Abstract
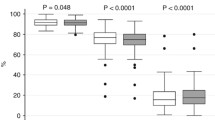
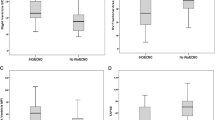
The relationship between right ventricular (RV) function and cerebral blood flow (CBF) velocity and cerebral oxygenation was assessed in neonates with hypoxic-ischemic encephalopathy (HIE) treated with therapeutic hypothermia (TH). Echocardiographic, transcranial Doppler, and hemodynamic data from 37 neonates with moderate-severe HIE + TH were reviewed. Twenty healthy newborns served as controls. Cardiac dysfunction in HIE + TH was characterized by a predominant RV dysfunction, with concomitantly reduced CBF velocity. A significant correlation was found between CBF velocity and tricuspid annular plane systolic excursion (TAPSE), RV output (RVO), and stroke volume (SVRV), as well as with left ventricular output and stroke volume. Brain oxygenation (rSO2) correlated significantly with RVO, SVRV, TAPSE, ejection fraction, and fractional shortening, whereas cerebral fractional tissue oxygen extraction (FTOEc) correlated with RVO, SVRV, RV myocardial performance index, and superior vena cava flow. CBF velocity and cerebral NIRS correlations were stronger with parameters of right ventricular performance.
Conclusion: CBF velocity and brain oxygenation correlate predominantly with RV function in HIE + TH. This suggests a preferential contribution of RV performance to cerebral hemodynamics in this context.
What is Known: • Neonates with hypoxic ischemic encephalopathy frequently exhibit alterations of cardiac function and cerebral blood flow. • These are considered organ-specific consequences of perinatal asphyxia. What is New: • We show that cerebral blood flow velocity and brain oxygenation are correlated predominantly with right ventricular function during therapeutic hypothermia. • This suggests a potential direct contribution of right ventricular performance to cerebral hemodynamics in this context. |

Similar content being viewed by others
Abbreviations
- BP:
-
Blood pressure
- CBF:
-
Cerebral blood flow
- cFTOE:
-
Cerebral fractional tissue oxygen extraction
- CO:
-
Cardiac output
- CrSO2:
-
Cerebral regional oxygen saturation
- CTnI:
-
Cardiac troponin I
- EDV:
-
End diastolic velocity
- EF:
-
Ejection fraction
- FS:
-
Fractional shortening
- FTOE:
-
Fractional tissue oxygen extraction
- HIE:
-
Hypoxic-ischemic encephalopathy
- HR:
-
Heart rate
- IQR:
-
Inter quartile range
- LFESD:
-
Left ventricular end systolic diameters
- LV:
-
Left ventricle
- LVEDD:
-
Left ventricular end diastolic diameter
- LVET:
-
Left ventricular ejection time
- LVO:
-
Left ventricular output
- MCA:
-
Mean cerebral artery
- MPI:
-
Myocardial performance index or Tei index
- MPILV :
-
Left ventricular myocardial performance index or Tei index
- MPIRV :
-
Right ventricular myocardial performance index or Tei index
- NICU:
-
Neonatal intensive care unit
- NIRS:
-
Near-infrared spectroscopy
- NPE:
-
Neonatologist-performed echocardiography
- PAAT:
-
Pulmonary artery accelerating time
- PDA:
-
Patent ductus arteriosus
- PFO:
-
Patent foramen ovale
- PH:
-
Pulmonary hypertension
- PSV:
-
Peak systolic velocity
- PVR:
-
Pulmonary vascular resistance
- RI:
-
Resistive index
- rSO2:
-
Regional oxygen saturation
- RV:
-
Right ventricle
- RVET:
-
Right ventricular ejection time
- RVO:
-
Right ventricular output
- SrSO2:
-
Somatic regional oxygen saturation
- SV:
-
Stroke volume
- SVCF:
-
Superior vena cava flow
- SVLV :
-
Left ventricular stroke volume
- SVRV :
-
Right ventricular stroke volume
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TH:
-
Therapeutic hypothermia
