Abstract
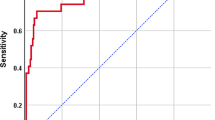
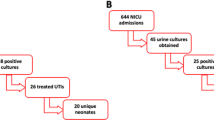
One previous study recommended oral and outpatient management for those infants aged 60–90 days with urinary tract infection (UTI) meeting the low-risk criteria identified: to be well-appearing and to have a procalcitonin value of < 0.7 ng/mL. A retrospective study was conducted, including infants aged 29 to 90 days with UTI from 2014 to 2019, to validate these low-risk criteria identified and determine the adherence to the new algorithm for managing these patients at the Emergency Department. Two hundred one patients were included; 105 (52.2%) were aged 60 to 90 days. Twelve (6%, 95% CI 3.4–10.1%) had bacteremia. One hundred thirty-six (67.7%) infants met low-risk criteria; none had a positive blood culture (0%, 95% CI 0–2.7%). Overall protocol adherence was 90.6%. One hundred and forty-four (71.6%) infants were admitted to the hospital; all patients meeting high-risk criteria were hospitalized. Among the 57 (28.4%) infants initially sent home, 4 (7.0%) required later hospital admission.
Conclusions: A prediction rule including general appearance and procalcitonin is highly accurate in identifying young infants with UTI at low risk for bacteremia. Outpatient management with appropriate follow-up is safe for these infants.
What is Known: • Patients under 2–3 months of age with a presumptive urinary tract infection (UTI) are commonly hospitalized because of concerns regarding concomitant bacteremia. | |
What is New: • A prediction rule including general appearance and procalcitonin is highly accurate in identifying young infants with UTI at low risk for bacteremia. Outpatient management with appropriate follow-up is safe for these infants. |

Similar content being viewed by others
Availability of data and material
Raw data are available upon reasonable request (correspondence author).
Abbreviations
- BC:
-
Blood culture
- CSF:
-
Cerebrospinal fluid
- CI:
-
Confidence interval
- ED:
-
Emergency Department
- GBS:
-
Group B Streptococcus
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- NPV:
-
Negative predictive value
- PAT:
-
Pediatric Assessment Triangle
- PCT:
-
Procalcitonin
- SBI:
-
Serious bacterial infection
- UC:
-
Urine culture
- UTI:
-
Urinary tract infection
References
Byington CL, Rittichier KK, Bassett KE, Castillo H, Glasgow TS, Daly J, Pavia AT (2003) Serious bacterial infections in febrile infants younger than 90 days of age: the importance of ampicillin-resistant pathogens. Pediatrics 111:964–968. https://doi.org/10.1542/peds.111.5.964
Morley EJ, Lapoint JM, Roy LW, Cantor R, Grant WD, Paolo WF, Wojcik S (2012) Rates of positive blood, urine, and cerebrospinal fluid cultures in children younger than 60 days during the vaccination era. Pediatr Emerg Care 28:125–130. https://doi.org/10.1097/PEC.0b013e318243fa50
Herr SM, Wald ER, Pitetti RD, Choi SS (2001) Enhanced urinalysis improves identification of febrile infants ages 60 days and younger at low risk for serious bacterial illness. Pediatrics 108:866–871. https://doi.org/10.1542/peds.108.4.866
Zorc JJ, Levine DA, Platt SL et al (2005) Clinical and demographic factors associated with urinary tract infection in young febrile infants. Pediatrics 116:644–648. https://doi.org/10.1542/peds.2004-1825
Hoberman A, Wald ER, Hickey RW, Baskin M, Charron M, Majd M, Kearney DH, Reynolds EA, Ruley J, Janosky JE (1999) Oral versus initial intravenous therapy for urinary tract infections in young febrile children. Pediatrics 104:79–86. https://doi.org/10.1542/peds.104.1.79
Honkinen O, Jahnukainen T, Mertsola, Eskola J, Ruuskanen O (2000) Bacteremic urinary tract infection in children. Pediatr Infect Dis J 19:630–634. https://doi.org/10.1097/00006454-200007000-00009
Bachur R, Caputo GL (1995) Bacteremia and meningitis among infants with urinary tract infections. Pediatr Emerg Care 11:280–284. https://doi.org/10.1097/00006565-199510000-00004
Dayan PS, Hanson E, Bennett JE, Langsam D, Miller SZ (2004) Clinical course of urinary tract infections in infants younger than 60 days of age. Pediatr Emerg Care 20:85–88. https://doi.org/10.1097/01.pec.0000113876.10140.9b
Montini G, Toffolo A, Zucchetta P et al (2007) Antibiotic treatment for pyelonephritis in children: multicentre randomised controlled non-inferiority trial. Br Med J 335:386–388. https://doi.org/10.1136/bmj.39244.692442.55
Bocquet N, Alaoui AS, Jais JP, Gajdos V, Guigonis V, Lacour B, Chéron G (2012) Randomized trial of oral versus sequential iv/oral antibiotic for acute pyelonephritis in children. Pediatrics 129: e269-e275. https://doi.org/10.1542/peds.2011-0814
Okarska-Napierała M, Wasilewska A, Kuchar E (2017) Urinary tract infection in children: diagnosis, treatment, imaging—comparison of current guidelines. J Pediatr Urol 13:567–573. https://doi.org/10.1016/j.jpurol.2017.07.018
