Abstract
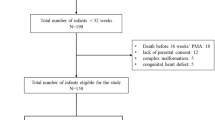
The N-terminal end of B-type natriuretic peptide (NT-proBNP) and lung ultrasound (LUS) score have been proven to be adequate early biomarkers of bronchopulmonary dysplasia (BPD) in preterm infants. Our aim was to study if the predictive capacity of each one is increased by analyzing them together. We included infants born before 32 weeks with NT-proBNP and LUS scores on the first day of life (DOL) and on the 3rd, 7th, and 14th DOL and compared the diagnostic ability for moderate–severe BPD (msBPD) of each biomarker and in combination. We also compared them with a multivariate model of msBPD using only clinical variables. The sample size was 133 patients, and twenty-seven (20%) developed msBPD. The LUS score on the 7th DOL had better performance than NT-proBNP at the same moment: area under the receiver operating characteristic curve (AUC) 0.83 (0.75–0.89) versus 0.66 (0.56–0.75), p = 0.003, without differences in the rest of the times studied. These values did not increase when using the combination of both. A multivariate regression model that included only clinical variables (birth weight and invasive mechanical ventilation (IMV) at the 7th DOL) predicted msBPD with the same AUC as after the addition of any of these biomarkers, neither together.
Conclusion: The LUS score is a better predictor of msBPD on the 7th DOL than NT-proBNP in preterm infants born before 32 weeks, although they have similar diagnostic accuracy on the 1st, 3rd, and 14th DOL. Neither of them, nor together, have a better AUC for msBPD than a clinical model with birthweight and the need for IMV at the 7th DOL.
What is Known: • NT-proBNP and LUS score are early predictors of moderate–severe bronchopulmonary dysplasia (msBPD). | |
What is New: • The combination of both NT-proBNP and LUS score does not increase the predictive ability of each separately. |


Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
Abbreviations
- AIC:
-
Akaike information criteria
- AUC:
-
Area under the receiver operating characteristic curve
- BIC:
-
Bayesian information criteria
- BNP:
-
B-Type natriuretic peptide
- BPD:
-
Bronchopulmonary dysplasia
- CRIB-II:
-
Clinical risk index for babies-II
- DOL:
-
Day of life
- EDTA:
-
Ethylenediaminetetraacetic acid
- ECLIA:
-
Electroluminescence immunoassay kit
- GA:
-
Gestational age
- hsPDA:
-
Haemodynamically significant patent ductus arteriosus
- ICC:
-
Intraclass correlation coefficient
- IMV:
-
Invasive mechanical ventilation
- LUS:
-
Lung ultrasound
- msBPD:
-
Moderate–severe bronchopulmonary dysplasia
- NIV:
-
Noninvasive ventilation
- NT-proBNP:
-
N-Terminal end of B-type natriuretic peptide
- PDA:
-
Patent ductus arteriosus
- PMA:
-
Postmenstrual age
- PT:
-
Preterm infants
- RDS:
-
Respiratory distress syndrome
- SNAPPE-II:
-
Score for neonatal acute physiology
- VLBWI:
-
Very-low-birth-weight infants
References
Coalson JJ (2003) Pathology of new bronchopulmonary dysplasia. Seminars in Neonatology 8:73–81. https://doi.org/10.1016/S1084-2756(02)00193-8
Zafra-Rodríguez P, Méndez-Abad P, Lubián-López SP, Benavente-Fernández I (2019) NT-proBNP as an early marker of diastolic ventricular dysfunction in very-low-birth-weight infants. Pediatr Cardiol 40:1165–1170. https://doi.org/10.1007/s00246-019-02125-z
Joseph L, Nir A, Hammerman C et al (2010) N-terminal pro-B-type natriuretic peptide as a marker of bronchopulmonary dysplasia in premature infants. Amer J Perinatol 27:381–386. https://doi.org/10.1055/s-0029-1243312
Dasgupta S, Aly AM, Malloy MH et al (2018) NTproBNP as a surrogate biomarker for early screening of pulmonary hypertension in preterm infants with bronchopulmonary dysplasia. J Perinatol 38:1252–1257. https://doi.org/10.1038/s41372-018-0164-1