- TPV:
-
Time to peak velocity
- VTI:
-
Velocity time integral
- D:
-
Diameter
References
Giesinger RE, Bailey LJ, Deshpande P, McNamara PJ (2017) Hypoxic-ischemic encephalopathy and therapeutic hypothermia: the hemodynamic perspective. J Pediatr 180:22–30.e2
Tagin MA, Woolcott CG, Vincer MJ, Whyte RK, Stinson DA (2012) Hypothermia for neonatal hypoxic ischemic encephalopathy. An updated systematic review and meta-analysis. Arch Pediatr Adolesc Med 166:558–566
Azzopardi DV, Strohm B, Edwards AD, Dyet L, Halliday HL, Juszczak E, Kapellou O, Levene M, Marlow N, Porter E, Thoresen M, Whitelaw A, Brocklehurst P, TOBY Study Group (2009) Moderate hypothermia to treat perinatal asphyxial encephalopathy. N Engl J Med 361:1349–1358
Shah P, Riphagen S, Beyene J, Perlman M (2004) Multiorgan dysfunction in infants with post-asphyxial hypoxic-ischaemic encephalopathy. Arch Dis Child Fetal Neonatal Ed 89:F152–F155
Kluckow M (2011) Functional echocardiography in assessment of the cardiovascular system in asphyxiated neonates. J Pediatr 158:e13–e18
More KS, Sakhuja P, Giesinger RE, Ting JY, Keyzers M, Sheth JN, Lapointe A, Jain A, Moore AM, Miller SP, McNamara PJ (2018) Cardiovascular associations with abnormal brain magnetic resonance imaging in neonates with hypoxic ischemic encephalopathy undergoing therapeutic hypothermia and rewarming. Am J Perinatol 35:979–989
Van Bel F, Walther FJ (1990) Myocardial dysfunction and cerebral blood flow velocity following birth asphyxia. Acta Paediatr Scand 79:756–762
Aggarwal S, Natarajan G (2017) Biventricular function on early echocardiograms in neonatal hypoxic-ischaemic encephalopathy. Acta Paediatr 106:1085–1090
Hochwald O, Jabr M, Osiovich H, Miller SP, McNamara PJ, Lavoie PM (2014) Preferential cephalic redistribution of left ventricular cardiac output during therapeutic hypothermia for perinatal hypoxic-ischemic encephalopathy. J Pediatr 164:999–1004
Nestaas E, Skranes JH, Støylen A, Brunvand L, Fugelseth D (2014) The myocardial function during and after whole-body therapeutic hypothermia for hypoxic-ischemic encephalopathy, a cohort study. Early Hum Dev 90:247–252
Lakshminrusimha S, Shankaran S, Laptook A, McDonald S, Keszler M, Van Meurs K, Guillet R, Chawla S, Sood BG, Bonifacio S, Das A, Higgins RD (2018) Pulmonary hypertension associated with hypoxic-ischemic encephalopathy-antecedent characteristics and comorbidities. J Pediatr 196:45–51.e3
Wu TW, Tamrazi B, Soleymani S, Seri I, Noori S (2018) Hemodynamic changes during rewarming phase of whole-body hypothermia therapy in neonates with hypoxic-ischemic encephalopathy. J Pediatr 197:68–74.e2
Giesinger RE, El Shahed AI, Castaldo MP, Breatnach CR, Chau V, Whyte HE, El-Khuffash A, Mertens L, McNamara PJ (2019) Impaired right ventricular performance is associated with adverse outcome following hypoxic ischemic encephalopathy. Am J Respir Crit Care Med 200:1294–1305. https://doi.org/10.1164/rccm.201903-0583OC
Liu J, Li J, Gu M (2007) The correlation between myocardial function and cerebral hemodynamics in term infants with hypoxic-ischemic encephalopathy. J Trop Pediatr 53:44–48
Greisen G (2014) Cerebral blood flow and oxygenation in infants after birth asphyxia. Clinically useful information? Early Hum Dev 90:703–705
Molicki J, Dekker I, de Groot Y, van Bel F (2000) Cerebral blood flow velocity wave form as an indicator of neonatal left ventricular heart function. Eur J Ultrasound 12:31–41
