Abstract
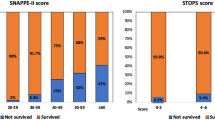
Various studies validated and compared Score for Neonatal Acute Physiology with Perinatal extension-II (SNAPPE-II) and Clinical Risk Index for Babies-II (CRIB-II) admission sickness severity scores for predicting survival, but very few studies compared them for predicting the morbidities in preterm infants. In this multicenter prospective observational study, SNAPPE-II and CRIB-II newborn illness severity scores were compared for predicting mortality and morbidities in infants with gestational age of ≤ 32 weeks. Major morbidities were classified as bronchopulmonary dysplasia, abnormal cranial ultrasound (presence of intraventricular hemorrhage grade III or more or periventricular leukomalacia grade II to IV), and retinopathy of prematurity requiring treatment. Combined adverse outcome was defined as death or any major morbidity. Comparison of the scoring systems was done by area under the curve (AUC) on receiver operating characteristics curve (ROC curve) analysis. A total of 419 neonates who were admitted to 5 participating NICUs were studied. The mortality rate in the study population was 8.8%. Both CRIB-II (AUC: 0.795) and SNAPPE-II (AUC: 0.78) had good predictive ability for in-hospital mortality. For predicting any one of the major morbidities and combined adverse outcome, CRIB-II had better predictive ability than SNAPPE-II with AUC of 0.83 vs. 0.70 and 0.85 vs. 0.74, respectively.
Conclusion: In infants with gestational age of ≤ 32 weeks, both CRIB-II and SNAPPE-II are good scoring systems for predicting mortality. CRIB-II, being a simpler scoring system and having better predictive ability for major morbidities and combined adverse outcome, is preferable over SNAPPE-II.
What is Known: • SNAPPE-II and CRIB-II scores have good predictive ability on in-hospital mortality in preterm neonates. | |
What is New: • SNAPPE-II and CRIB-II both have good predictive ability for mortality, but CRIB-II has better ability for short-term morbidities related to the prematurity. |



Similar content being viewed by others
Availability of data and material
Data will be available with corresponding author.
Code availability
Not applicable.
Abbreviations
- AUC:
-
Area under the curve
- BPD:
-
Bronchopulmonary dysplasia
- CI:
-
Confidence interval
- CRIB-II:
-
Clinical Risk Index for Babies-II
- CUS:
-
Cranial ultrasound
- d.f.:
-
Degrees of freedom
- FiO2 :
-
Fraction of inspired oxygen
- HL test:
-
Hosmer-Lemeshow test
- INNC:
-
Indian National Neonatal Collaborative
- IVH:
-
Intraventricular hemorrhage
- NEC:
-
Necrotizing enterocolitis
- NPV:
-
Negative predictive value
- NICU:
-
Neonatal intensive care unit
- OR:
-
Odds ratio
- PaO2:
-
Partial pressure of oxygen in arterial blood
- PPV:
-
Positive predictive value
- PVL:
-
Periventricular leukomalacia
- ROC curve:
-
Receiver operating characteristics curve
- ROP:
-
Retinopathy of prematurity
- SD:
-
Standard deviation
- SGA:
-
Small for gestational age
- SNAP:
-
Score for Neonatal Acute Physiology
- SNAPPE-II:
-
Score for Neonatal Acute Physiology with Perinatal extension-II
References
Tarnow-Mordi W, Ogston S, Wilkinson AR et al (1990) Predicting death from initial disease severity in very low birthweight infants: a method for comparing the performance of neonatal units. BMJ 300(6740):1611–1614. https://doi.org/10.1136/bmj.300.6740.1611
Network TIN (1993) The CRIB (clinical risk index for babies) score: a tool for assessing initial neonatal risk and comparing performance of neonatal intensive care units. Lancet 342(8865):193–198. https://doi.org/10.1016/0140-6736(93)92296-6
Parry G, Tucker J, Tarnow-Mordi W, UK Neonatal Staffing Study Collaborative Group (2003) CRIB II: an update of the clinical risk index for babies score. Lancet 361(9371):1789–1791. https://doi.org/10.1016/S0140-6736(03)13397-1
Richardson DK, Gray JE, McCormick MC, Workman K, Goldmann DA (1993) Score for Neonatal Acute Physiology: a physiologic severity index for neonatal intensive care. Pediatrics 91(3):617–623
Richardson DK, Phibbs CS, Gray JE, McCormick MC, Workman-Daniels K, Goldmann DA (1993) Birth weight and illness severity: independent predictors of neonatal mortality. Pediatrics 91(5):969–975
