Abstract
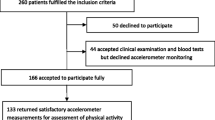
In addition to disease-specific complications, juvenile idiopathic arthritis (JIA) has been linked to metabolic impairments in adults. Recent data supported the usefulness of uric acid (UA) as risk factor for cardiometabolic derangements. Given the lack of pediatric evidence in this field, we aimed to explore this association in a cohort of children diagnosed with JIA. We retrospectively evaluated 113 children diagnosed with JIA classified according to the International League of Association for Rheumatology (ILAR) criteria attending our Rheumatology Clinic. Both clinical and biochemical assessments were performed. Participants were stratified in four groups according to quartiles of serum UA. Disease activity was calculated by the Juvenile Arthritis Disease Activity Score 10 (JADAS-10) joint reduced count, and cut-offs for disease states were applied. Patients belonging to the highest UA quartile showed higher serum triglycerides, total cholesterol, creatinine, and glucose levels (p = 0.01, p = 0.025, p = 0.04, and p = 0.005, respectively) and lower HDL cholesterol values (p < 0.0001) than subjects belonging to the lowest quartiles. Ferritin, erythrocyte sedimentation rate levels, and age at disease onset did not significantly differ across UA quartiles (all p > 0.05). As activity disease index, JADAS-10 score significantly increased across UA quartiles (p = 0.009).
Conclusion: Children with JIA presented with a worse cardiometabolic profile and a greater disease severity across UA quartiles. Our findings suggest that in clinical practice, UA might represent a useful marker of cardiometabolic risk and disease severity in children with JIA.
What is Known: • JIA has been linked to metabolic derangements in adulthood. • UA has been recognized as a marker of cardiometabolic risk both in adults and children. | |
What is New: • Children with JIA belonging to the highest UA quartile showed a worse cardiometabolic profile and a greater disease severity. • UA might represent a helpful marker not only of cardiometabolic risk but also of disease severity in children with JIA. |
Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- BMI:
-
Body mass index
- CVD:
-
Cardiovascular disease
- DMARDs:
-
Disease-modifying anti-rheumatic drugs
- ILAR:
-
International League of Association for Rheumatology
- IR:
-
Insulin resistance
- JIA:
-
Juvenile idiopathic arthritis
- JADAS-10:
-
Juvenile Arthritis Disease Activity Score 10
- MetS:
-
Metabolic syndrome
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- T2D:
-
Type 2 diabetes
- UA:
-
Uric acid
References
Ravelli A, Martini A (2007) Juvenile idiopathic arthritis. Lancet 369(9563):767–778
Petty RE, Southwood TR, Manners P et al (2004) International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol 31(2):390–392
Ringold S, Weiss PF, Beukelman T et al (2013) 2013 update of the 2011 American College of Rheumatology recommendations for the treatment of juvenile idiopathic arthritis: recommendations for the medical therapy of children with systemic juvenile idiopathic arthritis and tuberculosis screening among children receiving biologic medications. Arthritis Rheum 65(10):2499–2512
Beukelman T, Patkar NM, Saag KG et al (2011) 2011 American College of Rheumatology recommendations for the treatment of juvenile idiopathic arthritis: initiation and safety monitoring of therapeutic agents for the treatment of arthritis and systemic features. Arthritis Care Res (Hoboken) 63(4):465–482
Espinosa M, Gottlieb BS (2012) Juvenile idiopathic arthritis. Pediatr Rev 33(7):303–313
Sule S, Fontaine K (2018) Metabolic syndrome in adults with a history of juvenile arthritis. Open Access Rheumatol 10:67–72
Zanette Cde A, Machado SH, Brenol JC, Xavier RM (2010) Metabolic syndrome and juvenile idiopathic arthritis. Rev Bras Reumatol 50(2):190–204
