Abstract
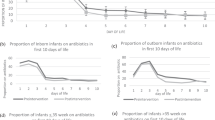
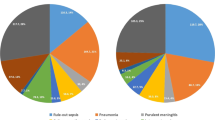
To evaluate the safety and effectiveness of evidence-based antibiotic stewardship in a neonatal unit in China. The study period consisted of two phases, one retrospective (the baseline period, January to December 2018, and the transition period, January 2019 to August 2020) and one prospective intervention period (September 2020 to August 2021). During the prospective period, evidence-based antibiotic stewardship was applied to neonates with suspected infections, pneumonia, and culture-negative sepsis. The antibiotic stewardship included the observation form of neonatal infections, antibiotic therapy of no more than 48 h for suspected infections, and 5 days for pneumonia and culture-negative sepsis. The change in antibiotic use measured by days of therapy per 1000 patient-days between the baseline and intervention period was analyzed. Safety outcomes included reinitiation of antibiotics within 14 days, length of stay, occurrence of late-onset sepsis and necrotizing enterocolitis (Bell stage ≥ II), multidrug-resistant organism infections, and mortality. A total of 7705 neonates were enrolled during the baseline (n = 4804) and the intervention periods (n = 2901). The total antibiotic usage during the baseline period was 771 days of therapy per 1000 patient-days, while that was 525 days of therapy per 1000 patient-days during the intervention period, indicating a 32% decrease in antibiotic consumption. No significant difference in safety outcomes was observed between the baseline and intervention period (P > 0.05), whereas the length of stay was longer during the intervention period (P < 0.001).
Conclusion: The evidence-based antibiotic stewardship can safely and effectively reduce antibiotic use and shorten the duration of therapy in the neonatal unit.
What is Known: • Overuse of antibiotics has been associated with adverse events in neonates, including necrotizing enterocolitis, multidrug-resistant organism infections, and death. • More clinical effectiveness evidence is needed to support antibiotic stewardship of neonates in China. | |
What is New: • Using prospective audit, targeted stewardship interventions, this study shows that a 32% reduction in overall antibiotic consumption was achieved safely. • Implementation of evidence-based neonatal antibiotic stewardship, including the observation form of neonatal infections, antibiotic therapy of no more than 48 h for suspected infections, and 5 days for pneumonia and culture-negative sepsis, is safe and effective among newborns in a developing country. |




Similar content being viewed by others
Abbreviations
- CHCMU:
-
Children’s Hospital of Chongqing Medical University
- CRP:
-
C-reactive protein
- DW:
-
Durbin-Watson method
- EOS:
-
Early-onset sepsis
- LOS:
-
Late-onset sepsis
- NEC:
-
Necrotizing enterocolitis
- PCT:
-
Procalcitonin
References
Hsieh EM, Hornik CP, Clark RH, Laughon MM, Benjamin DK Jr, Smith BP (2014) Medication use in the neonatal intensive care unit. Am J Perinatol 31:811–821. https://doi.org/10.1055/s-0033-1361933
Clark RH, Bloom BT, Spitzer AR, Gerstmann DR (2006) Reported medication use in the neonatal intensive care unit: data from a large national data set. Pediatrics 117:1979–1987. https://doi.org/10.1542/peds.2005-1707
Gkentzi D, Kortsalioudaki C, Cailes BC, Zaoutis T, Kopsidas J, Tsolia M, Spyridis N, Siahanidou S, Sarafidis K, Heath PT et al (2019) Epidemiology of infections and antimicrobial use in Greek neonatal units. Arch Child Fetal Neonatal Ed 104:F293–F297. https://doi.org/10.1136/archdischild-2018-315024
Ting JY, Synnes A, Roberts A, Deshpandey A, Dow K, Yoon EW, Lee KS, Dobson S, Lee SK, Shah PS et al (2016) Association between antibiotic use and neonatal mortality and morbidities in very low-birth-weight infants without culture-proven sepsis or necrotizing enterocolitis. JAMA Pediatr 170:1181–1187. https://doi.org/10.1001/jamapediatrics.2016.2132
Cotten CM, Taylor S, Stoll B, Goldberg RN, Hansen NI, Sánchez PJ, Ambalavanan N, Benjamin Jr DK, NICHD Neonatal Research Network (2009) Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics 123:58–66. https://doi.org/10.1542/peds.2007-3423
