Abstract
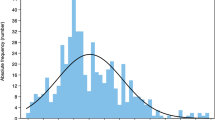
The associations of early-life head circumference (HC) with child neurodevelopmental and mental health among generally healthy population remain unclear. We aimed to examine the associations of early-life HC trajectories with cognitive development and emotional and behavioral problems in adolescence and to identify the HC growth–sensitive period. We conducted a prospective, community-based birth cohort study in rural western China, and 745 adolescents aged 10–14 years were followed between June and December 2016. We assessed their HC eight times during the first 2 years of life and their adolescent cognitive, emotional, and behavioral outcomes using the Wechsler Intelligence Scale for Children-IV and Youth Self-Report-2001, respectively. We applied group-based trajectory modeling to identify the HC trajectories and conditional growth to derive the HC growth–sensitive periods. We identified five distinct HC trajectories characterized as Start below average-then decrease (7.8% of the sample), Start below average-then increase (6.8%), Start average-then decrease (33%), Consistently average (38%), and Consistently above average (14%). Infants in the trajectory of consistently above average had higher cognitive scores in adolescence compared to those from suboptimal trajectories, with adjusted mean differences ranging from 2.84 to 8.99 points. The conditional gains showed that the HC growth–sensitive period was between 0 and 18 months for child cognition. We found null associations between HC measures and adolescent emotional and behavioral problem scores.
Conclusion: Early-life HC trajectories were associated with adolescent cognitive development. HC may serve as an inexpensive screening tool to monitor child development at risk during the first 18 months, particularly in resource-limited settings.
What is Known: • Postnatal head circumference (HC) has been shown to be associated with cognitive development in infants who were born premature and/or fetal growth restriction, while inconsistent associations were reported among generally healthy populations, especially in low- and middle- income countries, challenging its utility in public health practices. | |
What is New: • Adolescents in the HC growth trajectory of consistently above average had higher cognitive scores compared to those with other suboptimal trajectories, while null findings were observed for adolescent emotional and behavioral health. • HC may serve as an inexpensive screening tool to monitor child development at risk during the first 18 months of life, particularly in resource-limited settings. |



Similar content being viewed by others
Availability of data and materials
Individual data are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Abbreviations
- CI:
-
Confidence interval
- FSIQ:
-
Full-Scale Intelligence Quotient
- LMICs:
-
Low- and middle-income counties
- MUAC:
-
Mid upper arm circumference
- SD:
-
Standard deviation
- SGA:
-
Small for gestational age
- WHO:
-
World Health Organization
- WISC-IV:
-
Wechsler Intelligence Scale for children-Fourth Edition
- YSR:
-
Youth Self-Report
References
Black MM, Walker SP, Fernald LC et al (2017) Early childhood development coming of age: science through the life course. Lancet 389:77–90
Jaekel J, Sorg C, Baeuml J, Bartmann P, Wolke D (2019) Head growth and intelligence from birth to adulthood in very preterm and term born individuals. J Int Neuropsych Soc 25:48–56
Lidzba K, Rodemann S, Goelz R, Krägeloh-Mann I, Bevot A (2016) Growth in very preterm children: head growth after discharge is the best independent predictor for cognitive outcome. Early Hum Dev 103:183–188
Ong KK, Kennedy K, Castaneda-Gutierrez E et al (2015) Postnatal growth in preterm infants and later health outcomes: a systematic review. Acta Paediatr 104:974–986
Koshy B, Srinivasan M, Murugan TP et al (2021) Association between head circumference at two years and second and fifth year cognition. BMC Pediatr 21:74
Gale CR, O’Callaghan FJ, Godfrey KM, Law CM, Martyn CN (2004) Critical periods of brain growth and cognitive function in children. Brain 127:321–329
Nicolaou L, Ahmed T, Bhutta ZA et al (2020) Factors associated with head circumference and indices of cognitive development in early childhood. BMJ Glob Health e3427
Sinclair D, Dangerfield P (1998) Human growth after birth, 6th edn. Oxford University Press, Oxford
Kirkegaard H, Möller S, Wu C et al (2020) Associations of birth size, infancy, and childhood growth with intelligence quotient at 5 years of age: a Danish cohort study. Am J Clin Nutr 112:96–105
