraemia-nationwide assessment of treatment adequacy and outcome. J Infect. https://doi.org/10.1016/j.jinf.2011.03.003
Goto M, Schweizer ML, Vaughan-Sarrazin MS, Perencevich EN, Livorsi DJ, Diekema DJ, Richardson KK, Beck BF, Alexander B, Ohl ME (2017) Association of evidence-based care processes with mortality in Staphylococcus aureus bacteremia at Veterans Health Administration Hospitals, 2003–2014. JAMA Intern Med. https://doi.org/10.1001/jamainternmed.2017.3958
Paul M, Kariv G, Goldberg E, Raskin M, Shaked H, Hazzan R, Samra Z, Paghis D, Bishara J, Leibovici L (2010) Importance of appropriate empirical antibiotic therapy for methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother. https://doi.org/10.1093/jac/dkq373
Battle SE, Shuping M, Withers S, Justo JA, Bookstaver PB, Al-Hasan MN (2022) Prediction of mortality in Staphylococcus aureus bloodstream infection using quick Pitt bacteremia score. J Infect. https://doi.org/10.1016/j.jinf.2021.12.002
Goldstein B, Giroir B, Randolph A, International Consensus Conference on Pediatric Sepsis (2005) International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. https://doi.org/10.1097/01.PCC.0000149131.72248.E6
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections. Am J Infect Control 16:128–140
Brown DF, Edwards DI, Hawkey PM, Morrison D, Ridgway GL, Towner KJ, Wren MW, Joint Working Party of the British Society for Antimicrobial Chemotherapy, Hospital Infection Society, Infection Control Nurses Association (2005) Guidelines for the laboratory diagnosis and susceptibility testing of methicillin-resistant Staphylococcus aureus (MRSA). J Antimicrob Chemother. https://doi.org/10.1093/jac/dki372
Li Y, Li Q, Zhang G, Ma H, Wu Y, Yi Q, Jiang L, Wan J, Suo F, Luo Z (2019) Time to positivity of blood culture is a risk factor for clinical outcomes in Staphylococcus aureus bacteremia children: a retrospective study. BMC Infect Dis. https://doi.org/10.1186/s12879-019-3993-4
Tiwari LK, Singhi S, Jayashree M, Baranwal AK, Bansal A (2014) Hypoalbuminemia in critically sick children. Indian J Crit Care Med. https://doi.org/10.4103/0972-5229.140143
Chow JW, Yu VL (1999) Combination antibiotic therapy versus monotherapy for gram-negative bacteraemia: a commentary. Int J Antimicrob Agents. https://doi.org/10.1016/s0924-8579(98)00060-0
Guimaraes AO, Cao Y, Hong K, Mayba O, Peck MC, Gutierrez J, Ruffin F, Carrasco-Triguero M, Dinoso JB, Clemenzi-Allen A, Koss CA, Maskarinec SA, Chambers HF, Fowler VG, Baruch A, Rosenberger CM (2019) A prognostic model of persistent bacteremia and mortality in complicated Staphylococcus aureus bloodstream infection. Clin Infect Dis. https://doi.org/10.1093/cid/ciy739
Bisbe J, Gatell JM, Puig J, Mallolas J, Martinez JA, Jimenez de Anta MT, Soriano E (1988) Pseudomonas aeruginosa bacteremia: univariate and multivariate analyses of factors influencing the prognosis in 133 episodes. Rev Infect Dis. https://doi.org/10.1093/clinids/10.3.629
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. https://doi.org/10.1001/jama.2016.0287
Matics TJ, Sanchez-Pinto LN (2017) Adaptation and validation of a pediatric sequential organ failure assessment score and evaluation of the sepsis-3 definitions in critically ill children. JAMA Pediatr. https://doi.org/10.1001/jamapediatrics.2017.2352
Cardenas-Comfort C, Kaplan SL, Vallejo JG, McNeil JC (2020) Follow-up Blood Cultures in Children With Staphylococcus aureus Bacteremia. Pediatrics. https://doi.org/10.1542/peds.2020-1821
Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, Kaplan SL, Karchmer AW, Levine DP, Murray BE, Rybak MJ, Talan DA, Chambers HF; Infectious Diseases Society of America (2011) Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis. https://doi.org/10.1093/cid/ciq146
