Abstract
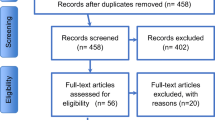
Preterm infants with severe brain injury are at high risk for poor outcomes and, therefore, may benefit from developmental care modalities such as music therapy (MT). In this prospective, randomized intervention, preterm infants with severe brain injury (grade 3 or 4 intraventricular hemorrhage or periventricular leukomalacia) who underwent skin-to-skin contact (SSC) with or without maternal singing during MT were evaluated for physiological responses, including autonomic nervous system stability (low frequency (LF)/high frequency (HF) power), heart rate, respiratory rate, oxygen saturation, and behavioral state. Maternal anxiety state and physiological data were also evaluated. A total of 35 preterm infants with severe brain injuries were included in the study analysis. Higher mean ± standard deviation (SD) LF/HF ratio (1.8 ± 0.7 vs. 1.1 ± 0.25, p = 0.01), higher mean ± SD heart rate (145 ± 15 vs. 132 ± 12 beats per minute, p = 0.04), higher median (interquartile range) infant behavioral state (NIDCAP manual for naturalistic observation and the Brazelton Neonatal Behavioral Assessment) score (3 (2–5) vs. 1 (1–3), p = 0.03), and higher mean ± SD maternal anxiety (state-trait anxiety inventory) score (39.1 ± 10.4 vs. 31.5 ± 7.3, p = 0.04) were documented in SSC combined with maternal singing during MT, as compared to SSC alone.
Conclusion: Maternal singing during MT for preterm infants with severe brain injury induces physiological and behavioral instability and increases maternal anxiety during NICU hospitalization. A unique MT intervention should be designed for preterm infants with severe brain injury and their mothers.
What is Known: • Preterm infants with severe brain injury are at high risk for poor outcomes. • Music therapy benefits brain development of preterm infants without severe brain injury, however it is unknown whether maternal singing during music therapy for preterm infants with severe brain injury is beneficial. | |
What is New: • Maternal singing during music therapy for preterm infants with severe brain injury induces physiological and behavioral instability and increases maternal anxiety during NICU hospitalization. • A unique music therapy intervention should be designed for preterm infants with severe brain injury and their mothers. |

Similar content being viewed by others
Data availability
Data will be made available upon request.
Abbreviations
- HF:
-
High frequency
- HRV:
-
Heart rate variability
- IVH:
-
Intraventricular hemorrhage
- LF:
-
Low frequency
- MT:
-
Music therapy
- NICU:
-
Neonatal intensive care unit
- NIDCAP:
-
Neonatal Individualized Developmental Care and Assessment Program
- PVL:
-
Periventricular leukomalacia
- SD:
-
Standard deviation
- SSC:
-
Skin-to-Skin contact
- STAI:
-
State-trait anxiety inventory
References
Hinojosa-Rodríguez M, Harmony T, Carrillo-Prado C, Van Horn JD, Irimia A, Torgerson C, Jacokes Z (2017) Clinical neuroimaging in the preterm infant: diagnosis and prognosis. NeuroImage Clin 16:355–368. https://doi.org/10.1016/j.nicl.2017.08.015
De Vries LS, Benders MJNL, Groenendaal F (2015) Progress in Neonatal Neurology with a focus on neuroimaging in the preterm infant. Neuropediatrics 46:234–241. https://doi.org/10.1055/s-0035-1554102
Pace CC, Spittle AJ, Molesworth CML, Lee KJ, Northam EA, Cheong JLY, Davis PG, Doyle LW, Treyvaud K, Anderson PJ (2016) Evolution of depression and anxiety symptoms in parents of very preterm infants during the newborn period. JAMA Pediatr 170:863–870. https://doi.org/10.1001/jamapediatrics.2016.0810