Mertens L, Seri I, Marek J, Arlettaz R, Barker P, McNamara P, Moon-Grady AJ, Coon PD, Noori S, Simpson J, Lai WW, Writing Group of the American Society of Echocardiography; European Association of Echocardiography (2011) Association for European Pediatric Cardiologists Targeted Neonatal Echocardiography in the Neonatal Intensive Care Unit: practice guidelines and recommendations for training. J Am Soc Echocardiogr 24:1057–1078
Naulaers G, Meyns B, Miserez M, Leunens V, Van Huffel S, Casaer P, Weindling M, Devlieger H (2007) Use of tissue oxygenation index and fractional tissue oxygen extraction as non-invasive parameters for cerebral oxygenation. A validation study in piglets. Neonatology 92:120–126
Kumagai T, Higuchi R, Higa A, Tsuno Y, Hiramatsu C, Sugimoto T, Booka M, Okutani T, Yoshikawa N (2013) Correlation between echocardiographic superior vena cava flow and short-term outcome in infants with asphyxia. Early Hum Dev 89:307–310
Tublin ME, Tessler FN, Murphy ME (1999) Correlation between renal vascular resistance, pulse pressure, and the resistive index in isolated perfused rabbit kidneys. Radiology. 213:258–264
Raju TN (1991) Cerebral Doppler studies in the fetus and newborn infant. J Pediatr 119:165–174
Guan B, Dai C, Zhang Y, Zhu L, He X, Wang N, Liu H (2017) Early diagnosis and outcome prediction of neonatal hypoxic-ischemic encephalopathy with color Doppler ultrasound. Diagn Interv Imaging 98:469–475
Wintermark P, Hansen A, Gregas MC, Soul J, Labrecque M, Robertson RL, Warfield SK (2011) Brain perfusion in asphyxiated newborns treated with therapeutic hypothermia. AJNR Am J Neuroradiol 32:2023–2029
Toet MC, Lemmers PM, van Schelven LJ, van Bel F (2006) Cerebral oxygenation and electrical activity after birth asphyxia: their relation to outcome. Pediatrics. 117(2):333–339
Zhou WJ, Yu F, Shi J, Yang H, Zou SJ, Jiang YM (2016) Serum levels of cardiac troponin I in asphyxiated neonates predict mortality. Clin Lab 62:1427–1434
Karaarslan S, Alp H, Baysal T, Çimen D, Örs R, Oran B (2012) Is myocardial performance index useful in differential diagnosis of moderate and severe hypoxic-ischaemic encephalopathy? A serial Doppler echocardiographic evaluation. Cardiol Young 22:335–340
Jain A, Mohamed A, Kavanagh B, Shah PS, Kuipers BCW, El-Khuffash A, Mertens L, Jankov RP, McNamara PJ (2018) Cardiopulmonary adaptation during first day of life in human neonates. J Pediatr 200:50–7.e2
Levy PT, El Khuffash A, Woo KV, Hauck A, Hamvas A, Singh GK (2019) A novel noninvasive index to characterize right ventricle pulmonary arterial vascular coupling in children. JACC Cardiovasc Imaging 12(4):761–763
Author information
Authors and Affiliations
Contributions
Study design: LA and MJR. Acquisition of data: MJR, AC, and LA. Data analysis: JMO. Interpretation of data: MJR, AC, JMO, and LA. Manuscript drafting: LA. All the authors critically reviewed the draft and gave their approval to the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the local Ethics Committee.
Informed consent
An exemption of formal consent was obtained for the inclusion of retrospective data. Parental informed consent was obtained before enrollment of control patients.
Additional information
Communicated by Daniele De Luca,
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 13 kb).
Rights and permissions
About this article
Cite this article
Rodriguez, M.J., Corredera, A., Martinez-Orgado, J. et al. Cerebral blood flow velocity and oxygenation correlate predominantly with right ventricular function in cooled neonates with moderate-severe hypoxic-ischemic encephalopathy. Eur J Pediatr 179, 1609–1618 (2020). https://doi.org/10.1007/s00431-020-03657-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-020-03657-w