Abstract
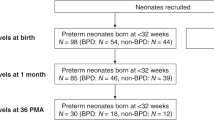
Bronchopulmonary dysplasia (BPD) is a severe complication of prematurity that impacts survival and neurodevelopment. Currently, no early marker exists which could help clinicians identify which preterm infants will develop BPD. Given the evidence that NTproBNP is elevated in children with BPD, we hypothesized that it could be used as an early marker of BPD development. We conducted a prospective cohort study including very low birth weight infants (VLBWI) admitted to our NICU between January 2015 and January 2017 in which we determined serial NTproBNP levels on days 1 and 3 and then weekly, until 49 days of life. A total of 101 patients were recruited (mean birth weight 1152 g (SD 247.5), mean gestational age 28.9 weeks (SD 1.9)). NTproBNP levels differed among infants who did and did not develop BPD from 14 to 35 days of life with the greatest difference on day 14 of life (non-BPD group (n = 86): 1155 (IQR 852–1908) pg/mL, BPD (n = 15): 9707 (IQR 3212–29,560) pg/mL; p = 0.0003). The presence of HsPDA did not account for higher levels of NTproBNP at day 14 (p = 0.165). We calculated an optimal cutoff point of 2264 pg/mL at 14 days of life (sensitivity 100%, specificity 86% and AUC 0.93).
Conclusions: NTproBNP at 14 days of life could be used as an early marker of later BPD development in VLBWI.
What is Known: • Children with BPD have elevated NTproBNP levels, which are related to the severity of BPD and the development of pulmonary hypertension. | |
What is New: • NTproBNP at 14 days of life is higher in those who later develop BPD, regardless of the presence of hemodynamically significant patent ductus arteriosus. • A calculated cutoff point of 2264 pg/mL of NTproBNP at 14 days has a sensitivity of 100% and specificity of 86% in the prediction of BPD. |



Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- BNP:
-
Brain natriuretic peptide
- BPD:
-
Bronchopulmonary dysplasia
- CRIB:
-
Clinical risk index for babies
- EDTA:
-
Ethylenediaminetetraacetic acid
- GA:
-
Gestational age
- HsPDA:
-
Hemodynamically significant patent ductus arteriosus
- IQR:
-
Interquartile range
- NEC:
-
Necrotizing enterocolitis
- NPV:
-
Negative predictive value
- NTproBNP:
-
N-terminal pro-brain natriuretic peptide
- PDA:
-
Patent ductus arteriosus
- PH:
-
Pulmonary hypertension
- PMA:
-
Postmenstrual age
- PPV:
-
Positive predictive value
- ROC:
-
Receiver operator curve
- ROP:
-
Retinopathy of prematurity
- SD:
-
Standard deviation
- Se:
-
Sensitivity
- Sp:
-
Specificity
- VLBWI:
-
Very low birth weight infants
References
Jensen EA, Schmidt B (2014) Epidemiology of bronchopulmonary dysplasia. Birth Defects Res. A Clin. Mol. Teratol 100(3):145–157. https://doi.org/10.1002/bdra.23235
Carraro S, Filippone M, Da Dalt L, Ferraro V, Maretti M, Bressan S et al (2013) Bronchopulmonary dysplasia: the earliest and perhaps the longest lasting obstructive lung disease in humans. Early Hum Dev 89(Suppl 3):S3–S5. https://doi.org/10.1016/j.earlhumdev.2013.07.015
Berkelhamer SK, Mestan KK, Steinhorn RH (2013) Pulmonary hypertension in bronchopulmonary dysplasia. Semin Perinatol 37(2):124–131. https://doi.org/10.1053/j.semperi.2013.01.009
Lenz AM (2011) Natriuretic peptides in children. Curr Opin Pediatr 23(4):452–459
König K, Guy KJ, Walsh G, Drew SM, Barfield CP (2016) Association of BNP, NTproBNP, and early postnatal pulmonary hypertension in very preterm infants. Pediatr Pulmonol 51(8):820–824. https://doi.org/10.1002/ppul.23391