Cotten CM, McDonald S, Stoll B, Goldberg RN, Poole K, Benjamin DK Jr (2006) The association of third-generation cephalosporin use and invasive candidiasis in extremely low birth-weight infants. Pediatrics 118:717–722. https://doi.org/10.1542/peds.2005-2677
Novitsky A, Tuttle D, Locke RG, Saiman L, Mackley A, Paul DA (2015) Prolonged early antibiotic use and bronchopulmonary dysplasia in very low birth weight infants. Am J Perinatol 32:43–48. https://doi.org/10.1055/s-0034-1373844
Kummeling I, Stelma FF, Dagnelie PC, Snijders BEP, Penders J, Huber M, van Ree R, van den Brandt PA, Thijs C (2007) Early life exposure to antibiotics and the subsequent development of eczema, wheeze, and allergic sensitization in the first 2 years of life: the KOALA Birth Cohort Study. Pediatrics 119:e225-231. https://doi.org/10.1542/peds.2006-0896
Gerber JS, Bryan M, Ross RK, Daymont C, Parks EP, Localio AR, Grundmeier RW, Stallings VA, Zaoutis TE (2016) Antibiotic exposure during the first 6 months of life and weight gain during childhood. JAMA 315:1258–1265. https://doi.org/10.1001/jama.2016.2395
The President’s Council of Advisors on Science and Technology (2014) Report to the president on combating antibiotic resistance. https://www.cdc.gov/drugresistance/pdf/report-to-the-president-on-combating-antibiotic-resistance.pdf. Accessed 16 Apr 2021
Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, Srinivasan A, Dellit TH, Falck-Ytter YT, Fishman NO et al (2016) Implementing an antibiotic stewardship program: guidelines by the infectious diseases society of america and the society for healthcare epidemiology of America. Clin Infect Dis 62:e51-77. https://doi.org/10.1093/cid/ciw118
World Health Organization (2015) Global action plan on antimicrobial resistance. http://www.who.int/antimicrobial-resistance/publications/global-action-plan/en/. Accessed 16 Apr 2021
Xiao Y, Zhang J, Zheng B, Zhao L, Li S, Li L (2013) Changes in Chinese policies to promote the rational use of antibiotics. PLoS Med 10:e1001556. https://doi.org/10.1371/journal.pmed.1001556
Ouldali N, Bellêttre X, Milcent K, Guedj R, de Pontual L, Cojocaru B, Soussan-Banini V, Craiu I, Skurnik D, Gajdos V et al (2017) Impact of implementing national guidelines on antibiotic prescriptions for acute respiratory tract infections in pediatric emergency departments: an interrupted time series analysis. Clin Infect Dis 65:1469–1476. https://doi.org/10.1093/cid/cix590
McCarthy KN, Hawke A, Dempsey EM (2018) Antimicrobial stewardship in the neonatal unit reduces antibiotic exposure. Acta Paediatr 107:1716–1721. https://doi.org/10.1111/apa.14337
Li H, Gong Y, Han J, Zhang S, Chen S, Xu X, Lu Z, Yin X (2020) Interrupted time-series analysis to evaluate the impact of a national antimicrobial stewardship campaign on antibiotic prescribing: a typical practice in China’s primary care. Clin Infect Dis. https://doi.org/10.1093/cid/ciaa962
Fu P, Wang C, Yu H, Xu H, Jing C, Deng J, Zhao R, Hua C, Chen Y, Chen X et al (2019) Antimicrobial resistance profile of clinical isolates in pediatric hospitals in China: report from the ISPED Surveillance Program, 2018. Chin J Evid Based Pediatr 14:321–326 (Chinese)
The Subspecialty Group of Neonatology, the Society of Pediatric, Chinese Medical Association, The Editorial Board of Chinese Journal of Pediatrics (2003) Protocol for diagnosis and treatment of neonatal septicemia. Chin J Pediatr 41:897–899. https://doi.org/10.3760/cma.j.issn.0578-1310.2003.12.106.Chinese
Shao X, Ye H, Qiu X (2010) Practice of Neonatology, 4th edn. People’s Medical Publishing House, Beijing (Chinese)
He Y, Chen F, Zhang Y, Xiang L, Liu Y, Hua Z (2020) C-reactive protein-guided antibiotic treatment strategy for neonates with suspected early-onset sepsis. Chin J Contemp Pediatr 22:12–16 (Chinese)
Stocker M, Fontana M, El Helou S, Wegscheider K, Berger TM (2010) Use of procalcitonin-guided decision-making to shorten antibiotic therapy in suspected neonatal early-onset sepsis: prospective randomized intervention trial. Neonatology 97:165–174. https://doi.org/10.1159/000241296
Ho T, Dukhovny D, Zupancic JAF, Goldmann DA, Horbar JD, Pursley DM (2015) Choosing wisely in newborn medicine: five opportunities to increase value. Pediatrics 136:e482-489. https://doi.org/10.1542/peds.2015-0737