Chung H, Kim E, Yang E, Lee YW, Park JH, Bae S, Jung J, Kim MJ, Chong YP, Kim SH, Lee SO, Choi SH, Kim YS (2021) C-reactive protein predicts persistent bacteremia caused by community-acquired methicillin-resistant Staphylococcus aureus strain. Eur J Clin Microbiol Infect Dis. https://doi.org/10.1007/s10096-021-04303-5
Khatib R, Riederer K, Saeed S, Johnson LB, Fakih MG, Sharma M, Tabriz MS, Khosrovaneh A (2005) Time to positivity in Staphylococcus aureus bacteremia: possible correlation with the source and outcome of infection. Clin Infect Dis. https://doi.org/10.1086/432472
Plorde JJ, Tenover FC, Carlson LG (1985) Specimen volume versus yield in the BACTEC blood culture system. J Clin Microbiol. https://doi.org/10.1128/jcm.22.2.292-295.1985
Xu H, Cheng J, Yu Q, Li Q, Yi Q, Luo S, Li Y, Zhang G, Tian X, Cheng D, Luo Z (2020) Prognostic role of time to positivity of blood culture in children with Pseudomonas aeruginosa bacteremia. BMC Infect Dis. https://doi.org/10.1186/s12879-020-05257-3
Berestein MÁC, Salerno MC, Giralda RN, Ferrer ML, Gil MF, Fasano MV (2021) Metastatic infections in pediatric patients with Staphylococcus aureus bacteremia assisted at a children’s hospital in La Plata, Argentina. Arch Argent Pediatr. https://doi.org/10.5546/aap.2021.eng.408
Tande AJ, Palraj BR, Osmon DR, Berbari EF, Baddour LM, Lohse CM, Steckelberg JM, Wilson WR, Sohail MR (2016) Clinical presentation, risk factors, and outcomes of hematogenous prosthetic joint infection in patients with Staphylococcus aureus Bacteremia. Am J Med. https://doi.org/10.1016/j.amjmed.2015.09.006
Fowler VG Jr, Olsen MK, Corey GR, Woods CW, Cabell CH, Reller LB, Cheng AC, Dudley T, Oddone EZ (2003) Clinical identifiers of complicated Staphylococcus aureus bacteremia. Arch Intern Med. https://doi.org/10.1001/archinte.163.17.2066
Kim YS, Sol IS, Kim MJ, Kim SY, Kim JD, Kim YH, Kim KW, Sohn MH, Kim KE (2017) Serum albumin as a biomarker of poor prognosis in the pediatric patients in intensive care unit. Korean J Crit Care Med. https://doi.org/10.4266/kjccm.2017.00437
Tsai CY, Lee CH, Chen IL (2021) Teicoplanin versus β-lactam for febrile patients with Staphylococcus-like bacteremia: focus on methicillin-susceptible Staphylococcus aureus bacteremia. BMC Infect Dis. https://doi.org/10.1186/s12879-021-06111-w
Minejima E, Wang J, Boettcher S, Liu L, Lou M, She RC, Wenzel SL, Spellberg B, Wong-Beringer A (2022) Distance between home and the admitting hospital and its effect on survival of low socioeconomic status population with Staphylococcus aureus bacteremia. Public Health Rep. https://doi.org/10.1177/0033354921994897
Funding
This work was supported by the National Key Clinical specialty fund (grant 2011–873).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by XM W, X Z, ZY G, QY L, GL Z, XY T, and DP C. The first draft of the manuscript was written by XM W and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of Children’s Hospital of Chongqing Medical University (File No. (2022)187). Informed consent was obtained from the parents in written form when children were admitted to the hospital. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Formal consent is not required because this was a retrospective evaluation of already collected data.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Tobias Tenenbaum
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, X., Guo, Z., Zhang, X. et al. Inappropriate empirical antibiotic therapy was an independent risk factor of pediatric persistent S. aureus bloodstream infection. Eur J Pediatr 182, 719–729 (2023). https://doi.org/10.1007/s00431-022-04729-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04729-9