Mattoo TK, Shaikh N, Nelson CP (2021) Contemporary management of urinary tract infection in children. Pediatrics 147:e2020012138. https://doi.org/10.1542/peds.2020-012138
Buettcher M, Trueck J, Niederer-Loher A et al (2021) Swiss consensus recommendations on urinary tract infections in children. Eur J Pediatr. 180:663–674. https://doi.org/10.1007/s00431-020-03714-4
Hernández-Bou S, Trenchs V, Alarcón M, Luaces C (2014) Afebrile very young infants with urinary tract infection and the risk for bacteremia. Pediatr Infect Dis J 33:244–247. https://doi.org/10.1097/INF.0000000000000033
Dieckmann RA, Brownstein D, Gausche-Hill M (2010) The pediatric assessment triangle: a novel approach for the rapid evaluation of children. Pediatr Emerg Care 26:312–315. https://doi.org/10.1097/PEC.0b013e3181d6db37
Schnadower D, Kuppermann N, Macias CG et al (2010) Febrile infants with urinary tract infections at very low risk for adverse events and bacteremia. Pediatrics 126:1074–1083. https://doi.org/10.1542/peds.2010-0479
Nugent J, Childers M, Singh-Miller N, Howard R, Allard R, Eberly M (2019) Risk of meningitis in infants aged 29 to 90 days with urinary tract infection: a systematic review and meta-analysis. J Pediatr 212:102–110. https://doi.org/10.1016/j.jpeds.2019.04.053
Velasco R, Lejarzegi A, Gomez B et al (2020) Febrile young infants with abnormal urine dipstick at low risk of invasive bacterial infection. Arch Dis Child 2020–320468 (Online ahead of print) https://doi.org/10.1136/archdischild-2020-320468
Sarvis AB, Sarvis RC, Schnadower D, Chamberlain JM, Mathison DJ (2019) Admit versus discharge—a cost analysis of infants 29 to 60 days old with febrile urinary tract infection at low risk for bacteremia. Acad Pediatr 19:209−215. https://doi.org/10.1016/j.acap.2018.11.002
Chaudhari PP, Monuteaux MC, Bachur RG (2019) Management of urinary tract infections in young children: balancing admission with the risk of emergency department revisits. Acad Pediatr 19:203–208. https://doi.org/10.1016/j.acap.2018.05.011
Schnadower D, Kuppermann N, Macias CG, Freedman SB, Agrawal D, Mao J, Dayan PS, American Academy of Pediatrics Pediatric Emergency Medicine Collaborative Research Committee UTI Study Group (2014) Outpatient management of young febrile infants with urinary tract infections. Pediatr Emerg Care 30:591–597. https://doi.org/10.1097/PEC.0000000000000202
Gómez B, Mintegi S, Benito J, Egireun A, Garcia D, Astobiza E (2010) Blood culture and bacteremia predictors in infants less than three months of age with fever without source. Pediatr Infect Dis J 29:43–47. https://doi.org/10.1097/INF.0b013e3181c6dd14
Irwin AD, Grant A, Williams R et al (2017) Predicting risk of serious bacterial infections in febrile children in the emergency department. Pediatrics 140:e20162853. https://doi.org/10.1542/peds.2016-2853
Edlin RS, Shapiro DJ, Hersh AL, Copp HL (2013) Antibiotic resistance patterns of outpatient pediatric urinary tract infections. J Urol 90: 222–227. https://doi.org/10.1016/j.juro.2013.01.069
Erol B, Culpan M, Caskurlu H, Sari U, Cag Y, Vahaboglu H, Özumut SH, Karaman MI, Caskurlu T (2018) Changes in antimicrobial resistance and demographics of UTIs in pediatric patients in a single institution over a 6-year period. J Pediatr Urol 14:176.e1–176.e5. https://doi.org/10.1016/j.jpurol.2017.12.002
Author information
Authors and Affiliations
Contributions
SHB: conceptualized and designed the study, enrolled patients, analyzed and interpreted data, drafted the initial manuscript, and revised and approved the final manuscript as submitted. VT: conceptualized and designed the study, was involved in obtaining ethics approval, enrolled patients, analyzed and interpreted data, revised the manuscript, and approved the final manuscript as submitted. ASG, MC, and MC: did data collection and approved the final manuscript as submitted. CL: provided critical review of the original and subsequent manuscript drafts, and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the hospital’s Ethics Committee (PIC-65–19). Since the data were extracted from a registry, the information contained in it was anonymous, and since no interventions were performed on patients, informed consent was not required or requested.
Conflicts of interest
The authors declare no competing interests.
Additional information
Communicated by Nicole Ritz
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hernández-Bou, S., Trenchs, V., Soler-Garcia, A. et al. Outpatient and oral management is suitable for infants 60–90 days old with urinary tract infections at low risk of bacteremia. Eur J Pediatr 181, 671–677 (2022). https://doi.org/10.1007/s00431-021-04224-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04224-7