Abstract
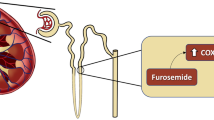
We aimed at establishing the state of the art in fluid restriction practice in our national setting and providing a foundation for future research efforts. A prospective cross-sectional survey was conducted among all 114 Italian Neonatal Units in order to address conservative management of patent ductus arteriosus (PDA) in preterm infants below 29 weeks’ gestational age (GA), with specific regard to fluid restriction. Response rate was 80%. Conservative measures for PDA management are provided in the majority of NICUs and 80% of centers reduce fluid intake in neonates with PDA. No relationship can be found among pharmacologically or surgically treated patients per year and the approach to fluid restriction. The minimum intake administered at regimen when fluid restriction is applied is associated to the ratio between the maximum number of neonates managed pharmacologically and number of admitted < 29 weeks’ GA newborns.
Conclusion: Our survey shows an extreme variability among centers in terms of use of fluid restriction as a prophylactic tool but also in terms of its use (both opportunity and modality) when a hemodynamically significant PDA is diagnosed. This variability, that can be also found in randomized trials and observational studies, suggests that further evidence is needed to better understand its potential beneficial effects and its potential harms such as dehydration, hypotension, decreased end-organ perfusion, and reduced caloric intake.
What is Known: • The lack of demonstrable improvement following the treatment of patent ductus arteriosus has recently paved the way to a more conservative approach. • Fluid restriction is the most commonly applied conservative treatment of PDA. | |
What is New: • Among Italian NICUs an extreme variability in terms of indications, timing and modalities of application of Fluid restriction can be found. • This variability reflects the lack of standardization of this practice and the contrasting evidence on its efficacy. |




Similar content being viewed by others
Abbreviations
- BPD:
-
Bronchopulmonary dysplasia
- DOL:
-
Day of life
- ELBW:
-
Extremely low birthweight
- FO:
-
Fluid overload
- FR:
-
Fluid restriction
- GA:
-
Gestational age
- HSPDA:
-
Hemodynamically significant patent ductus arteriosus
- ISGNC:
-
The Italian Study Group of Neonatal Cardiology
- ISN:
-
Italian Society of Neonatology
- IVH:
-
Intraventricular hemorrhage
- NEC:
-
Necrotizing enterocolitis
- NICU:
-
Neonatal intensive care unit
- OR:
-
Odds ratio
- PEEP:
-
Positive end expiratory pressure
- PDA:
-
Patent ductus arteriosus
- PVL:
-
Periventricular leukomalacia
- RCT:
-
Randomized controlled trial
- VLBWI:
-
Very low birthweight infants
References
Evans N (2015) Preterm patent ductus arteriosus: a continuing conundrum for the neonatologist? Semin Fetal Neonatal Med 20(4):272–277
Herrman K, Bose C, Lewis K, Laughon M (2009) Spontaneous closure of the patent ductus arteriosus in very low birth weight infants following discharge from the neonatal unit. Arch Dis Child Fetal Neonatal Ed 94(1):F48-50
Weber SC, Weiss K, Buhrer C, Hansmann G, Koehne P, Sallmon H (2015) Natural history of patent ductus arteriosus in very low birth weight infants after discharge. J Pediatr 167(5):1149–1151
Nemerofsky SL, Parravicini E, Bateman D, Kleinman C, Polin RA, Lorenz JM (2008) The ductus arteriosus rarely requires treatment in infants >1000 grams. Am J Perinatol 25(10):661–666
Semberova J, Sirc J, Miletin J, Kucera J, Berka I, Sebkova S, O'Sullivan S, Franklin O, Stranak Z (2017) Spontaneous closure of patent Ductus Arteriosus in infants ≤1500 g. Pediatrics. 140(2):e20164258. https://doi.org/10.1542/peds.2016-4258
Bose CL, Laughon M (2006) Treatment to prevent patency of the ductus arteriosus: beneficial or harmful? J Pediatr 148(6):713–714
Bose CL, Laughon MM (2007) Patent ductus arteriosus: lack of evidence for common treatments. Arch Dis Child Fetal Neonatal Ed 92(6):F498-502
Laughon MM, Simmons MA, Bose CL (2004) Patency of the ductus arteriosus in the premature infant: is it pathologic? Should it be treated? Curr Opin Pediatr 16(2):146–151
