Abstract
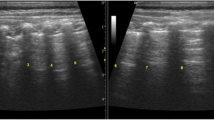
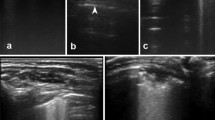
Bronchiolitis is the most common cause of hospitalization of children in the first year of life. The lung ultrasound is a new diagnostic tool which is inexpensive, non-invasive, rapid, and easily repeatable. Our prospective study was conducted in the emergency department and all patients underwent a routine clinical evaluation and lung ultrasound by the pediatricians who defined the clinical and the ultrasound score. We enrolled 76 infants (median age 90 days [IQR 62–183], 53.9% males). In nasopharyngeal aspirates, the respiratory syncytial virus was isolated in 33 patients. Considering the clinical score, children with higher score had a higher probability of requiring respiratory support (p 0.001). At the ultrasound evaluation, there was a significant difference on ultrasound score between those who will need respiratory support or not (p 0.003). Infants who needed ventilation with helmet continuous positive airway pressure had a more severe ultrasound score (p 0.028) and clinical score (p 0.004), if compared with those who did not need it.
Conclusion: Our study shows that lung ultrasound in the bronchiolitis may be a useful method to be integrated with the clinical evaluation to better define the prognosis of the individual patient. Multicenter studies on larger populations are necessary to confirm our data.
What is Known: • Bronchiolitis is the main cause of lower respiratory tract infection in children younger than 24 months. • Ultrasound can evaluate the lung parenchyma without ionizing radiations. | |
What is New: • Lung ultrasound may be a useful diagnostic tool to define the prognosis of the infants affected by bronchiolitis if performed at the first assessment in the emergency department. • The score obtained at the ultrasound evaluation is higher in those who will need oxygen therapy during admission for more time and in those who will need respiratory support with helmet continuous positive airway pressure. |







Similar content being viewed by others
Abbreviations
- ANOVA:
-
Analysis of variance
- AAP:
-
American Academy of Pediatrics
- ED:
-
Emergency department
- HCPAP:
-
Helmet continuous positive airway pressure
- HFNC:
-
High-flow nasal cannula
- IQR:
-
Interquartile range
- LUS:
-
Lung ultrasound
- NICE:
-
National Institute for Health and Care Excellence
- PICU:
-
Pediatric intensive care unit
- POCUS:
-
Point-of-care ultrasound
- RSV:
-
Respiratory syncytial virus
- SaO2 :
-
Hemoglobin oxygen saturation
- SD:
-
Standard deviation
- SPSS:
-
Statistical Package for the Social Science
References
Buonsenso D, Supino MC, Giglioni E, Battaglia M, Mesturino A, Scateni S, Scialanga B, Reale A, Musolino AMC (2018) Point of care diaphragm ultrasound in infants with bronchiolitis: a prospective study. Pediatr Pulmonol 53(6):778–786. https://doi.org/10.1002/ppul.23993
Caffrey Osvald E, Clarke JR (2016) NICE clinical guideline: bronchiolitis in children. Arch Dis Child Educ Pract Ed 101:46–48. https://doi.org/10.1136/archdischild-2015-309156
Collins FS, Varmus H (2015) A new initiative on precision medicine. N Engl J Med 372(9):793–795. https://doi.org/10.1056/NEJMp1500523
Copetti R, Cattarossi L (2008) Ultrasound diagnosis of pneumonia in children. Radiol Med 113(2):190–198. https://doi.org/10.1007/s11547-008-0247-8
Copetti R, Cattarossi L, Macagno F, Violino M, Furlan R (2008) Lung ultrasound in respiratory distress syndrome: a useful tool for early diagnosis. Neonatology 94(1):52–59. https://doi.org/10.1159/000113059
Dietrich CF, Mathis G, Blaivas M, Volpicelli G, Seibel A, Atkinson NS, Cui XW, Mei F, Schreiber-Dietrich D, Yi D (2016) Lung artefacts and their use. Med Ultrason 18(4):488–499. https://doi.org/10.11152/mu-878
Ghazaly M, Nadel S (2018) Characteristics of children admitted to intensive care with acute bronchiolitis. Eur J Pediatr 177:913–920. https://doi.org/10.1007/s00431-018-3138-6
Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA Jr (2013) Trends in bronchiolitis hospitalizations in the United States, 2000-2009. Pediatrics 132(1):28–36. https://doi.org/10.1542/peds.2012-3877
Henderson J, Hilliard TN, Sherriff A, Stalker D, Al Shammari N, Thomas HM (2005) Hospitalization for RSV bronchiolitis before 12 months of age and subsequent asthma, atopy and wheeze: a longitudinal birth cohort study. Pediatr Allergy Immunol 16(5):386–392. https://doi.org/10.1111/j.1399-3038.2005.00298.x
Kessler D, Ng L, Tessaro M, Fischer J (2017) Precision medicine with point-of-care ultrasound: the future of personalized pediatric emergency care. Pediatr Emerg Care 33(3):206–209. https://doi.org/10.1097/PEC.0000000000001050