Lv Q, Meng XF, He FF et al (2013) High serum uric acid and increased risk of type 2 diabetes: a systemic review and meta-analysis of prospective cohort studies. PLoS ONE 8(2):e56864
Yuan H, Yu C, Li X et al (2015) Serum uric acid levels and risk of metabolic syndrome: a dose-response meta-analysis of prospective studies. J Clin Endocrinol Metab 100(11):4198–4207
Richette P, Perez-Ruiz F (2013) Serum uric acid and metabolic risk. Curr Med Res Opin 29(Suppl 3):9–15
Russo E, Leoncini G, Esposito P, Garibotto G, Pontremoli R, Viazzi F (2020) Fructose and uric acid: major mediators of cardiovascular disease risk starting at pediatric age. Int J Mol Sci 21(12)
Shi Q, Wang R, Zhang H, Shan Y, Ye M, Jia B (2021) Association between serum uric acid and cardiovascular disease risk factors in adolescents in America: 2001–2018. PLoS ONE 16(8):e0254590
Di Bonito P, Valerio G, Licenziati MR et al (2021) Uric acid, impaired fasting glucose and impaired glucose tolerance in youth with overweight and obesity. Nutr Metab Cardiovasc Dis 31(2):675–680
Goli P, Riahi R, Daniali SS, Pourmirzaei M, Kelishadi R (2020) Association of serum uric acid concentration with components of pediatric metabolic syndrome: a systematic review and meta-analysis. J Res Med Sci 25:43
Ford ES, Li C, Cook S, Choi HK (2007) Serum concentrations of uric acid and the metabolic syndrome among US children and adolescents. Circulation 115(19):2526–2532
Di Bonito P, Valerio G, Licenziati MR et al (2022) Uric acid versus metabolic syndrome as markers of fatty liver disease in young people with overweight/obesity. Diabetes Metab Res Rev e3559
Giani T, De Masi S, Maccora I et al (2019) The influence of overweight and obesity on treatment response in juvenile idiopathic arthritis. Front Pharmacol 10:637
Diaz-Cordoves Rego G, Nunez-Cuadros E, Mena-Vazquez N et al (2021) Adiposity is related to inflammatory disease activity in juvenile idiopathic arthritis. J Clin Med 10(17)
Di Bonito P, Pacifico L, Licenziati MR et al (2020) Elevated blood pressure, cardiometabolic risk and target organ damage in youth with overweight and obesity. Nutr Metab Cardiovasc Dis 30(10):1840–1847
Di Sessa A, Umano GR, Cirillo G et al (2020) The rs72613567: TA variant in the hydroxysteroid 17-beta dehydrogenase 13 gene reduces liver damage in obese children. J Pediatr Gastroenterol Nutr 70(3):371–374
Ravelli A, Consolaro A, Horneff G et al (2018) Treating juvenile idiopathic arthritis to target: recommendations of an international task force. Ann Rheum Dis 77(6):819–828
Consolaro A, Ruperto N, Bazso A et al (2009) Development and validation of a composite disease activity score for juvenile idiopathic arthritis. Arthritis Rheum 61(5):658–666
Consolaro A, Bracciolini G, Ruperto N et al (2012) Remission, minimal disease activity, and acceptable symptom state in juvenile idiopathic arthritis: defining criteria based on the juvenile arthritis disease activity score. Arthritis Rheum 64(7):2366–2374
Dessein PH, Tobias M, Veller MG (2006) Metabolic syndrome and subclinical atherosclerosis in rheumatoid arthritis. J Rheumatol 33(12):2425–2432
Chung CP, Oeser A, Solus JF et al (2008) Prevalence of the metabolic syndrome is increased in rheumatoid arthritis and is associated with coronary atherosclerosis. Atherosclerosis 196(2):756–763
Tagi VM, Samvelyan S, Chiarelli F (2020) Treatment of metabolic syndrome in children. Horm Res Paediatr 93(4):215–225
Gesteiro E, Megia A, Guadalupe-Grau A, Fernandez-Veledo S, Vendrell J, Gonzalez-Gross M (2021) Early identification of metabolic syndrome risk: a review of reviews and proposal for defining pre-metabolic syndrome status. Nutr Metab Cardiovasc Dis 31(9):2557–2574
Borghi C, Agabiti-Rosei E, Johnson RJ et al (2020) Hyperuricaemia and gout in cardiovascular, metabolic and kidney disease. Eur J Intern Med 80:1–11
Feig DI (2009) Uric acid: a novel mediator and marker of risk in chronic kidney disease? Curr Opin Nephrol Hypertens 18(6):526–530
Luciano R, Shashaj B, Spreghini M et al (2017) Percentiles of serum uric acid and cardiometabolic abnormalities in obese Italian children and adolescents. Ital J Pediatr 43(1):3