Benitz WE (2010) Treatment of persistent patent ductus arteriosus in preterm infants: time to accept the null hypothesis? J Perinatol Official J California Perinatal Assoc 30(4):241–252
Benitz WE (2011) Learning to live with patency of the ductus arteriosus in preterm infants. J Perinatol Official J California Perinatal Assoc 31(Suppl 1):S42–S48
Benitz WE (2012) Patent ductus arteriosus: to treat or not to treat? Arch Dis Child Fetal Neonatal Ed 97(2):F80–F82
Benitz WE (2016) Committee on F Newborn AAoP. Patent ductus arteriosus in preterm infants. Pediatrics 137(1):e20153730
Clyman RI, Couto J, Murphy GM (2012) Patent ductus arteriosus: are current neonatal treatment options better or worse than no treatment at all? Semin Perinatol 36(2):123–129
Jain A, Shah PS (2015) Diagnosis, evaluation, and management of patent ductus arteriosus in preterm neonates. JAMA Pediatr 169(9):863–872
Perez KM, Laughon MM (2015) What is new for patent ductus arteriosus management in premature infants in 2015? Curr Opin Pediatr 27(2):158–164
Sallmon H, Koehne P, Hansmann G (2016) Recent advances in the treatment of preterm newborn infants with patent ductus arteriosus. Clin Perinatol 43(1):113–129
Mitra S, Florez ID, Tamayo ME, Mbuagbaw L, Vanniyasingam T, Veroniki AA, Zea AM, Zhang Y, Sadeghirad B, Thabane L (2018) Association of placebo, indomethacin, ibuprofen, and acetaminophen with closure of hemodynamically significant patent ductus arteriosus in preterm infants a systematic review and meta-analysis. JAMA 319(12):1221–1238
Hundscheid T, El-Khuffash A, McNamara PJ, de Boode WP (2022) Survey highlighting the lack of consensus on diagnosis and treatment of patent ductus arteriosus in prematurity. Eur J Pediatr. https://doi.org/10.1007/s00431-022-04441-8. Epub ahead of print. PMID: 35305143.
Ngo S, Profit J, Gould JB, Lee HC (2017) Trends in patent ductus arteriosus diagnosis and management for very low birth weight infants. Pediatrics 139:e20162390. https://doi.org/10.1542/peds.2016-2390
Bell EF, Acarregui MJ (2014) Restricted versus liberal water intake for preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev (12):CD000503. https://doi.org/10.1002/14651858.CD000503.pub3
Eysenbach G (2004) Improving the quality of web surveys: the checklist for reporting results of internet E-surveys. J Med Internet Res 6(3):e34
Kavvadia V, Greenough A, Dimitriou G, Forsling ML (2000) Randomized trial of two levels of fluid input in the perinatal period–effect on fluid balance, electrolyte and metabolic disturbances in ventilated VLBW infants. Acta Paediatr 89(2):237–241. https://doi.org/10.1080/080352500750028898. PMID: 10709897
Vanhaesebrouck S, Zonnenberg I, Vandervoort P, Bruneel E, Van Hoestenberghe MR, Theyskens C (2007) Conservative treatment for patent ductus arteriosus in the preterm. Arch Dis Child Fetal Neonatal Ed 92:F244–F247. https://doi.org/10.1136/adc.2006.104596
Ficial et al (2020) Survey of PDA management in very low birth weight infants across Italy. Ital J Pediatr 46:22
Hundscheid T, Jansen EJS, Onland W, Kooi EMW, Andriessen P, de Boode WP (2021) Conservative management of patent ductus arteriosus in preterm infants—a systematic review and meta-analyses assessing differences in outcome measures between randomized controlled trials and cohort studies. Front Pediatr 9:626261. https://doi.org/10.3389/fped.2021.626261
Ohlsson A, Shah PS (2020) Paracetamol (acetaminophen) for patent ductus arteriosus in preterm or low birth weight infants. Cochrane Database Syst Rev (1):CD010061
Ohlsson A, Shah SS (2020) Ibuprofen for the prevention of patent ductus arteriosus in preterm and/or low birth weight infants. Cochrane Database Syst Rev (1):CD004213
Clyman RI, Liebowitz M, Kaempf J et al (2019) PDA-TOLERATE (PDA: TO LEave it alone or Respond And Treat Early) trial investigators. PDA-TOLERATE trial: an exploratory randomized controlled trial of treatment of moderate-to-large patent ductus arteriosus at 1 week of age. J Pediatr 205:41–48.e6
Liebowitz M, Katheria A, Sauberan J et al (2019) PDA-TOLERATE (PDA: TOLEave it alone or Respond And Treat Early) Trial Investigators. Lack of equipoise in the PDA-TOLERATE trial: a comparison of eligible infants enrolled in the trial and those treated outside the trial. J Pediatr 213:222–226.e2