Trumello C, Candelori C, Cofini M, Cimino S, Cerniglia L, Paciello M, Babore A (2018) Mothers’ depression, anxiety, and mental representations after preterm birth: a study during the infant’s hospitalization in a neonatal intensive care unit. Front Public Health 6:1–9. https://doi.org/10.3389/fpubh.2018.00359
Winter L, Colditz PB, Sanders MR, Boyd RN, Pritchard M, Gray PH, Whittingham K, Forrest K, Leeks R, Webb L, Marquart L, Taylor K, Macey J (2018) Depression, posttraumatic stress and relationship distress in parents of very preterm infants. Arch Womens Ment Health 21:445–451. https://doi.org/10.1007/s00737-018-0821-6
Yaman S, Altay N (2015) Posttraumatic stress and experiences of parents with a newborn in the neonatal intensive care unit. J Reprod Infant Psychol 33:140–152. https://doi.org/10.1080/02646838.2014.990872
Ballantyne M, Orava T, Bernardo S, McPherson AC, Church P, Fehlings D (2017) Parents’ early healthcare transition experiences with preterm and acutely ill infants: a scoping review. Child Care Health Dev 43:783–796. https://doi.org/10.1111/cch.12458
Gogou M, Haidopoulou K, Pavlou E (2019) Sleep and prematurity: sleep outcomes in preterm children and influencing factors. World J Pediatr 15:209–218. https://doi.org/10.1007/s12519-019-00240-8.30830664
Als H, Gilkerson L (1997) The role of relationship-based developmentally supportive newborn intensive care in strengthening outcome of preterm infants. Semin Perinatol 21:178–189. https://doi.org/10.1016/S0146-0005(97)80062-6
Gonya J, Ray WC, Rumpf RW, Brock G (2017) Investigating skin-to-skin care patterns with extremely preterm infants in the NICU and their effect on early cognitive and communication performance: A retrospective cohort study. BMJ Open 7:1–9. https://doi.org/10.1136/bmjopen-2016-012985
World federation of music therapy (2008-2017). http://wfmt.info/wfmt-new-home/about-wfmt/
Robb SL, Carpenter JS, Burns DS (2011) Reporting guidelines for music-based interventions. J Health Psychol 16:342–352. https://doi.org/10.1177/1359105310374781
Lordier L, Loukas S, Grouiller F, Vollenweider A, Vasung L, Meskaldij DE, Lejeune F, Pittet MP, Borradori-Tolsa C, Lazeyras F, Grandjean D, Van De Ville D, Hüppi PS (2019) Music processing in preterm and full-term newborns: a psychophysiological interaction (PPI) approach in neonatal fMRI. Neuroimage 185:857–864. https://doi.org/10.1016/j.neuroimage.2018.03.078
Haslbeck FB, Jakab A, Held U, Bassler D, Bucher HU, Hagmann C (2020) Creative music therapy to promote brain function and brain structure in preterm infants: a randomized controlled pilot study. NeuroImage Clin 25:102171. https://doi.org/10.1016/j.nicl.2020.102171
Haslbeck FB, Bassler D (2018) Music from the very beginning—a neuroscience-based framework for music as therapy for preterm infants and their parents. Front Behav Neurosci 12:1–7. https://doi.org/10.3389/fnbeh.2018.00112
Palazzi A, Nunes CC, Piccinini CA (2018) Music therapy and musical stimulation in the context of prematurity: a narrative literature review from 2010–2015. J Clin Nurs 27:e1–e20. https://doi.org/10.1111/jocn.13893
Loewy J, Stewart K, Dassler AM, Telsey A, Homel P (2013) The effects of music therapy on vital signs, feeding, and sleep in premature infants. Pediatrics 131:902–918. https://doi.org/10.1542/peds.2012-1367
Arnon S, Diamant C, Bauer S, Regev R, Sirota G, Litmanovitz I (2014) Maternal singing during kangaroo care led to autonomic stability in preterm infants and reduced maternal anxiety. Acta Paediatr Int J Paediatr 103:1039–1044. https://doi.org/10.1111/apa.12744
Bieleninik Ł, Ghetti C, Gold C (2016) Music therapy for preterm infants and their parents: a meta-analysis. Pediatrics 138:e20160971. https://doi.org/10.1542/peds.2016-0971