Guzman J, Kerr T, Ward LM et al (2017) Growth and weight gain in children with juvenile idiopathic arthritis: results from the ReACCh-Out cohort. Pediatr Rheumatol Online J 15(1):68
Merwin S, Mackey E, Sule S (2021) US NHANES Data 2013–2016: increased risk of severe obesity in individuals with history of juvenile idiopathic arthritis. Pediatr Rheumatol Online J 19(1):119
Schenck S, Niewerth M, Sengler C et al (2015) Prevalence of overweight in children and adolescents with juvenile idiopathic arthritis. Scand J Rheumatol 44(4):288–295
Dixon JB (2010) The effect of obesity on health outcomes. Mol Cell Endocrinol 316(2):104–108
Gicchino MF, Di Sessa A, Guarino S, Miraglia Del Giudice E, Olivieri AN, Marzuillo P (2021) Prevalence of and factors associated to chronic kidney disease and hypertension in a cohort of children with juvenile idiopathic arthritis. Eur J Pediatr 180(2):655–661
Al-Daghri NM, Al-Attas OS, Wani K, Sabico S, Alokail MS (2017) Serum uric acid to creatinine ratio and risk of metabolic syndrome in Saudi type 2 diabetic patients. Sci Rep 7(1):12104
Silva NR, Goncalves CET, Goncalves DLN, Cotta RMM, da Silva LS (2021) Association of uric acid and uric acid to creatinine ratio with chronic kidney disease in hypertensive patients. BMC Nephrol 22(1):311
Harlan WR, Cornoni-Huntley J, Leaverton PE (1979) Physiologic determinants of serum urate levels in adolescence. Pediatrics 63(4):569–575
Dai C, Wang C, Xia F et al (2021) Age and gender-specific reference intervals for uric acid level in children aged 5–14 years in Southeast Zhejiang Province of China: hyperuricemia in children may need redefinition. Front Pediatr 9:560720
Copur S, Demiray A, Kanbay M (2022) Uric acid in metabolic syndrome: does uric acid have a definitive role? Eur J Intern Med
Kushiyama A, Nakatsu Y, Matsunaga Y et al (2016) Role of uric acid metabolism-related inflammation in the pathogenesis of metabolic syndrome components such as atherosclerosis and nonalcoholic steatohepatitis. Mediators Inflamm 2016:8603164
Spiga R, Marini MA, Mancuso E et al (2017) Uric acid is associated with inflammatory biomarkers and induces inflammation via activating the NF-kappaB signaling pathway in HepG2 Cells. Arterioscler Thromb Vasc Biol 37(6):1241–1249
Ghaemi-Oskouie F, Shi Y (2011) The role of uric acid as an endogenous danger signal in immunity and inflammation. Curr Rheumatol Rep 13(2):160–166
Sarkar S, Alam MM, Das G, Datta S (2017) Inflammatory markers and disease activity in juvenile idiopathic arthritis. Indian J Pediatr 84(5):349–356
Swart JF, de Roock S, Prakken BJ (2016) Understanding inflammation in juvenile idiopathic arthritis: how immune biomarkers guide clinical strategies in the systemic onset subtype. Eur J Immunol 46(9):2068–2077
Acknowledgements
The authors are grateful to all patients and their families.
Author information
Authors and Affiliations
Contributions
MFG and ADS drafted the paper. EMDG, ANO, and ADS participated in the conception and the design of the study. SZ, RM, and SG examined the patients and collected anthropometric and biochemical data. ADS and PM performed the data analysis. ADS, EMDG, ANO, and PM supervised the design and execution of the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Research Ethical Committee of the University of Campania “Luigi Vanvitelli” (protocol code 834/2016).
Consent to participate
Informed consent was obtained from all individual participants included in the study. Patients’ data were treated to guarantee confidentiality.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gicchino, M.F., Marzuillo, P., Zarrilli, S. et al. Uric acid could be a marker of cardiometabolic risk and disease severity in children with juvenile idiopathic arthritis. Eur J Pediatr 182, 149–154 (2023). https://doi.org/10.1007/s00431-022-04657-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04657-8