Flensborg-Madsen T, Falgreen Eriksen H, Mortensen EL (2015) Early life predictors of intelligence in young adulthood and middle age. PloS One e228144
Ferrer M, García-Esteban R, Iñiguez C et al (2019) Head circumference and child ADHD symptoms and cognitive functioning: results from a large population-based cohort study. Eur Child Adoles Psy 28:377–388
Dupont C, Castellanos-Ryan N, Séguin JR et al (2018) The predictive value of head circumference growth during the first year of life on early child traits. Sci Rep 8:9828
Gale CR, O’Callaghan FJ, Bredow M, Martyn CN (2006) The influence of head growth in fetal life, infancy, and childhood on intelligence at the ages of 4 and 8 years. Pediatrics 118:1486–1492
Scharf RJ, Rogawski ET, Murray Kolb LE et al (2018) Early childhood growth and cognitive outcomes: findings from the MAL-ED study. Matern Child Nutr 14:e12584
Smithers LG, Lynch JW, Yang S, Dahhou M, Kramer MS (2013) Impact of neonatal growth on IQ and behavior at early school age. Pediatrics 132:e53–e60
Sammallahti S, Heinonen K, Andersson S et al (2017) Growth after late-preterm birth and adult cognitive, academic, and mental health outcomes. Pediatr Res 81:767–774
Zeng L, Dibley MJ, Cheng Y et al (2008) Impact of micronutrient supplementation during pregnancy on birth weight, duration of gestation, and perinatal mortality in rural western China: double blind cluster randomised controlled trial. BMJ 337:a2001
Villar J, Cheikh IL, Victora CG et al (2014) International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 384:857–868
de Onis M, Garza C, Onyango AW, Martorell R (2006) WHO child growth standards. Acta Paediatrica Suppl 450:1–101
Wechsler D (2004) The Wechsler intelligence scale for children-fourth edition. Pearson, London
Leung PWL, Kwong SL, Tang CP et al (2006) Test-retest reliability and criterion validity of the Chinese version of CBCL, TRF, and YSR. J Child Psychol Psyc 47:970–973
Zhang X, Tilling K, Martin RM et al (2019) Analysis of ‘sensitive’ periods of fetal and child growth. Int J Epidemiol 48:116–123
Nagin DS, Jones BL, Passos VL, Tremblay RE (2016) Group-based multi-trajectory modeling. Stat Methods Med Res 27:2015–2023
Ni Y, Beckmann J, Gandhi R, Hurst JR, Morris JK, Marlow N (2020) Growth to early adulthood following extremely preterm birth: the EPICure study. Arch Dis Child Fetal Neonatal Ed 105:496–503
Leroy JL, Frongillo EA, Dewan P, Black MM, Waterland RA (2020) Can children catch up from the consequences of undernourishment?. Evidence from child linear growth, developmental epigenetics, and brain and neurocognitive development. Adv Nutr 11:1032–1041
Sindhu KN, Ramamurthy P, Ramanujam K et al (2019) Low head circumference during early childhood and its predictors in a semi-urban settlement of Vellore. Southern India BMC Pediatr 19:182
Bouthoorn SH, van Lenthe FJ, Hokken-Koelega AC et al (2012) Head circumference of infants born to mothers with different educational levels. The Generation R Study PloS One 7:e39798
Matijasevich A, Howe LD, Tilling K, Santos IS, Barros AJ, Lawlor DA (2012) Maternal education inequalities in height growth rates in early childhood: 2004 Pelotas birth cohort study. Paediatr Perinat Epidemiol 26:236–249
Broere-Brown ZA, Baan E, Schalekamp-Timmermans S, Verburg BO, Jaddoe VW, Steegers EAV (2016) Sex-specific differences in fetal and infant growth patterns: a prospective population-based cohort study. Biol Sex Differ 7:65
Melamed N, Meizner I, Mashiach R, Wiznitzer A, Glezerman M, Yogev Y (2013) Fetal sex and intrauterine growth patterns. J Ultrasound Med 32:35–43
Vaidya A, Saville N, Shrestha BP, Costello AM, Manandhar DS, Osrin D (2008) Effects of antenatal multiple micronutrient supplementation on children’s weight and size at 2 years of age in Nepal: follow-up of a double-blind randomised controlled trial. Lancet 371:492–499
Christian P, Khatry SK, Katz J, Pradhan EK et al (2003) Effects of alternative maternal micronutrient supplements on low birth weight in rural Nepal: double blind randomised community trial. BMJ 326:571
Keats EC, Haider BA, Tam E, Bhutta ZA (2019) Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database Syst Rev 3:D4905
Bach CC, Henriksen TB, Larsen RT, Aagaard K, Matthiesen NB (2020) Head circumference at birth and school performance: a nationwide cohort study of 536,921 children. Pediatr Res 87:1112–1118
Norris T, Johnson W, Petherick E et al (2018) Investigating the relationship between fetal growth and academic attainment: secondary analysis of the Born in Bradford (BiB) cohort. Int J Epidemiol 47:1475–1484