Graven SN (2000) Sound and the developing infant in the NICU: conclusions and recommendations for care. J Perinatol 20:S88–S93. https://doi.org/10.1038/sj.jp.7200444
Julian LJ (2011) Measures of anxiety: state-trait anxiety inventory (STAI), Beck anxiety inventory (BAI), and hospital anxiety and depression scale-anxiety (HADS-A). Arthritis Care Res (Hoboken) 63(Suppl 11(0 11)):S467–S472. https://doi.org/10.1002/acr.20561
Netz Y, Zeav A, Arnon M, Daniel S (2005) Translating a single-word items scale with multiple subcomponents – a Hebrew translation of the profile of mood states. Isr J Psychiatry Relat 42:263–270
Als H, Lawhon G, Brown E, Gibes R, Duffy FH, McAnulty G, Blickman JG (1986) Individualized behavioral and environmental care for the very low birth weight preterm infant at risk for bronchopulmonary dysplasia: neonatal intensive care unit and developmental outcomes. Pediatrics 78:1123–1132
Brazelton TB, Nugent JK (2011) The neonatal behavioral assessment scale. Mac Keith Press, Cambridge
Kleberg A, Westrup B, Stjernqvist K, Lagercrantz H (2002) Indications of improved cognitive development at one year of age among infants born very prematurely who received care based on the Newborn Individualized Developmental Care and Assessment Program (NIDCAP). Early Hum Dev 68:83–91. https://doi.org/10.1016/S0378-3782(02)00014-2
Haslbeck FB, Stegemann T (2018) The effect of music therapy on infants born preterm. Dev Med Child Neurol 60:217. https://doi.org/10.1111/dmcn.13677
Nelson MN, White-Traut RC, Vasan U, Silvestri J, Comiskey E, Meleedy-Rey P, Littau S, Gu G, Patel M (2001) One-year outcome of auditory-tactile-visual-vestibular intervention in the neonatal intensive care unit: effects of severe prematurity and central nervous system injury. J Child Neurol 16:493–498. https://doi.org/10.1177/088307380101600706
Haslbeck FB (2014) Creative music therapy with premature infants: an analysis of video footage. Nord J Music Ther 23:5–35. https://doi.org/10.1080/08098131.2013.780091
Standley JM, Gutierrez C (2020) Benefits of a comprehensive evidence-based NICU-MT Program: family-therapy for premature infants. Pediatr Nurs 46:40–46
Ettenberger M, Rojas Cárdenas C, Parker M, Odell-Miller H (2017) Family-centred music therapy with preterm infants and their parents in the neonatal intensive care unit (NICU) in Colombia–a mixed-methods study. Nord J Music Ther 26:207–234. https://doi.org/10.1080/08098131.2016.1205650
Haslbeck FB, Bassler D (2020) Clinical practice protocol of creative music therapy for preterm infants and their parents in the neonatal intensive care unit. J Vis Exp 2020:1–10. https://doi.org/10.3791/60412
Standley J (2012) Music therapy research in the NICU: an updated meta-analysis. Neonatal Netw 31:311–316. https://doi.org/10.1891/0730-0832.31.5.311
Ghetti C, Bieleninik Ł, Hysing M, Kvestad I, Assmus J, Romeo R et al (2019) Longitudinal study of music therapy’s effectiveness for premature infants and their caregivers (LongSTEP): protocol for an international randomised trial. BMJ Open 9:e025062. https://doi.org/10.1136/bmjopen-2018-025062
Ryckman J, Hilton C, Rogers C, Pineda R (2017) Sensory processing disorder in preterm infants during early childhood and relationships to early neurobehavior. Early Hum Dev 113:18–22. https://doi.org/10.1016/j.earlhumdev.2017.07.012
Wickremasinghe AC, Rogers EE, Johnson BC, Shen A, Barkovich AJ, Marco EJ (2013) Children born prematurely have atypical sensory profiles. J Perinatol 33:631–635. https://doi.org/10.1038/jp.2013.12