Mansbach JM, McAdam AJ, Clark S, Hain PD, Flood RG, Acholonu U, Camargo CA Jr (2008) Prospective multicenter study of the viral etiology of bronchiolitis in the emergency department. Acad Emerg Med 15(2):111–118. https://doi.org/10.1111/j.1553-2712.2007.00034.x
Marin JR, Lewiss RE (2015) Point-of-care ultrasonography by pediatric emergency medicine physicians. Pediatr Emerg Care 31:525. https://doi.org/10.1097/PEC.0000000000000492
Mecklin M, Heikkilä P, Korppi M (2018) The change in management of bronchiolitis in the intensive care unit between 2000 and 2015. Eur J Pediatr 177:1131–1137. https://doi.org/10.1007/s00431-018-3156-4
Medina A, Del Villar-Guerra P, Modesto I, Alapont V (2019) CPAP support should be considered as the first choice in severe bronchiolitis. Eur J Pediatr 178:119–120. https://doi.org/10.1007/s00431-018-3280-1
Meissner HC (2016) Viral bronchiolitis in children. N Engl J Med 374(1):62–72. https://doi.org/10.1056/NEJMra1413456
Miller EK, Gebretsadik T, Carroll KN, Dupont WD, Mohamed YA, Morin LL, Heil L, Minton PA, Woodward K, Liu Z, Hartert TV, Williams JV (2013) Viral etiologies of infant bronchiolitis, croup and upper respiratory illness during 4 consecutive years. Pediatr Infect Dis J 32(9):950–955. https://doi.org/10.1097/INF.0b013e31829b7e43
Øymar K, Skjerven HO, Mikalsen IB (2014) Acute bronchiolitis in infants, a review. Scand J Trauma Resusc Emerg Med 22(23). https://doi.org/10.1186/1757-7241-22-23
Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, Johnson DW, Light MJ, Maraqa NF, Mendonca EA, Phelan KJ, Zorc JJ, Stanko-Lopp D, Brown MA, Nathanson I, Rosenblum E, Sayles S 3rd, Hernandez-Cancio S (2014) American Academy of Pediatrics. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics 134(5):e1474–e1502. https://doi.org/10.1542/peds.2014-2742
Reali F, Sferrazza Papa GF, Carlucci P, Fracasso P, Di Marco F, Mandelli M, Soldi S, Riva E, Centanni S (2014) Can lung ultrasound replace chest radiography for the diagnosis of pneumonia in hospitalized children? Respiration 88(2):112–115. https://doi.org/10.1159/000362692
Rosenfield D, Kwan C, Fischer J (2015) Point-of-care ultrasound: an emerging technology in Canadian paediatrics. Paediatr Child Health 20:67–68
Seattle Children’s Hospital, 2011. Criteria and respiratory score. Publishing http://www.tecpedu.net/uploads/1/4/9/1/14912848/bronchiolitis_algorithm_1_1.pdf . Accessed 30 Sept 2018
Sigurs N, Aljassim F, Kjellman B, Robinson PD, Sigurbergsson F, Bjarnason R, Gustafsson PM (2010) Asthma and allergy patterns over 18 years after severe RSV bronchiolitis in the first year of life. Thorax 65(12):1045–1052. https://doi.org/10.1136/thx.2009.121582
Taveira M, Yousef N, Miatello J, Roy C, Claude C, Boutillier B, Dubois C, Pierre AF, Tissières P, Durand P (2018) Can a simple lung ultrasound score predict length of ventilation for infants with severe acute viral bronchiolitis? Arch Pediatr 25(2):112–117. https://doi.org/10.1016/j.arcped.2017.11.005
Tomà P, Granata C, Sperandeo M (2018) Diaphragm ultrasound in infants with bronchiolitis. Pediatr Pulmonol 53(9):1177–1178. https://doi.org/10.1002/ppul.24060
Zorc JJ, Hall CB (2010) Bronchiolitis: recent evidence on diagnosis and management. Pediatrics 125(2):342–349. https://doi.org/10.1542/peds.2009-2092
Acknowledgments
The authors are grateful to all the children and their parents, nurses, and physicians who helped to perform this study. We also thank Dr. Umberto Raucci (Bambino Gesù Children Hospital of Rome, Italy) for his excellent assistance.
Author information
Authors and Affiliations
Contributions
Conception and research design: M.C. Supino, D. Buonsenso, A.M. Musolino
Data collection: S. Scateni, M.A. Mesturino, C. Bock, A. Chiaretti
Data analysis and interpretation and drafting the article: A. Reale, B. Scialanga, E. Giglioni, M.C. Supino
Final approval of the article: all the authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study described has been carried out in accordance with the abovementioned standards and has been approved by the institutional ethic committee.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Mario Bianchetti
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Supino, M.C., Buonsenso, D., Scateni, S. et al. Point-of-care lung ultrasound in infants with bronchiolitis in the pediatric emergency department: a prospective study. Eur J Pediatr 178, 623–632 (2019). https://doi.org/10.1007/s00431-019-03335-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03335-6