Abstract
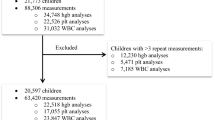
The aim of this study was to evaluate to which extend adult reference intervals (RIs) could be applied in children. A local paediatric population (aged 1 to < 20 years), based on first draw samples from general practitioners (GPs), was established. Children with samples taken at a hospital or > 3 samples from GPs were excluded. Analytes evaluated included haematological, liver and pancreatic function, kidney function, electrolytes, and metabolism parameters. Applicability of adult RIs in children aged 1–17 years was evaluated using individuals aged 18–19 years as reference groups for the adult RIs. The local population consisted of 31,024 children with 282,721 analyses in total. For each analyte, 17 age strata and two gender strata were established. Partitioning was not warranted in 51% of the male strata and in 69% of the female strata. Adult RIs could be applied in 42% for children aged 1–< 10 years, 57% for children aged 10–< 15 years, and 85% for children aged 15–<18 years.
Conclusion: for certain analytes, there is no need to partition between adult and paediatric RIs, but a need for age- and gender-specific RIs remains for several clinical laboratory tests.
What is Known: • Establishing paediatric reference intervals (RIs) is time consuming, costly, and not feasible for many laboratories. Transference of RIs established elsewhere often leads to misclassification of paediatric laboratory results. • Adult RIs are often more easily established and validated. | |
What is New: • Adult RIs can be applied to children as young as 2 years for some analytes. Conversely, for some analytes, adult RIs cannot be applied in children aged 1–17 years. • Laboratory data can be applied in evaluating the need for partitioning in reference intervals. |

Similar content being viewed by others
Abbreviations
- Alb:
-
Albumin
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine transaminase
- AMY:
-
Amylase
- AMYP:
-
Amylase, pancreatic
- AST:
-
Aspartate transaminase
- Bil, conj:
-
Bilirubin, conjugated
- BUN:
-
Blood urea nitrogen
- Ca:
-
Calcium
- CHOL:
-
Cholesterol
- CK:
-
Creatine kinase
- CLSI:
-
Clinical and Laboratory Standards Institute
- Cr:
-
Creatinine
- Erc:
-
Erythrocytes
- EVF:
-
Erythrocyte volume fraction
- F:
-
Female
- Fe:
-
Iron
- Glu:
-
Glucose
- GGT:
-
γ-Glutamyl transferase
- GP:
-
General practitioner
- HDL:
-
High-density lipoprotein
- Hgb:
-
Haemoglobin
- K:
-
Potassium
- LDH:
-
Lactate dehydrogenase
- LDL:
-
Low-density lipoprotein
- LH:
-
Lillebaelt Hospital
- Lkc:
-
Leukocytes
- M:
-
Male
- MCH:
-
Mean corpuscular haemoglobin
- MCHC:
-
Mean corpuscular haemoglobin concentration
- MCV:
-
Mean corpuscular volume
- Mg:
-
Magnesium
- Na:
-
Sodium
- OUH:
-
Odense University Hospital
- P:
-
Phosphate
- PLT:
-
Platelets
- RI:
-
Reference interval
- SI:
-
System of units
- SD:
-
Standard deviation
- TGL:
-
Triglyceride
- TP:
-
Total protein
- UA:
-
Uric acid
References
AACC. AACC calls on congress to fund CDC effort to improve pediatric medical testing: AACC.org; 2019 [Available from: https://www.aacc.org/media/press-release-archive/2019/03-mar/aacc-calls-on-congress-to-fund-cdc-effort-to-improve-pediatric-medical-testing
(CLSI) CaLSI. Defining, establishing, and verifying reference intervals in the clinical laboratory; approved guideline 2010
Tahmasebi H, Higgins V, Fung AWS, Truong D, White-Al Habeeb NMA, Adeli K (2017) Pediatric reference intervals for biochemical markers: gaps and challenges, recent national initiatives and future perspectives. EJIFCC. 28(1):43–63
Alnor AB, Vinholt PJ (2019) Paediatric reference intervals are heterogeneous and differ considerably in the classification of healthy paediatric blood samples. Eur J Pediatr
Rustad P, Felding P, Franzson L, Kairisto V, Lahti A, Martensson A et al (2004) The Nordic Reference Interval Project 2000: recommended reference intervals for 25 common biochemical properties. Scand J Clin Lab Invest 64(4):271–284
Nordin G, Martensson A, Swolin B, Sandberg S, Christensen NJ, Thorsteinsson V et al (2004) A multicentre study of reference intervals for haemoglobin, basic blood cell counts and erythrocyte indices in the adult population of the Nordic countries. Scand J Clin Lab Invest 64(4):385–398
Tukey JW (1977) Exploratory data analysis. Addison-Wesley, Reading