Schena F, Francescato G, Cappelleri A, Picciolli I, Mayer A, Mosca F, Fumagalli M (2015) Association between hemodynamically significant patent ductus arteriosus and bronchopulmonary dysplasia. J Pediatr 166(6):1488–1492. https://doi.org/10.1016/j.jpeds.2015.03.012. Epub 2015 Apr 14 PMID: 25882876
Mayer A, Francescato G, Pesenti N, Schena F, Mosca F (2022) Patent ductus arteriosus and spontaneous intestinal perforation in a cohort of preterm infants. J Perinatol. https://doi.org/10.1038/s41372-022-01403-8. Epub ahead of print. PMID: 35589970
Hundscheid T, Onland W, van Overmeire B, Dijk P, van Kaam AH, Dijkman KP, Kooi EM, Villamor E, Kroon AA, Visser R, Vijlbrief DC, de Tollenaer SM, Cools F, van Laere D, Johansson AB, Hocq C, Zecic A, Adang E, Donders R, de Vries W, van Heijst AF, de Boode WP (2018) Early treatment versus expectative management of patent ductus arteriosus in preterm infants: a multicentre, randomised, non-inferiority trial in Europe (BeNeDuctus trial). BMC Pediatr 18(1):262–262
Bell EF, Warburton D, Stonestreet BS, Oh W (1980) Effect of fluid administration on the development of symptomatic patent ductus arteriosus and congestive heart failure in premature infants. New Engl J Med 302:598‐604. [MEDLINE: 1980099478]
Kavvadia V, Greenough A, Dimitriou G, Hooper R (1999) Comparison of the effect of two fluid input regimens on perinatal lung function in ventilated infants of very low birth weight. Eur J Pediatr 158(11):917–922
Lorenz JM, Kleinman LI, Kotagal UR, Reller MD (1982) Water balance in very low-birth-weight infants: relationship to water and sodium intake and effect on outcome. J Pediatr 101:423–432
Tammela OKT, Koivisto ME (1992) Fluid restriction for preventing bronchopulmonary dysplasia? Reduced fluid intake during the first weeks of life improves the outcome of low-birth-weight infants. Acta Paediatr 81:207–212
Bell EF, Warburton D, Stonestreet BS, Oh W (1980) Effect of fluid administration on the development of symptomatic patent ductus arteriosus and congestive heart failure in premature infants. New Engl J Med 302:598‐604. [MEDLINE: 1980099478]
Stephens BE, Gargus RA, Walden RV, Mance M, Nye J, McKinley L et al (2008) Fluid regimens in the first week of life may increase risk of patent ductus arteriosus in extremely low birth weight infants. J Perinatol 28:123–128. https://doi.org/10.1038/sj.jp.7211895
De Buyst J, Rakza T, Pennaforte T, Johansson AB, Storme L (2012) Hemodynamic effects of fluid restriction in preterm infants with significant patent ductus arteriosus. J Pediatr 161:404–408
Levinson MB, Messina C, Mintzer JP (2018) Fluid management during the first postnatal day in very low birth weight neonates and rates of patent ductus arteriosus requiring treatment. J Matern Fetal Neonatal Med 31(20):2699–2704. https://doi.org/10.1080/14767058.2017.1353968. Epub 2017 Jul 24 PMID: 28691556
Hansson L, Lind T, Wiklund U, Öhlund I, Rydberg A (2019) Fluid restriction negatively affects energy intake and growth in very low birthweight infants with haemodynamically significant patent ductus arteriosus. Acta Paediatr 108(11):1985–1992. https://doi.org/10.1111/apa.14815. Epub 2019 May 23 PMID: 30980416
Diderholm B, Normann E, Ahlsson F, Sindelar R, Ågren J (2022) The impact of restricted versus liberal early fluid volumes on plasma sodium, weight change, and short-term outcomes in extremely preterm infants. Nutrients 14:795. https://doi.org/10.3390/nu14040795
Author information
Authors and Affiliations
Contributions
Gaia Francescato, Iuri Corsini, Benjamim Ficial, Rosamaria Cerbo, Stefano Fiocchi, Marilena Savoia, and Sabrina Salvadori contributed to study conception and design. Material preparation, data collection, and analysis were performed by Gaia Francescato, Iuri Corsini, Federico Matina, Fabio Mizzoni, Daniela Doni, Irma Capolupo, and Gregorio Milani. The first draft of the manuscript was written by Gaia Francescato, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Francescato, G., Capolupo, I., Cerbo, R.M. et al. Fluid restriction in management of patent ductus arteriosus in Italy: a nationwide survey. Eur J Pediatr 182, 393–401 (2023). https://doi.org/10.1007/s00431-022-04685-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04685-4