Cantey JB, Wozniak PS, Pruszynski JE, Sánchez PJ (2016) Reducing unnecessary antibiotic use in the neonatal intensive care unit (SCOUT): a prospective interrupted time-series study. Lancet Infect Dis 16:1178–1184. https://doi.org/10.1016/S1473-3099(16)30205-5
The Subspecialty Group of Neonatology, the Society of Pediatric, Professional Committee of Infectious Diseases, Neonatology Society (2019) Expert consensus on the diagnosis and management of neonatal sepsis (version 2019). Chin J Pediatr 57:252–257. https://doi.org/10.3760/cma.j.issn.0578-1310.2019.04.005.Chinese
Ibrahim OM, Polk RE (2014) Antimicrobial use metrics and benchmarking to improve stewardship outcomes: methodology, opportunities, and challenges. Infect Clin North Am 28:195–214. https://doi.org/10.1016/j.idc.2014.01.006
Liu X, Yang J, Chen X, Hua Z (2016) Effects of antibiotic stewardship on neonatal bloodstream infections. Chin J Contemp Pediatr 18:796–801 (Chinese)
Stocker M, van Herk W, El Helou S, Dutta S, Fontana MS, Schuerman FABA, van den Tooren-de Groot RK, Wieringa JW, Janota J, van der Meer-Kappelle LH et al (2017) Procalcitonin-guided decision making for duration of antibiotic therapy in neonates with suspected early-onset sepsis: a multicentre, randomised controlled trial (NeoPIns). Lancet 390:871–881. https://doi.org/10.1016/S0140-6736(17)31444-7
National Collaborating Centre for Women’s and Children’s Health (UK) (2012) Antibiotics for early-onset neonatal infection: antibiotics for the prevention and treatment of early-onset neonatal infection. RCOG Press, London
Cantey JB, Wozniak PS, Sánchez PJ (2015) Prospective surveillance of antibiotic use in the neonatal intensive care unit: results from the SCOUT study. Pediatr Infect J 34:267–272. https://doi.org/10.1097/INF.0000000000000542
Garcia-Prats JA, Cooper TR, Schneider VF, Stager CE, Hansen TN (2000) Rapid detection of microorganisms in blood cultures of newborn infants utilizing an automated blood culture system. Pediatrics 105:523–527. https://doi.org/10.1542/peds.105.3.523
Carr D, Barnes EH, Gordon A, Isaacs D (2017) Effect of antibiotic use on antimicrobial antibiotic resistance and late-onset neonatal infections over 25 years in an Australian tertiary neonatal unit. Arch Child Fetal Neonatal Ed 102:F244–F250. https://doi.org/10.1136/archdischild-2016-310905
Lu C, Liu Q, Yuan H, Wang L (2019) Implementation of the smart use of antibiotics program to reduce unnecessary antibiotic use in a neonatal icu: a prospective interrupted time-series study in a developing country. Crit Care Med 47:e1–e7. https://doi.org/10.1097/CCM.0000000000003463
Funding
This study was supported by grants from the Clinical Research Project of Children’s Hospital of Chongqing Medical University (grant number YBXM 2019–007). The funder had no involvement in the preparation of data or the manuscript.
Author information
Authors and Affiliations
Contributions
Kun Feng conceptualized and designed this study, performed data collection, analysis, and visualization, and contributed to writing the draft and revising the manuscript. Yunyan He and Xinyin Zhang contributed to conceptualization, data collection, and to writing the original draft. Weiqin Liu contributed to conceptualization, data analysis and visualization, and to revising the manuscript. Ping Song contributed to conceptualization, data collection, and reviewed the manuscript. Ziyu Hua supervised the study design, acquired the funding, conceptualized this study, contributed to data analysis and revised the manuscript. All authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Ethics approval
The Institutional Review Board of CHCMU approved the study (Approval No. 2020–197-1) with a waiver of informed consent.
Consent statement
Patient consent was not required.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Feng, K., He, Y., Liu, W. et al. Evaluation of antibiotic stewardship among near-term and term infants admitted to a neonatal unit. Eur J Pediatr 182, 245–254 (2023). https://doi.org/10.1007/s00431-022-04668-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04668-5