Abstract
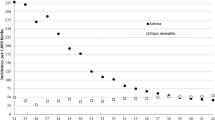
Little is known about respiratory morbidity and asthma risk in preterm infants (PTIs) with a gestational age (GA) over 32 weeks. This was a prospective study carried out from birth to 7–8 years, comparing two groups: (a) PTIs (GAs 32 weeks + 1 day to 35 weeks + 0 days, without comorbidities) and (b) full-term infants (FTIs; GA ≥ 37 weeks). Risk and protective factors for bronchiolitis and asthma were identified. A total of 232 children (116/group) were included. Sixty-six (56.9%) PTIs and 43 (37.1%) FTIs presented bronchiolitis (p = 0.002). Recurrent wheezing was 52 (44.8%) on PTIs versus 36 (31.0%) on FTIs (p = 0.03). Asthma at school aged was 27 (23.3%) on PTIs and 8 (6.9%) on FTIs (p = 0.020). Asthma risk factors were only detected in group A.
Conclusion: PTIs had a higher prevalence of bronchiolitis, recurrent wheezing and asthma; risk factors for asthma are the following: older siblings, allergic father, atopic dermatitis and antibiotic treatment in the first 3 years of life and prematurity itself, which also acted as protective factor for atopic dermatitis.
What is known: • In recent decades, there has been a significant increase in the birth of premature babies and consequently, also in the pathologies secondary to the prematurity: a greater number of complications and disorders related to the development and maturation of many organs and systems, especially the respiratory system. Several studies, especially in full-term infants and very preterm infants, have tried to elucidate the risk factors that may influence the development of persistent or chronic respiratory problems such asasthma, but little is known about the aetiology of these disorders in the late or moderate preterm infants. Inthis group of children, the role played by certain factors (early use of antibiotics, chorioamnionitis, smokeexposure, paternal asthma, etc.) on late respiratory morbidity, or asthma, is inconclusive. • Moderate-to-late preterm infants are more predisposed to developing recurrent wheezing/asthma and should adopt control measures. | |
What is new: • Our work provides data related to little-understood aspects of respiratory diseases in this group of late or moderate preterm infants (gestational age between 32 weeks plus 1 day and 35 weeks plus 0 days), by monitoring their evolution from birth to 7–8 years of age, compared with another group of full-term newborns. We aimed to establish the prevalence of bronchiolitis and recurrent wheezing in these children during their first years of life. • The prevalence of school-aged asthma and the risk factors for contracting it were also investigated. |

Similar content being viewed by others
Abbreviations
- BDT:
-
Bronchodilator test
- BMI:
-
Body mass index
- CIs:
-
Confidence intervals
- FeNO:
-
Fractional exhaled nitric oxide
- FEV1 :
-
Forced expiratory volume in the first second
- FVC:
-
Forced vital capacity
- FEV1/FVC:
-
Tiffeneau–Pinelli index
- FTIs:
-
Full-term infants
- GINA:
-
Global Initiative for Asthma
- GA:
-
Gestational age
- ISAAC:
-
International Study of Asthma and Allergies in childhood
- IgE:
-
Immunoglobulin E
- IVF:
-
In vitro fecundation
- mAPI:
-
Modified asthma predictive index
- MEF25–75:
-
Maximal expiratory flow rate at 25–75% of forced vital capacity
- N :
-
Number of responses
- NBs:
-
Newborns
- OR:
-
Odds ratio
- ppb:
-
Parts per billion
- PTIs:
-
Preterm infants
- RSV:
-
Respiratory syncytial virus
- SD:
-
Standard deviation
- TAPQOL:
-
Preschool Children’s Quality of Life Questionnaire
References
Beck S, Wojdyla D, Say L et al (2010) Incidencia mundial de parto prematuro: revisión sistemática de la morbilidad y mortalidad maternas. Bull 31 World Health Organ 88:31–38