Harris EK, Wong ET, Shaw ST Jr (1991) Statistical criteria for separate reference intervals: race and gender groups in creatine kinase. Clin Chem 37(9):1580–1582
Harris EK, Boyd JC (1990) On dividing reference data into subgroups to produce separate reference ranges. Clin Chem 36(2):265–270
Adeli K, Higgins V, Trajcevski K, White-Al HN (2017) The Canadian laboratory initiative on pediatric reference intervals: a CALIPER white paper. Crit Rev Clin Lab Sci 54(6):358–413
Colantonio DA, Kyriakopoulou L, Chan MK, Daly CH, Brinc D, Venner AA, Pasic MD, Armbruster D, Adeli K (2012) Closing the gaps in pediatric laboratory reference intervals: a CALIPER database of 40 biochemical markers in a healthy and multiethnic population of children. Clin Chem 58(5):854–868
Aarsand AK, Diaz-Garzon J, Fernandez-Calle P, Guerra E, Locatelli M, Bartlett WA et al (2018) The EuBIVAS: within- and between-subject biological variation data for electrolytes, lipids, urea, uric acid, total protein, total bilirubin, direct bilirubin, and glucose. Clin Chem 64(9):1380–1393
Dortschy R, Rosario AS, Scheidt-Nave C, Thierfelder W, Thamm M, Gutsche J, et al. (2009) Bevölkerungsbezogene Verteilungswerte ausgewählter Laborparameter aus der Studie zur Gesundheit von Kindern und Jugendlichen in Deutschland (KiGGS). In: Robert-Koch I, editor. Berlin
Adeli K, Raizman JE, Chen Y, Higgins V, Nieuwesteeg M, Abdelhaleem M et al (2015) Complex biological profile of hematologic markers across pediatric, adult, and geriatric ages: establishment of robust pediatric and adult reference intervals on the basis of the Canadian Health Measures Survey. Clin Chem 61(8):1075–1086
Rosenfeld RG, Nicodemus BC (2003) The transition from adolescence to adult life: physiology of the ‘transition’ phase and its evolutionary basis. Horm Res 60(Suppl 1):74–77
Palmert MR, Boepple PA (2001) Variation in the timing of puberty: clinical spectrum and genetic investigation. J Clin Endocrinol Metab 86(6):2364–2368
Harris EK, Boyd JC (1995) Statistical bases of reference values in laboratory medicine. Marcel Dekker, New York
Lahti A, Hyltoft Petersen P, Boyd JC, Fraser CG, Jorgensen N (2002) Objective criteria for partitioning Gaussian-distributed reference values into subgroups. Clin Chem 48(2):338–352
Horn PS, Pesce AJ, Copeland BE (1998) A robust approach to reference interval estimation and evaluation. Clin Chem 44(3):622–631
Koerbin G, Potter JM, Andriolo K, West NP, Glasgow N, Hawkins C, Cavanaugh JA, Hickman PE (2017) ‘Aussie Normals’: an a priori study to develop reference intervals in a healthy Australian population using the Beckman Coulter LH 750 Haematology Analyser as candidates for harmonised values. Pathology. 49(5):518–525
Lahti A (2004) Are the common reference intervals truly common? Case studies on stratifying biochemical reference data by countries using two partitioning methods. Scand J Clin Lab Invest 64(4):407–430
Lahti A, Petersen PH, Boyd JC, Rustad P, Laake P, Solberg HE (2004) Partitioning of nonGaussian-distributed biochemical reference data into subgroups. Clin Chem 50(5):891–900
Lykkeboe S, Nielsen CG, Christensen PA (2018) Indirect method for validating transference of reference intervals. Clin Chem Lab Med 56(3):463–470
Zierk J, Arzideh F, Rechenauer T, Haeckel R, Rascher W, Metzler M, Rauh M (2015) Age- and sex-specific dynamics in 22 hematologic and biochemical analytes from birth to adolescence. Clin Chem 61(7):964–973
Zierk J, Arzideh F, Haeckel R, Rascher W, Rauh M, Metzler M (2013) Indirect determination of pediatric blood count reference intervals. Clin Chem Lab Med 51(4):863–872
Author information
Authors and Affiliations
Contributions
Anne Bryde Alnor and Pernille Just Vinholt contributed equally to the present study.
The authors contributed equally to the present study.
Corresponding author
Ethics declarations
This article does not contain any studies with human participant or animals performed by any of the authors. The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 72 kb)
Rights and permissions
About this article
Cite this article
Alnor, A.B., Vinholt, P.J. Application of adult reference intervals in children. Eur J Pediatr 179, 483–491 (2020). https://doi.org/10.1007/s00431-019-03527-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03527-0