Reynolds EW, Ellington JG, Vranicar M, Bada HS (2004) Brain-type natriuretic peptide in the diagnosis and Management of Persistent Pulmonary Hypertension of the newborn. Pediatrics 114(5):1297–1304. https://doi.org/10.1542/peds.2004-0525
Markovic-Sovtic G, Kosutic J, Jankovic B, Bojanin D, Sovtic A, Radojicic Z, Rakonjac MZ (2014) N-terminal pro-brain natriuretic peptide in the assessment of respiratory distress in term neonates. Pediatr Int 56(3):373–377. https://doi.org/10.1111/ped.12258
Snoek KG, Kraemer US, ten Kate CA, Greenough A, van Heijst A, Capolupo I, Schaible T, van Rosmalen J, Wijnen RM, Reiss IKM, Tibboel D (2016) High-sensitivity troponin T and N-terminal pro-brain natriuretic peptide in prediction of outcome in congenital diaphragmatic hernia: results from a multicenter, randomized controlled trial. J Pediatr 173:245–249.e4. https://doi.org/10.1016/j.jpeds.2016.03.026
Harris SL, More K, Dixon B, Troughton R, Pemberton C, Horwood J, Ellis N, Austin N (2018) Factors affecting N-terminal pro-B-type natriuretic peptide levels in preterm infants and use in determination of haemodynamic significance of patent ductus arteriosus. Eur J Pediatr 177(4):521–532. https://doi.org/10.1007/s00431-018-3089-y
Kulkarni M, Gokulakrishnan G, Price J, Fernandes CJ, Leeflang M, Pammi M (2015) Diagnosing significant PDA using natriuretic peptides in preterm neonates: a systematic review. Pediatrics 135(2):e510–e525. https://doi.org/10.1542/peds.2014-1995
Joseph L, Nir A, Hammerman C, Goldberg S, Ben Shalom E, Picard E (2010) N-terminal pro-B-type natriuretic peptide as a marker of bronchopulmonary dysplasia in premature infants. Am J Perinatol 27(05):381–386. https://doi.org/10.1055/s-0029-1243312
Kalra VK, Aggarwal S, Arora P, Natarajan G (2014) B-type natriuretic peptide levels in preterm neonates with bronchopulmonary dysplasia: a marker of severity? Pediatr Pulmonol 49(11):1106–1111. https://doi.org/10.1002/ppul.22942
Montgomery AM, Bazzy-Asaad A, Asnes JD, Bizzarro MJ, Ehrenkranz RA, Weismann CG (2016) Biochemical screening for pulmonary hypertension in preterm infants with bronchopulmonary dysplasia. Neonatology 109(3):190–194. https://doi.org/10.1159/000442043
König K, Guy KJ, Nold-Petry CA, Barfield CP, Walsh G, Drew SM, Veldman A, Nold MF, Casalaz DM (2016) BNP, troponin I, and YKL-40 as screening markers in extremely preterm infants at risk for pulmonary hypertension associated with bronchopulmonary dysplasia. Am J Physiol Lung Cell Mol Physiol 311(6):L1076–L1081. https://doi.org/10.1152/ajplung.00344.2016
Montaner A, Pinillos R, Galve Z, Boix H, de la cuesta C, Jimenez L, Samper P, Rite S (2017) Brain natriuretic Propeptide as an early marker of bronchopulmonary dysplasia or death in the preterm newborn. Klin Pädiatrie 229(04):223–228. https://doi.org/10.1055/s-0043-111597
Sellmer A, Hjortdal VE, Bjerre JV, Schmidt MR, McNamara PJ, Bech BH et al (2015) N-terminal pro-B type natriuretic peptide as a marker of bronchopulmonary dysplasia or death in very preterm neonates: a cohort study. PLoS One 10(10):e0140079. https://doi.org/10.1371/journal.pone.0140079
Mannarino S, Garofoli F, Mongini E, Cerbo RM, Codazzi AC, Tzialla C, Mazzucchelli I, Perotti G, Tinelli C, de Silvestri A, Manzoni P, Stronati M (2010) BNP concentrations and cardiovascular adaptation in preterm and fullterm newborn infants. Early Hum Dev 86(5):295–298. https://doi.org/10.1016/j.earlhumdev.2010.04.003
