Abstract
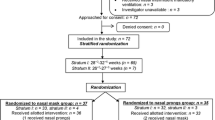
To determine if RAM cannula is non-inferior to short binasal prongs (SBP) in providing nasal continuous positive airway pressure (CPAP) in preterm infants with respiratory distress syndrome (RDS). In this randomized, open-label, noninferiority trial from a low-middle-income country, we enrolled 254 preterm infants (28–34 weeks gestational age) with RDS who needed CPAP as primary respiratory support. The eligible infants were randomized to either RAM cannula or SBP interface groups. The primary outcome was CPAP failure (defined as the need for intubation or non-invasive positive pressure ventilation) within 72 h of randomization. The noninferiority margin was defined as a 10% or less absolute difference in CPAP failure rates. The secondary outcomes included nasal trauma and adverse events. We analyzed by per-protocol (primary) and intention to treat. CPAP failure has been seen in 25 infants (19.7%) in the RAM cannula group versus 22 (17.3%) in the SBP group (RD −2.36%; 95% CI −11.9 to 7.2 [beyond inferiority margin]; p = 0.6). Moderate and severe nasal trauma was less in RAM cannula (2.4 vs. 8.7%; RR 0.27; 95% CI 0.08–0.95; p 0.028). Duration of CPAP was also significantly shorter in the RAM cannula group (MD −12.4 h; 95% CI −20.34 to −4.46, p 0.017). There were no differences in other adverse events.
Conclusions: RAM cannula was not non-inferior to SBP in providing CPAP to preterm infants with respiratory distress syndrome.
Trial registration: Registered at Clinical Trial Registry of India (CTRI/2020/03/024097).
What is Known: • RAM cannula is used for providing supplemental oxygen therapy. There is conflicting evidence on its efficacy in delivering CPAP support in preterm infants. | |
What is New: • RAM cannula was not non-inferior to SBP in providing CPAP to preterm infants with respiratory distress syndrome. • RAM cannula causes less nasal trauma than short binasal prongs. |

Similar content being viewed by others
Availability of data and material
The data is available with the corresponding author. Deidentified data can be provided on reasonable request.
Code availability
Custom coded data available on request.
Abbreviations
- CI:
-
Confidence interval
- CO2:
-
Carbon dioxide
- CPAP:
-
Continuous positive airway pressure
- FiO2:
-
Fraction of inspired oxygen
- InSurE:
-
Intubate surfactant extubate
- NICU:
-
Neonatal intensive care unit
- NIPPV:
-
Non-invasive positive pressure ventilation
- PEEP:
-
Peak end expiratory pressure
- PPV:
-
Positive pressure ventilation
- RCT:
-
Randomized controlled trial
- RD:
-
Risk difference
- RDS:
-
Respiratory distress syndrome
- RR:
-
Risk ratio
- SBP:
-
Short binasal prongs
- SD:
-
Standard deviation
References
Ho JJ, Subramaniam P, Davis PG (2020) Continuous positive airway pressure (CPAP) for respiratory distress in preterm infants. Cochrane Database Syst Rev 10:CD002271. https://doi.org/10.1002/14651858.CD002271.pub3
King BC, Gandhi BB, Jackson A et al (2019) Mask versus prongs for nasal continuous positive airway pressure in preterm infants: a systematic review and meta-analysis. Neonatology 116:100–114. https://doi.org/10.1159/000496462
Say B, Kanmaz Kutman HG, Oguz SS et al (2016) Binasal prong versus nasal mask for applying CPAP to preterm infants: a randomized controlled trial. Neonatology 109:258–264. https://doi.org/10.1159/000443263
Razak A, Patel W (2020) Nasal mask vs binasal prongs for nasal continuous positive airway pressure in preterm infants: a systematic review and meta-analysis. Pediatr Pulmonol 55:2261–2271. https://doi.org/10.1002/ppul.24878
Nzegwu NI, Mack T, DellaVentura R et al (2015) Systematic use of the RAM nasal cannula in the Yale-New Haven Children’s Hospital Neonatal Intensive Care Unit: a quality improvement project. J Matern-Fetal Neonatal Med 28:718–721. https://doi.org/10.3109/14767058.2014.929659
Maram S, Murki S, Nayyar S et al (2021) RAM cannula with Cannulaide versus Hudson prongs for delivery of nasal continuous positive airway pressure in preterm infants: an RCT. Sci Rep 11:23527. https://doi.org/10.1038/s41598-021-02988-4
Gokce IK, Kaya H, Ozdemir R (2021) A randomized trial comparing the short binasal prong to the RAM cannula for noninvasive ventilation support of preterm infants with respiratory distress syndrome. J Matern-Fetal Neonatal Med 34:1868–1874. https://doi.org/10.1080/14767058.2019.1651268
Gerdes JS, Sivieri EM, Abbasi S (2016) Factors influencing delivered mean airway pressure during nasal CPAP with the RAM cannula. Pediatr Pulmonol 51:60–69. https://doi.org/10.1002/ppul.23197
Iyer NP, Chatburn R (2015) Evaluation of a nasal cannula in noninvasive ventilation using a lung simulator. Respir Care 60:508–512. https://doi.org/10.4187/respcare.03560
Singh N, McNally MJ, Darnall RA (2019) Does the RAM cannula provide continuous positive airway pressure as effectively as the Hudson prongs in preterm neonates? Am J Perinatol 36:849–854. https://doi.org/10.1055/s-0038-1675330
Drescher GS, Hughes CW (2018) Comparison of interfaces for the delivery of noninvasive respiratory support to low birthweight infants. Respir Care 63:1197–1206. https://doi.org/10.4187/respcare.05978
