Abstract
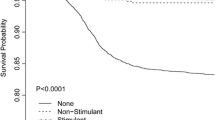
Stimulants have become the most popular psychopharmacologic drugs used in therapy for attention-deficit/hyperactivity disorder (ADHD). Childhood and adolescence are crucial periods for optimizing bone health to prevent osteoporosis-related fractures in old age. However, controversy remains regarding the relationship between stimulant use and bone health. The present study was designed to examine the bone mineral content (BMC) and bone mineral density (BMD) of 5472 individuals aged 8–16 years with or without stimulant use based on National Health and Nutrition Examination Survey (NHANES) 2011–2018 data and to further assess the association between stimulant use and bone health. Among these, 284 (5.2%) participants were using stimulants. In analyses stratified by sex, the BMC and BMD at the level of the lumbar spine, pelvis, and total body were generally lower among stimulant users than among nonusers in males (all P < 0.001), while the differences were not statistically significant in females. In multivariable linear regression models, the increasing range of BMCs and BMDs with age was lower in participants using stimulants than in those not using stimulants after fully adjusting for potential confounding factors. Compared to participants not using stimulants, stimulant use ≥ 3 months was associated with significantly lower BMCs [lumbar spine: β = − 1.35, (95% CI: − 2.56, − 0.14); pelvis: β = − 9.06, (95% CI: − 15.21, − 2.91); and total: β = − 52.96, (95% CI: − 85.87, − 20.04)] and BMDs [pelvis: β = − 0.03, (95% CI: − 0.04, − 0.01), total: β = − 0.01, (95% CI: − 0.02, − 0.00)].
Conclusions: Children and adolescents using stimulants exhibited reductions in BMC and BMD at the lumbar spine, pelvis, and total body compared to those who were not using stimulants, especially among males.
What is Known: • Childhood and adolescence are crucial periods for optimizing bone health to prevent osteoporosis-related fractures in old age. • Controversy remains regarding the relationship between stimulant use and bone health. | |
What is New: • The bone mineral content and bone mineral density at the level of the lumbar spine, pelvis, and total body were generally lower among stimulant users than among nonusers in males, while the differences were not statistically significant in females. • Body mass index and serum alkaline phosphatase may be predictors for loss of bone mineral content and bone mineral density in stimulant users. |

Similar content being viewed by others
Availability of data and material
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
- ADHD:
-
Attention-deficit/hyperactivity disorder
- ALP:
-
Alkaline phosphatase
- BMC:
-
Bone mineral content
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- DA:
-
Dopamine
- DXA:
-
Dual-energy X-ray absorptiometry
- MEC:
-
Mobile examination center
- NCHS:
-
National Center for Health Statistics
- NE:
-
Norepinephrine
- NHANES:
-
National Health and Nutrition Examination Survey
- PIR:
-
Poverty income ratio
- RANKL:
-
Receptor activator of nuclear factor κ-β (NF-κB) ligand
References
Yedavally-Yellayi S, Ho AM, Patalinghug EM (2019) Update on osteoporosis. Prim Care - Clin Off Pract 46:175–190. https://doi.org/10.1016/j.pop.2018.10.014
Drever A (2009) Bone health and osteoporosis Pract Nurse 38:13–22. https://doi.org/10.1016/b978-0-443-06639-9.50027-7
Qaseem A, Forciea MA, McLean RM, Denberg TD (2017) Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American college of physicians. Ann Intern Med 166:818–839. https://doi.org/10.7326/M15-1361
Cosman F, de Beur SJ, LeBoff MS et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381. https://doi.org/10.1007/s00198-014-2794-2
Crabtree NJ, Arabi A, Bachrach LK et al (2014) Dual-energy x-ray absorptiometry interpretation and reporting in children and adolescents: the revised 2013 ISCD pediatric official positions. J Clin Densitom 17:225–242. https://doi.org/10.1016/j.jocd.2014.01.003
Gordon CM, Leonard MB, Zemel BS (2014) 2013 pediatric position development conference: EXECUTIVE summary and reflections. J Clin Densitom 17:219–224. https://doi.org/10.1016/j.jocd.2014.01.007
Ward LM, Konji VN, Ma J (2016) The management of osteoporosis in children. Osteoporos Int 27:2147–2179. https://doi.org/10.1007/s00198-016-3515-9
Grover M, Bachrach LK (2017) Osteoporosis in children with chronic illnesses: diagnosis, monitoring, and treatment. Curr Osteoporos Rep 15:271–282. https://doi.org/10.1007/s11914-017-0371-2