Catena A, Martínez-Zaldívar C, Diaz-Piedra C et al (2019) On the relationship between head circumference, brain size, prenatal long-chain PUFA/5-methyltetrahydrofolate supplementation and cognitive abilities during childhood. Brit J Nutr 122:S40–S48
Jin C, Li Y, Li X et al (2019) Associations of gestational age and birth anthropometric indicators with brain white matter maturation in full-term neonates. Hum Brain Mapp 40:3620–3630
Lee JJ, McGue M, Iacono WG, Michael AM, Chabris CF (2019) The causal influence of brain size on human intelligence: evidence from within-family phenotypic associations and GWAS modeling. Intelligence 75:48–58
Sania A, Sudfeld CR, Danaei G et al (2019) Early life risk factors of motor, cognitive and language development: a pooled analysis of studies from low/middle-income countries. BMJ Open 9:e26449
Knickmeyer RC, Gouttard S, Kang C, Evans D, Wilber K, Smith JK, Hamer RM, Lin W, Gerig G, Gilmore JH (2008) A structural MRI study of human brain development from birth to 2 years. J Neurosci 28:12176–12182
Gilmore JH, Shi F, Woolson SL, Knickmeyer RC, Short SJ, Lin W, Zhu H, Hamer RM, Styner M, Shen D (2012) Longitudinal development of cortical and subcortical gray matter from birth to 2 years. Cereb Cortex 22:2478–2485
Haartsen R, Jones EJH, Johnson MH (2016) Human brain development over the early years. Curr Opin Behav Sci 10:149–154
Gilmore JH, Knickmeyer RC, Gao W (2018) Imaging structural and functional brain development in early childhood. Nat Rev Neurosci 19:123–137
Bartholomeusz HH, Courchesne E, Karns CM (2002) Relationship between head circumference and brain volume in healthy normal toddlers, children, and adults. Neuropediatrics 33:239–241
Boat TF, Kelleher KJ (2020) Fostering healthy mental, emotional, and behavioral development in child health care. JAMA Pediatr 174:745–746
Dotinga BM, de Winter AF, Bocca-Tjeertes I, Kerstjens JM, Reijneveld SA, Bos AF (2019) Longitudinal growth and emotional and behavioral problems at age 7 in moderate and late preterms. PLoS ONE 14:e211427
Huang C, Martorell R, Ren A, Li Z (2013) Cognition and behavioural development in early childhood: the role of birth weight and postnatal growth. Int J Epidemiol 42:160–171
Johnson S, Kochhar P, Hennessy E, Marlow N, Wolke D, Hollis C (2016) Antecedents of attention-deficit/hyperactivity disorder symptoms in children born extremely preterm. J Dev Behav Pediatr 37:285–297
Murray E, Pearson R, Fernandes M et al (2016) Are fetal growth impairment and preterm birth causally related to child attention problems and ADHD?. Evidence from a comparison between high-income and middle-income cohorts. J Epidemiol Community Health 70:704–709
Murray E, Matijasevich A, Santos IS et al (2015) Sex differences in the association between foetal growth and child attention at age four: specific vulnerability of girls. J Child Psychol Psychiatry 56:1380–1388
Victora CG, Horta BL, Loret DMC, Quevedo L, Pinheiro RT, Gigante DP, Goncalves H, Barros FC (2015) Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: a prospective birth cohort study from Brazil. Lancet Glob Health 3:e199-205
Funding
This work was supported by the National Natural Science Foundation of China (grants 81872633 to LZ, 82103867 to ZZ, and 81803264 to CL) and the China Postdoctoral Science Foundation (grant 2021M702578 to ZZ).
Author information
Authors and Affiliations
Contributions
ZZ, YC, MJD, and LZ designed the study; ZZ, JS, YZ, LW, XW, LC, QQ, AKA, and ME conducted the study; ZZ and JS analyzed data and interpreted results; ZZ wrote the paper; LZ had primary responsibility for final content; and all authors reviewed, revised, and approved the final paper. ZZ and JS contributed equally to this paper.
Corresponding author
Ethics declarations
Ethics approval
The trial and follow-up evaluation protocols were approved by the Ethics Committee in Xi’an Jiaotong University Health Science Center.
Consent to participate
Written informed consent was obtained from the biological parents or caregivers, while verbal consent was obtained from all the participants depending on their age.
Consent to publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Gregorio Paolo Milani
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Reprint request author: Lingxia Zeng
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhu, Z., Shen, J., Zhu, Y. et al. Head circumference trajectories during the first two years of life and cognitive development, emotional, and behavior problems in adolescence: a cohort study. Eur J Pediatr 181, 3401–3411 (2022). https://doi.org/10.1007/s00431-022-04554-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04554-0