Colin AA, Mc Evoy C, Castile RG (2010) Respiratory morbidity and lung function in preterm infants of 32 to 36 weeks gestational age. Pediatrics 126(1):115–128
Been JV, Lugtenberg MJ, Smets E, van Schayck CP, Kramer BW, Mommers M, Sheikh A (2014) Preterm birth and childhood wheezing disorders: a systematic review and meta-analysis. PLoS Med 11(1):e1001596
Paul IM, Camera L, Zeiger RS, Guilbert TW, Bacharier LB, Taussig LM, Morgan WJ, Covar RA, Krawiec M, Bloomberg GR, Mauger DT, for the Childhood Asthma Research and Education (CARE) Network (2010) Childhood Asthma Research and Education (CARE) Network. Relationship between infant weight gain and later asthma. Pediatr Allergy Immunol 21(1 Pt 1):82–89
Pike KC, Crozier SR, Lucas JS et al (2010) Patterns of fetal and infant growth are related to atopy and wheezing disorders at age 3 years. Thorax 65(12):1099–1106
Kindlund K, Thomsen SF, Stensballe LG, Skytthe A, Kyvik KO, Backer V, Bisgaard H (2010) Birth weight and risk of asthma in 3-9-year-old twins: exploring the fetal origins hypothesis. Thorax 65(2):146–149
Sonnenschein-van der Voort AM, Jaddoe VW, Raat H et al (2012) Fetal and infant growth and asthma symptoms in preschool children: the Generation R Study. Am J Respir Crit Care Med 85(7):731–737
Rzehak P, Wijga AH, Keil T, Eller E, Bindslev-Jensen C, Smit HA, Weyler J, Dom S, Sunyer J, Mendez M, Torrent M, Vall O, Bauer CP, Berdel D, Schaaf B, Chen CM, Bergström A, Fantini MP, Mommers M, Wahn U, Lau S, Heinrich J (2013) Body mass index trajectory classes and incident asthma in childhood: results from 8 European birth cohorts—a Global Allergy and Asthma European Network initiative. J Allergy Clin Immunol 131(6):1528–1536
Bacharier LB (2014) Early-life weight gain, prematurity, and asthma development. J Allergy Clin Immunol 133(5):1330–1331
Sonnenschein-van der Voort AM, Arends LR, de Jongste JC et al (2014) Preterm birth, infant weight gain, and childhood asthma risk: a meta-analysis of 147,000 European children. J Allergy Clin Immunol 133(5):1317–1329
Harju M, Keski-Nisula L, Georgiadis L et al (2014) The burden of childhood asthma and late preterm and early term births. J Pediatr 164(2):295–299.e1
Liu X, Olsen J, Agerbo E, Yuan W, Cnattingius S, Gissler M, Li J (2014) Birth eight, gestational age, fetal growth and childhood asthma hospitalization. Allergy Asthma Clin Immunol 10(1):13
Kwinta P, Pietrzyk JJ (2010) Preterm birth and respiratory disease in later life. Expert Rev Respir Med 4(5):593–604
Wise J (2014) Smoking bans are linked to reduction in preterm births and childhood asthma, says study. BMJ 348:g2414
Aspberg S, Dahlquist G, Kahan T, Källén B (2010) Confirmed association between neonatal phototherapy or neonatal icterus and risk of childhood asthma. Pediatr Allergy Immunol 21(4 Pt 2):e733–e739
Khalkhali HR, Oshnouei S, Salarilak S, Rad MR, Karamyar M, Khashabi J (2014) Effects of antibiotic consumption on children 2-8 years of age developing asthma. Epidemiol Health 36:e2014006
García P, San Feliciano L, Benito F, García R, Guzmán J, Salas S, Fernández C, del Prado N, Ciprián D, Figueras J, hospitales pertenecientes a SEN1500 (2013) Evolución a los 2 años de una cohorte de RN con peso <=1500 g de los hospitales pertenecientes a la red neonatal SEN 1500. An Pediatr (Barc) 79(5):279–287
Costeloe KL, Hennessy EM, Haider S, Stacey F, Marlow N, Draper ES (2012) Short term outcomes after extreme preterm birth in England: comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). BMJ 345:e7976
Álvarez Mingorance P, Burón Martínez E, Blanco QA (2011) Morbilidad de los niños prematuros en edad escolar (II): patología respiratoria, alteraciones del crecimiento y presión arterial. Acta Pediatr Esp 69(9):379–384
