Abstract
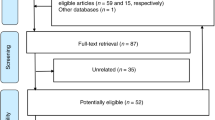
Monitoring leptin concentration in maternal blood would be useful for earlier identification of mothers at risk of delivering small for gestational age (SGA) neonates. This study was performed to examine whether maternal blood leptin concentrations are different between SGA neonates and healthy controls. Meta-analysis was performed to summarize the data of all English-language studies providing the numbers of SGA neonates, the numbers of healthy controls, and the means and standard deviations of maternal blood leptin concentrations in these two groups. The studies were collected by searching ten databases including PubMed (MEDLINE) and investigating the PubMed Related Citations and bibliographic references. The Newcastle–Ottawa Scale was used to assess study quality. Publication bias was assessed using Egger’s test. The primary outcome of this study was the standardized mean difference (SMD) in maternal blood leptin concentration between SGA neonates and healthy controls. Thirty-two overall good-quality studies involving 1734 women and their neonates were extracted from 17 articles. Synthetic evidence did not indicate statistically significant SMD in maternal blood leptin concentration between SGA neonates and healthy controls (P = 0.172). Egger’s test showed no publication bias (P = 0.309).
Conclusion: Maternal blood leptin concentration is not significantly different between SGA neonates and healthy controls.
What is Known: • Monitoring leptin concentration in maternal blood would be useful for earlier identification of mothers at risk of delivering small for gestational age (SGA) neonates. | |
What is New: • The results of this meta-analysis including 1734 women and their neonates in 32 overall good-quality studies showed that maternal blood leptin concentration is not significantly different between SGA neonates and healthy controls. |

Similar content being viewed by others
Abbreviations
- CM:
-
Congenital malformations
- ELISA:
-
Enzyme-linked immunosorbent assay
- IRMA:
-
Immunoradiometric assay
- IUGR:
-
Intrauterine growth restriction
- NOS:
-
Newcastle–Ottawa Scale
- PE:
-
Preeclampsia
- RIA:
-
Radioimmunoassay
- SD:
-
Standard deviation
- SGA:
-
Small for gestational age
- SMD:
-
Standardized mean difference
References
Arslan M, Yazici G, Erdem A, Erdem M, Arslan EO, Himmetoglu O (2004) Endothelin 1 and leptin in the pathophysiology of intrauterine growth restriction. Int J Gynaecol Obstet 84:120–126
Aydin Hİ, Demirkaya E, Karadeniz RS, Olgun A, Alpay F (2014) Assessing leptin and soluble leptin receptor levels in full-term asymmetric small for gestational age and healthy neonates. Turk J Pediatr 56:250–258
Aydin HI, Eser A, Kaygusuz I, Yildirim S, Celik T, Gunduz S, Kalman S (2016) Adipokine, adropin and endothelin-1 levels in intrauterine growth restricted neonates and their mothers. J Perinat Med 44:669–676
Briffa JF, McAinch AJ, Romano T, Wlodek ME, Hryciw DH (2015) Leptin in pregnancy and development: a contributor to adulthood disease? Am J Physiol Endocrinol Metab 308:E335–E350
Catov JM, Patrick TE, Powers RW, Ness RB, Harger G, Roberts JM (2007) Maternal leptin across pregnancy in women with small-for-gestational-age infants. Am J Obstet Gynecol 196:558.e1–558.e8
Deeks JJ, Higgins JPT, Altman DG (2011) 9.2.3.2 The standardized mean difference. In: Higgins JPT, Green S (eds) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. http://handbook.cochrane.org/chapter_9/9_2_3_2_the_standardized_mean_difference.htm. Accessed 13 February 2019
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Egger M, Smith GD, Altman DG (2001) Systematic reviews in healthcare: meta-analysis in context, 2nd edn. BMJ, London
Ferrero S, Mazarico E, Valls C, Di Gregorio S, Montejo R, Ibáñez L, Gomez-Roig MD (2015) Relationship between foetal growth restriction and maternal nutrition status measured by dual-energy x-ray absorptiometry, leptin, and insulin-like growth factor. Gynecol Obstet Investig 80:54–59
Fu R, Vandermeer BW, Shamliyan TA, O’Neil ME, Yazdi F, Fox SH, Morton SC (2008) Handling continuous outcomes in quantitative synthesis. In: Kronick R, Slutsky JR, Chang S (eds) Methods guide for effectiveness and comparative effectiveness reviews [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK154408/. Accessed 13 February 2019
Giapros V, Drougia A, Krallis N, Theocharis P, Andronikou S (2012) Morbidity and mortality patterns in small-for-gestational age infants born preterm. J Matern Fetal Neonatal Med 25:153–157
Grisaru-Granovsky S, Eitan R, Algur N, Schimmel MS, Diamant YZ, Samueloff A (2003) Maternal and umbilical cord serum leptin concentrations in small-for-gestational-age and in appropriate-for-gestational-age neonates: a maternal, fetal, or placental contribution? Biol Neonate 84:67–72
Jenkins LD, Powers RW, Adotey M, Gallaher MJ, Markovic N, Ness RB, Roberts JM (2007) Maternal leptin concentrations are similar in African Americans and Caucasians in normal pregnancy, preeclampsia and small-for-gestational-age infants. Hypertens Pregnancy 26:101–109