Montaner A, Pinillos R, Galve Z et al (2017) Brain natriuretic propeptide as an early marker of bronchopulmonary dysplasia or death in the preterm newborn. Klin Padiatr 229:223–228. https://doi.org/10.1055/s-0043-111597
Mir TS, Laux R, Hellwege HH et al (2003) Plasma concentrations of aminoterminal pro atrial natriuretic peptide and aminoterminal pro brain natriuretic peptide in healthy neonates: marked and rapid increase After Birth. Pediatrics 112:896–899. https://doi.org/10.1542/peds.112.4.896
Méndez-Abad P, Zafra-Rodríguez P, Lubián-López S, Benavente-Fernández I (2019) NTproBNP is a useful early biomarker of bronchopulmonary dysplasia in very low birth weight infants. Eur J Pediatr 178:755–761. https://doi.org/10.1007/s00431-019-03347-2
Rodríguez-Blanco S, Oulego-Erroz I, Alonso-Quintela P et al (2018) N-terminal-probrain natriuretic peptide as a biomarker of moderate to severe bronchopulmonary dysplasia in preterm infants: a prospective observational study. Pediatr Pulmonol 53:1073–1081. https://doi.org/10.1002/ppul.24053
Harris SL, More K, Dixon B et al (2018) Factors affecting N-terminal pro-B-type natriuretic peptide levels in preterm infants and use in determination of haemodynamic significance of patent ductus arteriosus. Eur J Pediatr 177:521–532. https://doi.org/10.1007/s00431-018-3089-y
Sellmer A, Hjortdal VE, Bjerre JV et al (2015) N-Terminal pro-B type natriuretic peptide as a marker of bronchopulmonary dysplasia or death in very preterm neonates: a cohort study. PLoS ONE 10:e0140079. https://doi.org/10.1371/journal.pone.0140079
Raimondi F, Yousef N, Migliaro F et al (2018) Point-of-care lung ultrasound in neonatology: classification into descriptive and functional applications. Pediatr Res 1–8. https://doi.org/10.1038/s41390-018-0114-9
Corsini I, Parri N, Gozzini E et al (2019) Lung ultrasound for the differential diagnosis of respiratory distress in neonates. Neonatology 115:77–84. https://doi.org/10.1159/000493001
Brat R, Yousef N, Klifa R et al (2015) Lung ultrasonography score to evaluate oxygenation and surfactant need in neonates treated with continuous positive airway pressure. JAMA Pediatr 169:e151797. https://doi.org/10.1001/jamapediatrics.2015.1797
Aldecoa-Bilbao V, Velilla M, Teresa-Palacio M et al (2021) Lung ultrasound in bronchopulmonary dysplasia: patterns and predictors in very preterm infants. Neonatology 1–9. https://doi.org/10.1159/000517585
Mohamed A, Mohsen N, Diambomba Y et al (2021) Lung ultrasound for prediction of bronchopulmonary dysplasia in extreme preterm neonates: a prospective diagnostic cohort study. J Pediatr S0022347621006612. https://doi.org/10.1016/j.jpeds.2021.06.079
Raimondi F, Migliaro F, Corsini I et al (2021) Lung ultrasound score progress in neonatal respiratory distress syndrome. Pediatrics 147:e2020030528. https://doi.org/10.1542/peds.2020-030528
Alonso-Ojembarrena A, Serna-Guerediaga I, Aldecoa-Bilbao V et al (2021) The predictive value of lung ultrasound scores in developing bronchopulmonary dysplasia. Chest S0012369221004682. https://doi.org/10.1016/j.chest.2021.02.066
Loi B, Vigo G, Baraldi E et al (2020) Lung ultrasound to monitor extremely preterm infants and predict BPD: multicenter longitudinal cohort study. Am J Respir Crit Care Med rccm.202008–3131OC. https://doi.org/10.1164/rccm.202008-3131OC
Oulego-Erroz I, Alonso-Quintela P, Terroba-Seara S et al (2020) Early assessment of lung aeration using an ultrasound score as a biomarker of developing bronchopulmonary dysplasia: a prospective observational study. J Perinatol. https://doi.org/10.1038/s41372-020-0724-z
Pezza L, Alonso-Ojembarrena A, Elsayed Y et al (2022) Meta-analysis of lung ultrasound scores for early prediction of bronchopulmonary dysplasia. Annals ATS 19:659–667. https://doi.org/10.1513/AnnalsATS.202107-822OC