Richardson DK, Corcoran JD, Escobar GJ, Lee SK (2001) SNAP-II and SNAPPE-II: Simplified newborn illness severity and mortality risk scores. J Pediatr 138(1):92–100. https://doi.org/10.1067/mpd.2001.109608
Radfar M, Hashemieh M, Fallahi M, Masihi R (2018) Utilization of SNAP II and SNAPPE II scores for predicting the mortality rate among a cohort of Iranian newborns. Arch Iran Med 21(4):153–157
Mia RA, Etika R, Harianto A, Indarso F, Damanik S (2016) The use of score for neonatal acute physiology perinatal extension II (SNAPPE II) in predicting neonatal outcome in neonatal intensive care unit. Paediatr Indones 45(6):241–245. https://doi.org/10.14238/pi45.6.2005.241-5
Harsha SS, Archana BR (2015) SNAPPE-II (Score for Neonatal Acute Physiology with Perinatal Extension-II) in Predicting Mortality and Morbidity in NICU. J Clin Diagn Res 9(10):SC10–SC12. https://doi.org/10.7860/JCDR/2015/14848.6677
Rachuri S, Paul S, Jaidev MD (2019) SNAPPE II score: predictor of mortality in NICU. Int J Contemp Pediatr 6:422–426
Muktan D, Singh RR, Bhatta NK, Shah D (2019) Neonatal mortality risk assessment using SNAPPE-II score in a neonatal intensive care unit. BMC Pediatr 19(1):279. https://doi.org/10.1186/s12887-019-1660-y
Ezz-Eldin ZM, Hamid TA, Youssef MR, Hel-D Nabil (2015) Clinical Risk Index for Babies (CRIB II) Scoring System in Prediction of Mortality in Premature Babies. J Clin Diagn Res 9(6):SC08-SC11. https://doi.org/10.7860/JCDR/2015/12248.6012
Rastogi PK, Sreenivas V, Kumar N (2010) Validation of CRIB II for prediction of mortality in premature babies. Indian Pediatr 47(2):145–147. https://doi.org/10.1007/s13312-010-0022-5
Asker HS, Satar M, Yıldızdaş HY, Mutlu B, Özyurt BM, İpek MŞ, Sivaslı E, Taviloğlu Ş, Çelik Y, Özcan K, Burgut R (2016) Evaluation of score for neonatal acute physiology and perinatal extension II and clinical risk index for babies with additional parameters. Pediatr Int 58(10):984–987. https://doi.org/10.1111/ped.12973
Zupancic JA, Richardson DK, Horbar JD, Carpenter JH, Lee SK, Escobar GJ (2007) Revalidation of the score for neonatal acute physiology in the Vermont Oxford Network. Pediatrics 119(1):e156–e163. https://doi.org/10.1542/peds.2005-2957
Greenwood S, Abdel-Latif ME, Bajuk B, Lui K, NSW and ACT Neonatal Intensive Care Units Audit Group (2012) Can the early condition at admission of a high-risk infant aid in the prediction of mortality and poor neurodevelopmental outcome? A population study in Australia. J Paediatr Child Health 48(7):588–595. https://doi.org/10.1111/j.1440-1754.2012.02430.x
Heidarzadeh M, Ghorbani F, Dastgiri S (2016) Prediction value of CRIB-II in outcome of preterm and low birth weight infants: a prospective cohort study. Int J Pediatr 4(4):1583–1589
Sindičić Dessardo N, Jašić M, Dessardo S, Manestar Rukavina K (2016) CRIB II score versus gestational age and birth weight in preterm infant mortality prediction: who will win the bet? Signa Vitae J Intensive Care Emerg Med 11(1):172–181
Hussain F, Gilshenan K, Gray PH (2009) Does lactate level in the first 12 hours of life predict mortality in extremely premature infants? J Paediatr Child Health 45(5):263–267. https://doi.org/10.1111/j.1440-1754.2009.01488.x
Manktelow BN, Draper ES, Field DJ (2010) Predicting neonatal mortality among very preterm infants: a comparison of three versions of the CRIB score. Arch Dis Child Fetal Neonatal Ed 95(1):F9–F13. https://doi.org/10.1136/adc.2008.148015
Bührer C, Metze B, Obladen M (2008) CRIB, CRIB-II, birth weight or gestational age to assess mortality risk in very low birth weight infants? Acta Paediatr 97(7):899–903. https://doi.org/10.1111/j.1651-2227.2008.00793.x
Park JH, Chang YS, Ahn SY, Sung SI, Park WS (2018) Predicting mortality in extremely low birth weight infants: Comparison between gestational age, birth weight, Apgar score, CRIB II score, initial and lowest serum albumin levels. PloS one 13(2):e0192232. https://doi.org/10.1371/journal.pone.0192232
Gagliardi L, Cavazza A, Brunelli A, Battaglioli M, Merazzi D, Tandoi F, Frisone F (2004) Assessing mortality risk in very low birthweight infants: a comparison of CRIB, CRIB-II, and SNAPPE-II. Arch Dis Child Fetal Neonatal Ed 89(5):F419–F422. https://doi.org/10.1136/adc.2003.031286