Mukerji A, Belik J (2015) Neonatal nasal intermittent positive pressure ventilation efficacy and lung pressure transmission. J Perinatol 35:716–719. https://doi.org/10.1038/jp.2015.61
Thaddanee R, Chaudhari A, Chauhan H et al (2018) Bubble continuous positive airway pressure machine versus indigenous bubble continuous positive airway pressure as a respiratory support in preterm babies with respiratory distress syndrome: a prospective outcome research at a tertiary care centre in Gujarat, India. Int J Contemp Pediatr 5:493. https://doi.org/10.18203/2349-3291.ijcp20180542
Deorari AK, Kumar P, Murki S Workbook on CPAP Science, Evidence, and Practice, 4th ed. Available from: https://www.newbornwhocc.org/pdf/Evidence%20&%20Intial%20pages.pdf
Downes JJ, Vidyasagar D, Boggs TR, Morrow GM (1970) Respiratory distress syndrome of newborn infants. I. New clinical scoring system (RDS score) with acid–base and blood-gas correlations. Clin Pediatr (Phila) 9:325–331. https://doi.org/10.1177/000992287000900607
Sweet DG, Carnielli V, Greisen G et al (2019) European consensus guidelines on the management of respiratory distress syndrome - 2019 update. Neonatology 115:432–450. https://doi.org/10.1159/000499361
De Luca D, Autilio C, Pezza L et al (2021) Personalized medicine for the management of RDS in preterm neonates. Neonatology 118:127–138. https://doi.org/10.1159/000513783
Raschetti R, Yousef N, Vigo G et al (2019) Echography-guided surfactant therapy to improve timeliness of surfactant replacement: a quality improvement project. J Pediatr 212:137-143.e1. https://doi.org/10.1016/j.jpeds.2019.04.020
Black J, Baharestani MM, Cuddigan J et al (2007) National Pressure Ulcer Advisory Panel’s updated pressure ulcer staging system. Adv Skin Wound Care 20:269–274. https://doi.org/10.1097/01.ASW.0000269314.23015.e9
Fischer C, Bertelle V, Hohlfeld J et al (2010) Nasal trauma due to continuous positive airway pressure in neonates. Arch Dis Child Fetal Neonatal Ed 95:F447-451. https://doi.org/10.1136/adc.2009.179416
Wright CJ, Sherlock LG, Sahni R, Polin RA (2018) Preventing continuous positive airway pressure failure: evidence-based and physiologically sound practices from delivery room to the neonatal intensive care unit. Clin Perinatol 45:257–271. https://doi.org/10.1016/j.clp.2018.01.011
Thukral A, Sankar MJ, Chandrasekaran A et al (2016) Efficacy and safety of CPAP in low- and middle-income countries. J Perinatol 36(Suppl 1):S21-28. https://doi.org/10.1038/jp.2016.29
Hochwald O, Riskin A, Borenstein-Levin L et al (2021) Cannula with long and narrow tubing vs short binasal prongs for noninvasive ventilation in preterm infants: noninferiority randomized clinical trial. JAMA Pediatr 175:36–43. https://doi.org/10.1001/jamapediatrics.2020.3579
Claassen CC, Hillman NH, Brown K et al (2019) Comparison of bubble CPAP devices using RAM cannula for extubation failure in very low birth weight infants: randomized and cohort studies. Neonatology 115:28–35. https://doi.org/10.1159/000493156
Pillow JJ, Hillman N, Moss TJM et al (2007) Bubble continuous positive airway pressure enhances lung volume and gas exchange in preterm lambs. Am J Respir Crit Care Med 176:63–69. https://doi.org/10.1164/rccm.200609-1368OC
Sharma D, Murki S, Maram S et al (2020) Comparison of delivered distending pressures in the oropharynx in preterm infant on bubble CPAP and on three different nasal interfaces. Pediatr Pulmonol 55:1631–1639. https://doi.org/10.1002/ppul.24752
Althunian TA, de Boer A, Klungel OH et al (2017) Methods of defining the non-inferiority margin in randomized, double-blind controlled trials: a systematic review. Trials 18:107. https://doi.org/10.1186/s13063-017-1859-x
Piaggio G, Elbourne DR, Pocock SJ et al (2012) Reporting of noninferiority and equivalence randomized trials: extension of the CONSORT 2010 statement. JAMA 308:2594–2604. https://doi.org/10.1001/jama.2012.87802
Althunian TA, de Boer A, Groenwold RHH, Klungel OH (2017) Defining the noninferiority margin and analysing noninferiority: an overview. Br J Clin Pharmacol 83:1636–1642. https://doi.org/10.1111/bcp.13280
Author information
Authors and Affiliations
Contributions
SKS: conceived idea, recruited participants, and critically reviewed the manuscript. PD and AY: conceived idea, supervised patient recruitment and data collection, participated in manuscript writing and revisions. JK: data analysis, participated in manuscript writing and revisions. PA and MG: data collection, critically reviewed and revised the manuscript. All the authors approved the final version of the manuscript and shall be accountable for all aspects of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. The Institutional Ethics Committee of Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, approved the study protocol.
Consent to participate
All participants were recruited after taking written informed consent.
Consent for publication
All authors consented to publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Samim, S.K., Debata, P.K., Yadav, A. et al. RAM cannula versus short binasal prongs for nasal continuous positive airway pressure delivery in preterm infants: a randomized, noninferiority trial from low-middle-income country. Eur J Pediatr 181, 4111–4119 (2022). https://doi.org/10.1007/s00431-022-04620-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04620-7