Alonso-Ojembarrena A, Lubián-López SP (2019) Lung ultrasound score as early predictor of bronchopulmonary dysplasia in very low birth weight infants. Pediatr Pulmonol 54:1404–1409. https://doi.org/10.1002/ppul.24410
Walsh MC, Yao Q, Gettner P et al (2004) Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics 114:1305–1311. https://doi.org/10.1542/peds.2004-0204
Louis D, Belen K, Farooqui M et al (2019) Prone versus supine position for lung ultrasound in neonates with respiratory distress. Amer J Perinatol s-0039–1695776. https://doi.org/10.1055/s-0039-1695776
Parry G, Tucker J, Tarnow-Mordi W, UK Neonatal Staffing Study Collaborative Group (2003) CRIB II: an update of the clinical risk index for babies score. Lancet 361:1789–1791. https://doi.org/10.1016/S0140-6736(03)13397-1
Richardson DK, Corcoran JD, Escobar GJ, Lee SK (2001) SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores. J Pediatr 138:92–100
Gibbs RS, Blanco JE, St. Clair PJ, Castaneda YS, (1982) Quantitative bacteriology of amniotic fluid from women with clinical intraamniotic infection at term. J Infect Dis 145:1–8. https://doi.org/10.1093/infdis/145.1.1
Pacora P, Chaiworapongsa T, Maymon E et al (2002) Funisitis and chorionic vasculitis: the histological counterpart of the fetal inflammatory response syndrome. J Matern Fetal Neonatal Med 11:18–25. https://doi.org/10.1080/jmf.11.1.18.25
Arlettaz R (2017) Echocardiographic evaluation of patent ductus arteriosus in preterm infants. Front Pediatr 5:147. https://doi.org/10.3389/fped.2017.00147
Akaike H (1973) Information theory and an extension of the maximum likelihood principle. International Symposium on Information Theory, 2nd edn. Akademiai Kiado, Budapest, pp 267–281
Schwarz GE (1978) Estimating the dimension of a model. Annals of Statistics 461–464
Vandenbroucke JP (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med 147:W163–W194. https://doi.org/10.7326/0003-4819-147-8-200710160-00010-w1
Mendez-Abad P, Zafra-Rodriguez P, Lubián-López SP, Benavente-Fernández I (2019) NTproBNP is a useful early biomarker of bronchopulmonary dysplasia in very low birth weight infants. Eur J Pediatr 178:755–761. https://doi.org/10.1007/s00431-019-03347-2
Zhou L, Xiang X, Wang L et al (2019) N-Terminal Pro-B-type natriuretic peptide as a biomarker of bronchopulmonary dysplasia or death in preterm infants: a retrospective cohort analysis. Front Pediatr 7:166. https://doi.org/10.3389/fped.2019.00166
Yousef N, Vigo G, Shankar-Aguilera S, De Luca D (2020) Semiquantitative ultrasound assessment of lung aeration correlates with lung tissue inflammation. Ultrasound Med Biol 46:1258–1262. https://doi.org/10.1016/j.ultrasmedbio.2020.01.018
Raimondi F, Migliaro F, Corsini I et al (2021) Neonatal lung ultrasound and surfactant administration: a pragmatic, multicenter study. Chest S0012369221013544. https://doi.org/10.1016/j.chest.2021.06.076
Song M, Lei M, Luo C et al (2021) Development of a nomogram for moderate-to-severe bronchopulmonary dysplasia or death: role of N-terminal pro-brain natriuretic peptide as a biomarker. Front Pediatr 9:727362. https://doi.org/10.3389/fped.2021.727362
Montgomery AM, Bazzy-Asaad A, Asnes JD et al (2016) Biochemical screening for pulmonary hypertension in preterm infants with bronchopulmonary dysplasia. Neonatology 109:190–194. https://doi.org/10.1159/000442043
Avitabile CM, Ansems S, Wang Y et al (2019) Accuracy of brain natriuretic peptide for diagnosing pulmonary hypertension in severe bronchopulmonary dysplasia. Neonatology 116:147–153. https://doi.org/10.1159/000499082
Kim HH, Sung SI, Yang MS et al (2021) Early pulmonary hypertension is a risk factor for bronchopulmonary dysplasia-associated late pulmonary hypertension in extremely preterm infants. Sci Rep 11:11206. https://doi.org/10.1038/s41598-021-90769-4