Mir TS, Laux R, Hellwege HH, Liedke B, Heinze C, von Buelow H, Läer S, Weil J (2003) Plasma concentrations of aminoterminal pro atrial natriuretic peptide and aminoterminal pro brain natriuretic peptide in healthy neonates: marked and rapid increase after birth. Pediatrics 112(4):896–899. https://doi.org/10.1542/peds.112.4.896
The CRIB (clinical risk index for babies) score: a tool for assessing initial neonatal risk and comparing performance of neonatal intensive care units (1993) The International Neonatal Network. Lancet 342:193–198. https://doi.org/10.1016/0140-6736(93)92296-6
Jobe AH, Bancalari E (2001) Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163(7):1723–1729. https://doi.org/10.1164/ajrccm.163.7.2011060
Walsh MC, Wilson-Costello D, Zadell A, Newman N, Fanaroff A (2003) Safety, reliability, and validity of a physiologic definition of bronchopulmonary dysplasia. J Perinatol 23(6):451–456. https://doi.org/10.1038/sj.jp.7210963
Mertens L, Seri I, Marek J, Arlettaz R, Barker P, McNamara P, Moon-Grady AJ, Coon PD, Noori S, Simpson J, Lai WW, Writing Group of the American Society of Echocardiography (ASE), European Association of Echocardiography (EAE), Association for European Pediatric Cardiologists (AEPC) (2011) Targeted neonatal echocardiography in the neonatal intensive care unit: practice guidelines and recommendations for training. Eur J Echocardiogr 12(10):715–736. https://doi.org/10.1093/ejechocard/jer181
Liu X (2012) Classification accuracy and cut point selection. Stat Med 31(23):2676–2686
El-Khuffash A, Davis PG, Walsh K, Molloy EJ (2008) Cardiac troponin T and N-terminal-pro-B type natriuretic peptide reflect myocardial function in preterm infants. J Perinatol 28(7):482–486. https://doi.org/10.1038/jp.2008.21
König K, Guy KJ, Walsh G, Drew SM, Watkins A, Barfield CP (2014) The relationship between BNP, NTproBNP and echocardiographic measurements of systemic blood flow in very preterm infants. J Perinatol 34(4):296–300. https://doi.org/10.1038/jp.2014.2
Dasgupta S, Aly AM, Malloy MH, Okorodudu AO, Jain SK (2018) NTproBNP as a surrogate biomarker for early screening of pulmonary hypertension in preterm infants with bronchopulmonary dysplasia. J Perinatol 38(9):1252–1259. https://doi.org/10.1038/s41372-018-0164-1
Da Graca RL, Hassinger DC, Flynn PA, Sison CP, Nesin M, Auld PAM (2006) Longitudinal changes of brain-type natriuretic peptide in preterm neonates. Pediatrics 117(6):2183–2189. https://doi.org/10.1542/peds.2005-1387
Author information
Authors and Affiliations
Contributions
PMA: Concept/design, Data analysis/interpretation, Drafting article, Approval of article, Data collection
PZR: Concept/design, Data analysis/interpretation, Drafting article, Approval of article, Data collection
SLL: Concept/design, Critical revision of article, Approval of article
IBF: Concept/design, Data analysis/interpretation, Critical revision of article, Approval of article, Statistics
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Patrick Van Reempts
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Méndez-Abad, P., Zafra-Rodríguez, P., Lubián-López, S. et al. NTproBNP is a useful early biomarker of bronchopulmonary dysplasia in very low birth weight infants. Eur J Pediatr 178, 755–761 (2019). https://doi.org/10.1007/s00431-019-03347-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03347-2