Bachrach LK, Gordon CM (2016) Bone densitometry in children and adolescents. Pediatrics 138. https://doi.org/10.1542/peds.2016-2398
Ma Y, Nyman JS, Tao H et al (2011) β2-adrenergic receptor signaling in osteoblasts contributes to the catabolic effect of glucocorticoids on bone. Endocrinology 152:1412–1422. https://doi.org/10.1210/en.2010-0881
Mosti MP, Flemmen G, Hoff J et al (2016) Impaired skeletal health and neuromuscular function among amphetamine users in clinical treatment. Osteoporos Int 27:1003–1010. https://doi.org/10.1007/s00198-015-3371-z
Lahat E, Weiss M, Ben-Shlomo A et al (2000) Bone mineral density and turnover in children with attention-deficit hyperactivity disorder receiving methylphenidate. J Child Neurol 15:436–439. https://doi.org/10.1177/088307380001500702
Centers for Disease Control and Prevention(CDC) National Health and Nutrition Examination Survey. In: NHANES - Natl. Heal. Nutr. Exam. Surv. Homepage. https://www.cdc.gov/nchs/nhanes/index.htm. Accessed 6 Jan 2021
Centers for Disease Control Prevention(CDC) NHANES Questionnaire Data. https://wwwn.cdc.gov/nchs/nhanes/search/datapage.aspx?Component=Questionnaire. Accessed 6 Jan 2021
Centers for Disease Control and Prevention (CDC) NHANES Examination Data. https://wwwn.cdc.gov/nchs/nhanes/search/datapage.aspx?Component=Examination. Accessed 6 Jan 2021
Polanczyk GV, Salum GA, Sugaya LS et al (2015) Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry Allied Discip 56:345–365. https://doi.org/10.1111/jcpp.12381
Meltzer H, Gatward R, Goodman R, Ford T (2003) Mental health of children and adolescents in Great Britain. Int Rev Psychiatry 15:185–187. https://doi.org/10.1080/0954026021000046155
Feuer AJ, Thai A, Demmer RT, Vogiatzi M (2016) Association of stimulant medication use with bone mass in children and adolescents with attention-deficit/hyperactivity disorder. JAMA Pediatr 170:1–8. https://doi.org/10.1001/jamapediatrics.2016.2804
Howard JT, Walick KS, Rivera JC (2017) Preliminary evidence of an association between ADHD medications and diminished bone health in children and adolescents. J Pediatr Orthop 37:348–354. https://doi.org/10.1097/BPO.0000000000000651
Harstad EB, Weaver AL, Katusic SK et al (2014) ADHD, stimulant treatment, and growth: a longitudinal study. Pediatrics 134:e935–e944. https://doi.org/10.1542/peds.2014-0428
Collins MT, Stratakis CA (2016) Bone formation, growth, and repair. Horm Metab Res 48:687–688. https://doi.org/10.1055/s-0042-119907
Bailey DA, McKay HA, Mirwald RL et al (1999) A six-year longitudinal study of the relationship of physical activity to bone mineral accrual in growing children: the University of Saskatchewan Bone Mineral Accrual Study. J Bone Miner Res 14:1672–1679. https://doi.org/10.1359/jbmr.1999.14.10.1672
Poulton A, Briody J, McCorquodale T et al (2012) Weight loss on stimulant medication: how does it affect body composition and bone metabolism? – a prospective longitudinal study. Int J Pediatr Endocrinol 2012:1. https://doi.org/10.1186/1687-9856-2012-30
Poulton AS, Bui Q, Melzer E, Evans R (2016) Stimulant medication effects on growth and bone age in children with attention-deficit/hyperactivity disorder: a prospective cohort study. Int Clin Psychopharmacol 31:93–99. https://doi.org/10.1097/YIC.0000000000000109
Chuang TL, Chuang MH, Lin CH et al (2020) Significant association factors of bone mineral density in Taiwan adults. Tzu Chi Med J 32:367–372. https://doi.org/10.4103/tcmj.tcmj_113_19
Fong CY, Kong AN, Noordin M et al (2018) Determinants of low bone mineral density in children with epilepsy. Eur J Paediatr Neurol 22:155–163. https://doi.org/10.1016/j.ejpn.2017.10.007
Iki M, Akiba T, Matsumoto T et al (2004) Reference database of biochemical markers of bone turnover for the Japanese female population. Japanese Population-based Osteoporosis (JPOS) Study. Osteoporos Int 15:981–991. https://doi.org/10.1007/s00198-004-1634-1
Fu L, Patel MS, Bradley A et al (2005) The molecular clock mediates leptin-regulated bone formation. Cell 122:803–815. https://doi.org/10.1016/j.cell.2005.06.028
Colussi-Mas J, Panayi F, Scarna H et al (2005) Blockade of β-adrenergic receptors prevents amphetamine-induced behavioural sensitization in rats: a putative role of the bed nucleus of the stria terminalis. Int J Neuropsychopharmacol 8:569–581. https://doi.org/10.1017/S1461145705005298
Challman TD, Lipsky JJ (2000) Methylphenidate: its pharmacology and uses. Mayo Clin Proc 75:711–721. https://doi.org/10.4065/75.7.711