Sotodate G, Oyama K, Matsumoto A, Konishi Y, Toya Y, Takashimizu N (2022) Predictive ability of neonatal illness severity scores for early death in extremely premature infants. J Matern Fetal Neonatal Med 35(5):846–851. https://doi.org/10.1080/14767058.2020.1731794
Reid S, Bajuk B, Lui K, Sullivan EA, NSW and ACT Neonatal Intensive Care Units Audit Group, PSN (2015) Comparing CRIB- II and SNAPPE- II as mortality predictors for very preterm infants. J Paediatr Child Health 51(5):524–528. https://doi.org/10.1111/jpc.12742
Karaarslan U, Ozlem B, Esra O, Mehmet H (2017) Comparison of CRIB II and SNAPPE II Scoring systems in predicting the mortality and morbidity of Very Low Birth Weight infants. Turkish J Pediatr Dis 3:183–187. https://doi.org/10.12956/tjpd.2017.270
Lee SM, Lee MH, Chang YS (2019) The Clinical Risk Index for Babies II for prediction of time-dependent mortality and short-term morbidities in very low birth weight infants. Neonatology 116(3):244–251. https://doi.org/10.1159/000500270
Phillips LA, Dewhurst CJ, Yoxall CW (2011) The prognostic value of initial blood lactate concentration measurements in very low birthweight infants and their use in development of a new disease severity scoring system. Arch Dis Child Fetal Neonatal Ed 96(4):F275–F280. https://doi.org/10.1136/adc.2010.185793
Sullivan BA, McClure C, Hicks J, Lake DE, Moorman JR, Fairchild KD (2016) Early heart rate characteristics predict death and morbidities in preterm infants. J Pediatr 174:57–62. https://doi.org/10.1016/j.jpeds.2016.03.042
Özcan B, Kavurt AS, Aydemir Ö, Gençtürk Z, Baş AY, Demirel N (2017) SNAPPE-II and risk of neonatal morbidities in very low birth weight preterm infants. Turkish J Pediatr 59(2):105–112. https://doi.org/10.24953/turkjped.2017.02.001
Fortes Filho JB, Dill JC, Ishizaki A, Aguiar WW, Silveira RC, Procianoy RS (2009) Score for Neonatal Acute Physiology and Perinatal Extension II as a predictor of retinopathy of prematurity: study in 304 very-low-birth-weight preterm infants. Ophthalmologica 223(3):177–182. https://doi.org/10.1159/000197114
Fenton TR, Kim JH (2013) A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr 13(1):59. https://doi.org/10.1186/1471-2431-13-59
Jobe AH, Bancalari E (2001) Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163(7):1723–1729. https://doi.org/10.1164/ajrccm.163.7.2011060
Walsh MC, Kliegman RM (1986) Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am 33(1):179–201. https://doi.org/10.1016/S0031-3955(16)34975-6
Volpe J (2017) Preterm intraventricular hemorrhage and post hemorrhagic hydrocephalus. In: Volpe JJ, Inder TE, Perlman JM (eds) Neurology of Newborn, 6th edn. Elseivier, Amsterdam, p 666
de Vries LS, Eken P, Dubowitz LM (1992) The spectrum of leukomalacia using cranial ultrasound. Behav Brain Res 49(1):1–6. https://doi.org/10.1016/S0166-4328(05)80189-5
Early Treatment for Retinopathy of Prematurity Cooperative Group (2003) Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol 121(12):1684. https://doi.org/10.1001/archopht.121.12.1684
McLeod JS, Menon A, Matusko N, Weiner GM, Gadepalli SK, Barks J, Mychaliska GB, Perrone EE (2020) Comparing mortality risk models in VLBW and preterm infants: systematic review and meta-analysis. J Perinatol 18:1–9. https://doi.org/10.1038/s41372-020-0650-0
Author information
Authors and Affiliations
Contributions
Concept of the study: VV, SM, VK; design of study: VV, SM, TO, BS, BT; data acquisition: VV, BT, BS, YM, SS, SSS, VK; analysis: VV, SM, SD; drafting of the work and revising the manuscript: VV, SM, SD, TO. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Statement of ethics
Institutional review board approval (Fernandez Hospital Ethics Committee. Ref. No: 03_2018) was obtained.
Consent to participate and publication
Written informed consent was provided by all parents.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vardhelli, V., Murki, S., Tandur, B. et al. Comparison of CRIB-II with SNAPPE-II for predicting survival and morbidities before hospital discharge in neonates with gestation ≤ 32 weeks: a prospective multicentric observational study. Eur J Pediatr 181, 2831–2838 (2022). https://doi.org/10.1007/s00431-022-04463-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04463-2