Pérez-Yarza EG, Moreno-Galdó A, Ramilo O, Rubí T, Escribano A, Torres A, Sardón O, Oliva C, Pérez G, Cortell I, Rovira-Amigo S, Pastor-Vivero MD, Pérez-Frías J, Velasco V, Torres-Borrego J, Figuerola J, Barrio MI, García-Hernández G, Mejías A, the SAREPREM 3235 investigators (2015) Risk factors for bronchiolitis, recurrent wheezing and related hospitalization in preterm infants during the first year of life. Pediatr Allergy Immunol 26(8):797–804. https://doi.org/10.1111/pai.12414
Pike KC, Lucas JS (2015) Respiratory consequences of late preterm birth. Paediatr Respir Rev 16(3):182–188
Voge GA, Katusic SK, Qin R, Juhn YJ (2015) Risk of asthma in late preterm infants: a propensity score approach. J Allergy Clin Immunol Pract 3(6):905–910. https://doi.org/10.1016/j.jaip.2015.03.018
Sardón Prado O, Morera G, Herdman M, Moreno Galdó A, Pérez-Yarza EG, Detmar S, Fekkes M, Rajmil L (2008) Versión española del TAPQOL: calidad de vida relacionada con la salud en niños de 3 meses a 5 años. An Pediatr 68(5):420–424
Mata Fernández C, Fernández-Benitez M, Pérez Miranda M et al (2005) Validation of the Spanish version of the phase III ISAAC questionnaire on asthma. J Investig Allergol Clin Immunol 15(3):201–210
GINA (2015) Global strategy for asthma management and prevention. Available from: http://www.ginasthma.org/. Accessed Dec 2015
Álvarez Caro F, Pérez Guirado A (2010) Ruíz del Árbol Sánchez P, et al. Óxido nítrico exhalado en el asma infantil. Arch Argent Pediatr 108(6):544–551
Jenkins MA, Clarke JR, Carlin JB et al (1996) Validation of questionnaire and bronchial hyperresponsiveness against respiratory physician assessment in the diagnosis of asthma. Int J Epidemiol 25:609–616
GEMA4.0 Guía Española para el Manejo del Asma (2015) www.gemasma.com. Accessed Dec 2015
Figueras Aloy J, Carbonell Estrany X, Comité de Estándares de la SENeo (2015) Actualización de las recomendaciones de la Sociedad Española de Neonatología para la utilización del palivizumab como profilaxis de las infecciones graves por el virus respiratorio sincitial. An Pediatr (Barc) 82(3):199.e1–2
Odibo IN, Bird TM, McKelvey SS et al (2016 Jan) Childhood respiratory morbidity after late preterm and early term delivery: a study of Medicaid patients in South Carolina. Paediatr Perinat Epidemiol 30(1):67–75
Brandão HV, Vieira GO, Vieira TO et al (2017) Acute viral bronchiolitis and risk of asthma in schoolchildren: analysis of a Brazilian newborn cohort. J Pediatr 93:223–229
GonÇalves C, Wandalsen G, Lanza F et al (2016) Repercussions of preterm birth on symptoms of asthma, allergic diseases and pulmonary function, 6–14 years later. Allergol Immunopathol 44(6):489–496
Chang TS, Lemanske RF, Guilbert TW et al (2013) Evaluation of the modified asthma predictive index in high risk preschool children. J Allergy Clin Immunol Pract 1(2):152–156
Kotecha SJ, Watkins WJ, Paranjothy S, Dunstan FD, Henderson AJ, Kotecha S (2012) Effect of late preterm birth on longitudinal lung spirometry in school age children and adolescents. Thorax 67(1):54–61
Leung JY, Lam HS, Leung GM et al (2016 Mar) Gestational age, birthweight for gestational age, and childhood hospitalisations for asthma and other wheezing disorders. Paediatr Perinat Epidemiol 30(2):149–159
İlkay E, Günlemez A, Uyan ZS et al (2017) Evaluation of pulmonary functions in preschool children born late-preterm. Turk Pediatri Ars 52:72–78
Leps C, Carson C, Quigley MA (2018) Gestational age at birth and wheezing trajectories at 3-11 years. Arch Dis Child 103(12):1138–1144
Kaczmarczyk K, Wiszomirska I, Szturmowicz M, Magiera A, Błażkiewicz M (2017 Jul) Are preterm-born survivors at risk of long-term respiratory disease? Ther Adv Respir Dis 11(7):277–287