Kingdom JC, Kaufmann P (1997) Oxygen and placental villous development: origins of fetal hypoxia. Placenta 18:613–621
Kingdom JC, Kaufmann P (1999) Oxygen and placental vascular development. Adv Exp Med Biol 474:259–275
Kyriakakou M, Malamitsi-Puchner A, Militsi H, Boutsikou T, Margeli A, Hassiakos D, Kanaka-Gantenbein C, Papassotiriou I, Mastorakos G (2008) Leptin and adiponectin concentrations in intrauterine growth restricted and appropriate for gestational age fetuses, neonates, and their mothers. Eur J Endocrinol 158:343–348
Laivuori H, Gallaher MJ, Collura L, Crombleholme WR, Markovic N, Rajakumar A, Hubel CA, Roberts JM, Powers RW (2006) Relationships between maternal plasma leptin, placental leptin mRNA and protein in normal pregnancy, pre-eclampsia and intrauterine growth restriction without pre-eclampsia. Mol Hum Reprod 12:551–556
Lepercq J, Guerre-Millo M, André J, Caüzac M, Hauguel-de Mouzon S (2003) Leptin: a potential marker of placental insufficiency. Gynecol Obstet Investig 55:151–155
Mise H, Yura S, Itoh H, Nuamah MA, Takemura M, Sagawa N, Fujii S (2007) The relationship between maternal plasma leptin levels and fetal growth restriction. Endocr J 54:945–951
Mouzaki A, Panagoulias I, Raptis G, Farri-Kostopoulou E (2010) Cord blood leptin levels of healthy neonates are associated with IFN-γ production by cord blood T-cells. PLoS One 7:e40830
Nezar MA, el-Baky AM, Soliman OA, Abdel-Hady HA, Hammad AM, Al-Haggar MS (2009) Endothelin-1 and leptin as markers of intrauterine growth restriction. Indian J Pediatr 76:485–488
Orbak Z, Darcan S, Coker M, Gökşen D (2001) Maternal and fetal serum insulin-like growth factor-I (IGF-I) IGF binding protein-3 (IGFBP-3), leptin levels and early postnatal growth in infants born asymmetrically small for gestational age. J Pediatr Endocrinol Metab 14:1119–1127
Pérez-Pérez A, Toro A, Vilariño-García T, Maymó J, Guadix P, Dueñas JL et al (2018) Leptin action in normal and pathological pregnancies. J Cell Mol Med 22:716–727
Ren RX, Shen Y (2010) A meta-analysis of relationship between birth weight and cord blood leptin levels in newborns. World J Pediatr 6:311–316
Romero R (1996) The child is the father of the man. Prenat Neonatal Med 1:8–11
Savvidou MD, Sotiriadis A, Kaihura C, Nicolaides KH, Sattar N (2008) Circulating levels of adiponectin and leptin at 23-25 weeks of pregnancy in women with impaired placentation and in those with established fetal growth restriction. Clin Sci (Lond) 115:219–224
Señarís R, Garcia-Caballero T, Casabiell X, Gallego R, Castro R, Considine RV, Dieguez C, Casanueva FF (1997) Synthesis of leptin in human placenta. Endocrinology 138:4501–4504
Sharma P, McKay K, Rosenkrantz TS, Hussain N (2004) Comparisons of mortality and pre-discharge respiratory outcomes in small-for-gestational-age and appropriate-for-gestational-age premature infants. BMC Pediatr 4:9
Steichen TJ (1998) Tests for publication bias in meta-analysis. Stata Tech Bull 41:9–15
Tamura T, Goldenberg RL, Johnston KE, Cliver SP (1998) Serum leptin concentrations during pregnancy and their relationship to fetal growth. Obstet Gynecol 91:389–395
Tsai LY, Chen YL, Tsou KI, Mu SC, Taiwan Premature Infant Developmental Collaborative Study Group (2015) The impact of small-for-gestational-age on neonatal outcome among very-low-birth-weight infants. Pediatr Neonatol 56:101–107
Wells GA, Shea B, O’Connel D, Peterson J, Welch V, Losos M, Tugwell P (2014) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 13 February 2019
Yildiz L, Avci B, Ingeç M (2002) Umbilical cord and maternal blood leptin concentrations in intrauterine growth retardation. Clin Chem Lab Med 40:1114–1117
Zareaan E, Heidarpour M, Kargarzadeh E, Moshfeghi M (2017) Association of maternal and umbilical cord blood leptin concentrations and abnormal color Doppler indices of umbilical artery with fetal growth restriction. Int J Reprod Biomed (Yazd) 15:135–140
Acknowledgements
The author is grateful to the staff of the Medical Library, the Japan Medical Association (Tokyo, Japan), for help in retrieving the full texts of the articles included in the analysis.
Author information
Authors and Affiliations
Contributions
EG, the corresponding author, is responsible for literature search, figures, study design, data collection, data analysis, data interpretation, and writing.
Corresponding author
Ethics declarations
Conflict of interest
The author declares that he has no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by the author.
Informed consent
Not required.
Additional information
Communicated by Patrick Van Reempts
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 47 kb)
Rights and permissions
About this article
Cite this article
Goto, E. Maternal blood leptin concentration in small for gestational age: a meta-analysis. Eur J Pediatr 178, 763–770 (2019). https://doi.org/10.1007/s00431-019-03351-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03351-6