Xie H, Huo Y, Chen Q, Hou X (2021) Application of B-type natriuretic peptide in neonatal diseases. Front Pediatr 9:767173. https://doi.org/10.3389/fped.2021.767173
Dassios T, Williams EE, Hickey A, Greenough A (2021) Duration of mechanical ventilation and prediction of bronchopulmonary dysplasia and home oxygen in extremely preterm infants. Acta Paediatr 110:2052–2058. https://doi.org/10.1111/apa.15801
Villamor-Martinez E, Álvarez-Fuente M, Ghazi AMT et al (2019) Association of chorioamnionitis with bronchopulmonary dysplasia among preterm infants: a systematic review, meta-analysis, and metaregression. JAMA Netw Open 2:e1914611. https://doi.org/10.1001/jamanetworkopen.2019.14611
Ebrahimi ME, Romijn M, Vliegenthart RJS et al (2021) The association between clinical and biochemical characteristics of late-onset sepsis and bronchopulmonary dysplasia in preterm infants. Eur J Pediatr 180:2147–2154. https://doi.org/10.1007/s00431-021-03981-9
Uberos J, Jimenez-Montilla S, Molina-Oya M, García-Serrano JL (2020) Early energy restriction in premature infants and bronchopulmonary dysplasia: a cohort study. Br J Nutr 123:1024–1031. https://doi.org/10.1017/S0007114520000240
Onland W, Debray TP, Laughon MM et al (2013) Clinical prediction models for bronchopulmonary dysplasia: a systematic review and external validation study. BMC Pediatr 13:207. https://doi.org/10.1186/1471-2431-13-207
Jung YH, Jang J, Kim H-S et al (2019) Respiratory severity score as a predictive factor for severe bronchopulmonary dysplasia or death in extremely preterm infants. BMC Pediatr 19:121. https://doi.org/10.1186/s12887-019-1492-9
Zhang J, Luo C, Lei M et al (2021) Development and validation of a nomogram for predicting bronchopulmonary dysplasia in very-low-birth-weight infants. Front Pediatr 9:648828. https://doi.org/10.3389/fped.2021.648828
Laughon MM, Langer JC, Bose CL et al (2011) Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am J Respir Crit Care Med 183:1715–1722. https://doi.org/10.1164/rccm.201101-0055OC
Doyle LW, Halliday HL, Ehrenkranz RA et al (2014) An update on the impact of postnatal systemic corticosteroids on mortality and cerebral palsy in preterm infants: effect modification by risk of bronchopulmonary dysplasia. J Pediatr 165:1258–1260. https://doi.org/10.1016/j.jpeds.2014.07.049
Singh Y, Tissot C, Fraga MV et al (2020) International evidence-based guidelines on Point of Care Ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit Care 24:65. https://doi.org/10.1186/s13054-020-2787-9
Gomond-Le Goff C, Vivalda L, Foligno S et al (2020) Effect of different probes and expertise on the interpretation reliability of point-of-care lung ultrasound. Chest 157:924–931. https://doi.org/10.1016/j.chest.2019.11.013
Gouwens KR, Higano NS, Marks KT et al (2020) Magnetic resonance imaging evaluation of regional lung V t s in severe neonatal bronchopulmonary dysplasia. Am J Respir Crit Care Med 202:1024–1031. https://doi.org/10.1164/rccm.202001-0213OC
Author information
Authors and Affiliations
Contributions
AAO, PMA, PZR and SLL contributed to the study conception and design. Data collection was performed by AAO, PAQ, and IOE. Statistical analysis was performed by AAO. The first draft of the manuscript was written by AAO, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study protocol was approved by each regional Ethics Committee with the code number LUS-NEO-17–02.
Consent to participate
Parents gave informed consent for participation in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alonso-Ojembarrena, A., Méndez-Abad, P., Alonso-Quintela, P. et al. Lung ultrasound score has better diagnostic ability than NT-proBNP to predict moderate–severe bronchopulmonary dysplasia. Eur J Pediatr 181, 3013–3021 (2022). https://doi.org/10.1007/s00431-022-04491-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04491-y