Asher M, Montefort S, Bjorksten B et al (2006) Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet 368(9537):733–743
Kusel MM, de Klerk NH, Kebadze T et al (2007) Early life respiratory viral infections, atopic sensitization, and risk of subsequent development of persistent asthma. J Allergy Clin Immunol 119(5):1105–1110
Kusel MMH, Kebadze T, Johnston SL, Holt PG, Sly PD (2012) Febrile respiratory illnesses in infancy and atopy are risk factors for persistent asthma and wheeze. Eur Respir J 39(4):876–882
Von Kobyletzki L, Bornehag CG, Hasselgren M et al (2012) Eczema in early childhood is strongly associated with the development of asthma and rhinitis in a prospective cohort. BMC Dermatol 12:11
Saunes M, Oien T, Dotterud CK et al (2012) Early eczema and risk of childhood asthma: a prospective, population-based study. BMC Pediatr 12:168
Rosas-Salazar C, Ramratnam SK, Brehm JM, Han YY, Boutaoui N, Forno E, Acosta-Pérez E, Alvarez M, Colón-Semidey A, Canino G, Celedón JC (2014) Prematurity, atopy, and childhood asthma in Puerto Ricans. J Allergy Clin Immunol 133(2):357–362
Miyake Y, Tanaka K (2013) Lack of relationship between birth conditions and allergic disorders in Japanese children aged 3 years. J Asthma 50(6):555–559
Gaffin JM, Kanchongkittiphon W, Phipatanakul W (2014) Perinatal and early childhood environmental factors influencing allergic asthma immunopathogenesis. Int Immunopharmacol 23:337–346
van der Gugten AC, Koopman M, Evelein AM et al (2012) Rapid early weight gain is associated with wheeze and reduced lung function in childhood. Eur Respir J 39(2):403–410
Acknowledgements
The authors would like to acknowledge the collaboration of the neonatal service and the paediatric nursing staff at the Hospital Clínico de Valencia. The authors acknowledge the collaboration of Alce Ingeniería (Las Rozas, Madrid, Spain) in the initial development of the project support systems and statistical analysis.
Author information
Authors and Affiliations
Contributions
J M-A, MD, and A E-M, MD: conceived and designed the study, drafted the initial manuscript and approved the final manuscript as submitted.
T R-R, MD, and S C-C, MD: carried out the initial analyses, reviewed and revised the manuscript and approved the final manuscript as submitted.
All the authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Ethics declarations
The period between birth and 3 years of age was already collected in our centre (Infantile Pneumology and Cystic Fibrosis Unit of the Hospital Clínico Universitario Valencia), as part of a national multicentre study (SAREPREM 3235) in which we participated as researchers, and which was approved by the Ethics and Clinical Research Committee of the Donostia Hospital, in San Sebastián, and was carried out under the ethical postulates of the Helsinki Declaration and the guidelines of the Spanish Society of Paediatric Pneumology (SENP).
After its completion, it was proposed to extend it with the follow-up of the children included in our centre until the age of 6–8 years, and was approved by the Ethics Committee of the Hospital Clínico Universitario de Valencia.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
All parents signed the written informed consent.
Additional information
Communicated by Peter de Winter
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Morata-Alba, J., Romero-Rubio, M.T., Castillo-Corullón, S. et al. Respiratory morbidity, atopy and asthma at school age in preterm infants aged 32–35 weeks. Eur J Pediatr 178, 973–982 (2019). https://doi.org/10.1007/s00431-019-03372-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03372-1