Adams-Chapman I (2009) Insults to the developing brain and impact on neurodevelopmental outcome. J Commun Disord 42:256–262. https://doi.org/10.1016/j.jcomdis.2009.03.010
Eeles AL, Anderson PJ, Brown NC, Lee KJ, Boyd RN, Spittle AJ, Doyle LW (2013) Sensory profiles of children born <30 weeks’ gestation at 2 years of age and their environmental and biological predictors. Early Hum Dev 89:727–732. https://doi.org/10.1016/j.earlhumdev.2013.05.005
White-Traut RC, Nelson MN, Silvestri JM, Patel M, Berbaum M, Gu GG, Rey PM (2004) Developmental patterns of physiological response to a multisensory intervention in extremely premature and high-risk infants. J Obstet Gynecol Neonatal Nurs 33:266–275. https://doi.org/10.1177/0884217504263289
Gima H, Ohgi S, Fujiwara T, Abe K (2010) Stress behavior in premature infants with periventricular leukomalacia. J Phys Ther Sci 22:109–115. https://doi.org/10.1589/jpts.22.109
Harrison LL, Roane C, Weaver M (2004) The relationship between physiological and behavioral measures of stress in preterm infants. J Obstet Gynecol Neonatal Nurs 33:236–245. https://doi.org/10.1177/0884217504263293
Lipner HS, Huron RF (2018) Developmental and interprofessional care of the preterm infant: neonatal intensive care unit through high-risk infant follow-up. Pediatr Clin N Am 65:135–141. https://doi.org/10.1016/j.pcl.2017.08.026
Williams MD, Lascelles BDX (2020) Early neonatal pain—a review of clinical and experimental implications on painful conditions later in life. Front Pediatr 8:30. https://doi.org/10.3389/fped.2020.00030
Koelsch S (2014) Brain correlates of music-evoked emotions. Nat Rev Neurosci 15:170–180. https://doi.org/10.1038/nrn3666
Foroushani SM, Herman CA, Wiseman CA, Anthony CM, Drury SS, Howell MP (2020) Evaluating physiologic outcomes of music interventions in the neonatal intensive care unit: a systematic review. J Perinatol 31:11–15. https://doi.org/10.1038/s41372-020-0756-4
Filippa M, Lordier L, De Almeida JS, Monaci MG, Adam-Darque A, Grandjean D, Kuhn P, Hüppi PS (2020) Early vocal contact and music in the NICU: new insights into preventive interventions. Pediatr Res 87:249–264. https://doi.org/10.1038/s41390-019-0490-9
Author information
Authors and Affiliations
Contributions
Shulamit Epstein contributed to the study conception, design, material preparation and data collection. Sofia Bauer contributed to the study conception. Orly Levkovits Stern contributed to the study design. Ita Litmanovitz contributed to the study methodology and outcome assessments. Cochavit Elefant contributed to the study conception and wrote the first draft. Dana Yakobson contributed to the study methodology and conducted the music therapy intervention. Shmuel Arnon contributed to the study design, data collection and analysis and manuscript preparation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study was approved by the Institutional Review Board of Meir Medical Center and conducted in accordance with the ethical and humane principles of research established by the Declaration of Helsinki (trial registration number NCT 01427894).
Consent to participate
Written informed consent was obtained from all parents.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Communicated by Daniele De Luca
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Epstein, S., Bauer, S., Levkovitz Stern, O. et al. Preterm infants with severe brain injury demonstrate unstable physiological responses during maternal singing with music therapy: a randomized controlled study. Eur J Pediatr 180, 1403–1412 (2021). https://doi.org/10.1007/s00431-020-03890-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-020-03890-3