Aitken SJ, Landao-Bassonga E, Ralston SH, Idris AI (2009) β2-adrenoreceptor ligands regulate osteoclast differentiation in vitro by direct and indirect mechanisms. Arch Biochem Biophys 482:96–103. https://doi.org/10.1016/j.abb.2008.11.012
Elefteriou F (2008) Regulation of bone remodeling by the central and peripheral nervous system. Arch Biochem Biophys 473:231–236. https://doi.org/10.1016/j.abb.2008.03.016
Elefteriou F, Campbell P, Ma Y (2014) Control of bone remodeling by the peripheral sympathetic nervous system. Calcif Tissue Int 94:140–151. https://doi.org/10.1007/s00223-013-9752-4
Karsenty G (2020) The central regulation of bone mass: genetic evidence and molecular bases. Handb Exp Pharmacol 262:309–323. https://doi.org/10.1007/164_2020_378
Takeda S, Karsenty G (2008) Molecular bases of the sympathetic regulation of bone mass. Bone 42:837–840. https://doi.org/10.1016/j.bone.2008.01.005
Gordeladze JO, Drevon CA, Syversen U, Reseland JE (2002) Leptin stimulates human osteoblastic cell proliferation, de novo collagen synthesis, and mineralization: impact on differentiation markers, apoptosis, and osteoclastic signaling. J Cell Biochem 85:825–836. https://doi.org/10.1002/jcb.10156
Holloway WR, Collier FML, Aitken CJ et al (2002) Leptin inhibits osteoclast generation. J Bone Miner Res 17:200–209. https://doi.org/10.1359/jbmr.2002.17.2.200
City SL (1985) Role of the dopamine uptake carrier in the neurochemical response to methamphetamine: effects of amfonelic acid 109:73–80
Burrows KB, Gudelsky G, Yamamoto BK (2000) Rapid and transient inhibition of mitochondrial function following methamphetamine or 3,4-methylenedioxymethamphetamine administration. Microscopy 11–18
Thomas DM, Walker PD, Benjamins JA et al (2004) Methamphetamine neurotoxicity in dopamine nerve endings of the striatum is associated with microglial activation. J Pharmacol Exp Ther 311:1–7. https://doi.org/10.1124/jpet.104.070961
Negrao BL, Viljoen M (2011) Stimulants and growth in children with attention-deficit/hyperactivity disorder. Med Hypotheses 77:21–28. https://doi.org/10.1016/j.mehy.2011.03.015
Gómez-Bruton A, Matute-Llorente Á, González-Agüero A et al (2017) Plyometric exercise and bone health in children and adolescents: a systematic review. World J Pediatr 13:112–121. https://doi.org/10.1007/s12519-016-0076-0
Händel MN, Heitmann BL, Abrahamsen B (2015) Nutrient and food intakes in early life and risk of childhood fractures: a systematic review and meta-analysis. Am J Clin Nutr 102:1182–1195. https://doi.org/10.3945/ajcn.115.108456
Specker B, Thiex NW, Sudhagoni RG (2015) Does exercise influence pediatric bone? A systematic REVIEW. Clin Orthop Relat Res 473:3658–3672. https://doi.org/10.1007/s11999-015-4467-7
Golden NH, Abrams SA, Daniels SR et al (2014) Optimizing bone health in children and adolescents. Pediatrics 134:e1229–e1243. https://doi.org/10.1542/peds.2014-2173
Rice JN, Gillett CB, Malas NM (2018) The impact of psychotropic medications on bone health in youth. Curr Psychiatry Rep 20. https://doi.org/10.1007/s11920-018-0960-5
Schneider BN, Enenbach M (2014) Managing the risks of ADHD treatments. Curr Psychiatry Rep 16. https://doi.org/10.1007/s11920-014-0479-3
Funding
This work is supported by grants from the Natural Science Foundation of Shandong Province (ZR201808010011), the Science Foundation of Qilu Hospital of Shandong University (2019QLQN28), and the National Natural Science Foundation of China (82171352).
Author information
Authors and Affiliations
Contributions
YAF and GW contributed to the study conception and design, collected the data, wrote the first draft, performed the data analysis, and revised the manuscript. JHL contributed to the study conception and design and collected and analyzed the data. ML, MD, CZ, and RX contributed to the data analysis and reviewed and revised the manuscript. XJL contributed to the study conception and design, performed the data analysis, and revised the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The survey protocol was approved by the Centers for Disease Control and Prevention (CDC) and the National Center for Health Statistics (NCHS) Ethics Review Board, and all participants provided written informed consent.
Consent to participate
All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Gregorio Paolo Milani
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fu, Y., Wang, G., Liu, J. et al. Stimulant use and bone health in US children and adolescents: analysis of the NHANES data. Eur J Pediatr 181, 1633–1642 (2022). https://doi.org/10.1007/s00431-021-04356-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04356-w